When it struck near Kathmandu, Nepal, on April 25, 2015, the Gorkha earthquake mainshock registered a moment magnitude of 7.8 Mw, making it Nepal’s most severe natural disaster since the 1934 Nepal-Bihar earthquake, and caused major aftershocks that persisted for weeks. Reference Ambraseys and Douglas1,Reference Chaulagain, Gautam and Rodrigues2 It razed entire villages, killing more than 8800 people, injuring more than 23,000, and rendering hundreds of thousands homeless. Reference Bilham3,4 In its immediate aftermath, the international community mobilized to mitigate the crisis, and contributions of humanitarian aid came from around the world; however, postdisaster humanitarian aid has variable success at achieving its intended results. Reference Cook, Shrestha and Bo Htet5 Fostering disaster-response strategies that promote on-the-ground impact remains an important public health goal.
The international medical response to any natural disaster is confronted by innumerable challenges, both universal and locale-specific. Preeminent among these is the difficulty of identifying and achieving a utilitarian balance of equipping sufficient personnel with sufficient supplies to thereby maximize the efficiency and impact of the response. To meet that challenge in responding to the Gorkha earthquake, we used a hybrid approach in which 2 independent organizations, Empower Nepali Girls (ENG) and International Neurosurgical Children’s Association (INCA), each contributed complementary resources based on each organization’s strengths. Thus, ENG, having more continuous communication and on-the-ground knowledge of Nepal, predominantly contributed personnel, Reference Peleg6–Reference Platt, Gautam and Rupakhety8 while material medical supplies were predominantly contributed by INCA, with additional support provided by other donors. Using this hybrid approach enabled the organizations to achieve a greater combined impact than either organization could have realized on its own and additionally proved to be an efficient way to rapidly mobilize resources. This strategy may be a valuable model that other international organizations can replicate as they seek to respond to future natural disasters.
Two Independent Organizations With Complementary Resources
Empower Nepali Girls
The mission of ENG (http://www.empowernepaligirls.org/) is to support and empower neglected, marginalized, and at-risk Nepali girls and young women, especially those considered to be at highest risk of being forced into an early marriage, sold into sex slavery, or abandoned as orphans. ENG raises funds to assist and mentor select Nepali girls who are thought to have the greatest potential to transform their communities and their country but who are unable to attend school and consequently lack the opportunity to pursue future careers in medicine, engineering, business, teaching, and other professions. These Nepali girls and adolescent women—selected based on financial need, as well as academic potential and performance—are granted scholarships, mentoring, career guidance, and subsistence by the organization. The girls’ progress and welfare are carefully monitored by means of home and school visits that are conducted several times yearly, both by volunteer staff in Nepal and by an international team of volunteers. As of this writing, ENG has supported over 400 scholarship recipients; these Nepali girls and young women receive all the necessities they require, including uniforms, supplies, books, shoes, and paid fees.
International Neurosurgical Children’s Association
INCA (http://www.incachildren.org/) was founded with the primary goal of educating, equipping, and empowering neurosurgeons in developing regions of the world to provide lasting and sustainable neurosurgical interventions for impoverished children living in their cities. The organization offers assistance in the form of equipment, technical information, training, and surgical support to neurosurgical teams throughout the world. In practice, INCA’s neurosurgeons are deployed on targeted visits over several years to build or renovate international pediatric neurosurgical programs. Success in this endeavor is measured by 2 parameters: how rapidly the neurosurgical team becomes obsolete in the host country and the amount of donation dollars spent.
Establishment of an Acute Response Medical Team
To manage global response to disasters, the World Health Organization (WHO) created emergency medical teams—Acute Response Medical Teams (ARMT)—comprised of groups of medical personnel with documented qualifications that are officially registered with the WHO. These teams are then deployed after a disaster in official coordination with the government of the country in question.
We established an equivalent version of an ARMT comprised of select personnel from ENG and INCA. Interaction of the leadership of the Division of Pediatric Neurosurgery at UCSD–RCHSD (also in leadership positions in INCA) and ENG was coordinated by the primary author (D.M.L.). Specifically, the primary author was concurrently a member of ENG (with prior experience in Nepal) and the UCSD-RCHSD Neurosurgery Service. The UCSD-RCHSD Neurosurgery Service is the primary sponsor of INCA. The relationship between the 2 organizations was negotiated for this single mission. These efforts were not coordinated with any other teams from either the WHO or United Nations (UN) in Nepal.
Inclusion on our team was foremost determined by availability of continuous contact with ENG team members living in the Gorkha earthquake disaster region; team members were selected for their local knowledge and familiarity with the region. Given the acuity of the intervention in a complex landscape, an additional consideration for inclusion was having the capacity to work in that region. Final considerations included medical and psychological expertise with trauma response. The medical team thus consisted of a naval military corpsman (surgical assistant and hospital administrator from UCSD), a trauma nurse from UCSD, a trauma psychologist, a local hospitality worker responsible for the labeling and distribution of packages of antibiotics and other medications, 2 nurses who had been scholarship recipients of ENG, 2 translators, a primary Nepali guide who also served as a logistics supervisor, and 6 local porters who carried medical supplies, tents, and survival equipment that were distributed along the way. Almost all the equipment and supplies had been donated by various organizations and physicians in the United States.
Barriers to a Successful Natural Disaster Medical Response
Achieving successful public health interventions or effective medical responses to natural disasters invariably requires identifying and overcoming barriers to medical delivery or implementation, some of which may be generalizable to a variety of settings and natural disasters Reference Guha-Sapir and Scales9 but others of which are context-specific. The observations described here further elaborate previous efforts that have been made to identify several of the barriers that specifically impeded the Gorkha earthquake response. Reference Cook, Shrestha and Bo Htet5,Reference Lee10,Reference Hall, Lee and Cartwright11
Geography
The goal of the natural disaster medical response group from ENG and INCA (Figure 1) was to travel to rural areas in Nepal (Figure 2, top left) that had previously been considered inaccessible to both national and international medical teams. These regions, in addition to their poor accessibility, were simultaneously expected to be among the most devastated. Reference Adhikari, Bhandari and Neupane12–Reference Aryal, Acharya and Shrestha14 The most direct access to these areas was provided by helicopter, creating a logistical transport challenge for the medical relief effort. Reference Bilham3,Reference Cook, Shrestha and Bo Htet5,Reference Platt, Gautam and Rupakhety8 This challenge worsened further on Tuesday, May 12, 2015, when a United States UH-1Y Huey helicopter involved in the relief efforts crashed near Charikot, Nepal, killing all onboard. 15 Helicopter support for the relief efforts ceased 2 wk later, 16 further diminishing capability to travel to desolate locations by air. Reference Cook, Shrestha and Bo Htet5,Reference Gulland13 Many remote locations affected by the earthquake were subsequently either inaccessible or accessible principally on foot with the guidance of knowledgeable locals, the approach used by the ENG/INCA team, described below.

Figure 1. The 2015 Gorkha earthquake medical response team from ENG and INCA. Left, some members of the team arranged with supplies. Right, members of the group interacting with a Nepali girl (top) and preparing to welcome patients to an ENG/INCA health camp (bottom).

Figure 2. Distributing medical aid in Nepal in the aftermath of the Gorkha earthquake. Top left, poorly accessible rural areas of Nepal were expected to be among the most severely affected by the earthquake. Top right, coordinating with Nepali nurses to distribute medical supplies. Bottom, some devastated areas of the city of Kathmandu (left) resulted in displaced residents setting up encampments (right).
Resource Pipeline
When the organizations’ medical response team arrived on May 11, 2015, 2 wk after the initial earthquake, the tarmac at Kathmandu airport was congested with humanitarian aid that had arrived from all over the world, and neither customs nor immigration oversight were identifiable at the airport. Reference Cook, Shrestha and Bo Htet5 Emergent government transport restrictions, which sought to charge duties for all donations, resulted in stranded aircraft from militaries and support organizations from countries including India, Nepal, Pakistan, and the United States. Reference Gautam17 Side-stepping what was essentially a Nepali governmental embargo of medical equipment being brought into the country, Reference Cook, Shrestha and Bo Htet5 the ENG/INCA team received advance notice that baggage accompanying international commercial airline passengers was allowable without such scrutiny. INCA coordinated in advance the collection of medical supplies that would be useful in the disaster zone (see below). Only 2 bags were permitted per passenger, each weighing up to 45 pounds, but once the airline waved the fee for additional baggage, an additional 12 bags of medical supplies were brought.
It was this group’s experience—albeit similar to the experiences reported by others Reference Gautam17 —that, although numerous physicians and medical organizations were stationed throughout Nepal, few or none of these individuals or organizations (including formal nongovernmental organizations and other medical organizations) could access medical equipment or supplies. The lack of supplies increased concern regarding the spread of disease and, when combined with persistent and deadly aftershocks, Reference Adhikari, Gautam and Koirala18,Reference Mendoza, Ghosh and Karplus19 a concurrent monsoon, Reference Bilham3 and the complete devastation of certain regions, made venture to outlying villages, particularly at altitude, untenable. Unavoidably, the most severe consequences of this impaired access were borne by the most at-risk populations, namely children and the elderly, Reference Adhikari, Bhandari and Neupane12,Reference Wagle, Amnatsatsue and Adhikari20 and likewise severely affected the local hospitals and the wider community. Reference Wagle, Amnatsatsue and Adhikari20–Reference Giri, Risnes and Uleberg22 Only by using the local experience of the community-based members of ENG—with their interpersonal contacts and their knowledge of local geography—was the ENG/INCA team able to connect the medical supplies they had brought with the outlying communities and people in need.
Language
Although the language barrier presented multiple difficulties, the assistance of 2 Nepali Sherpas and a Nepali nurse, included among the ENG members, was sufficient to not only triage patients but also to package the various drugs and antibiotics into individual pediatric and adult doses for distribution (Figure 2, top right) in addition to providing verbal and written instructions in Nepali regarding their correct usage. Partnership with ENG, an organization deeply integrated in the local community, was ultimately critical to successful delivery of medical care.
Series of Acute Interventions, Supplies, and Chronic Issues and Future Engagement
Series of Acute Interventions
On May 11, 2015, the group arrived in Kathmandu (a summary of the timeline and location-specific impact are provided in Table 1) with supplies, which included antibiotics and other assorted medications (Table 2), intravenous fluids, dressings, bandages, splints, sutures, stethoscopes, blood pressure cuffs, oxygen-saturation finger probes, headlamps, and additional medical supplies to combat a myriad of other conceivable contingencies. The following day, couriers from ENG brought additional supplies into Kathmandu, including more pharmaceuticals, antibiotics, and medical supplies.
Table 1. Itinerary, Treatment, and Resources

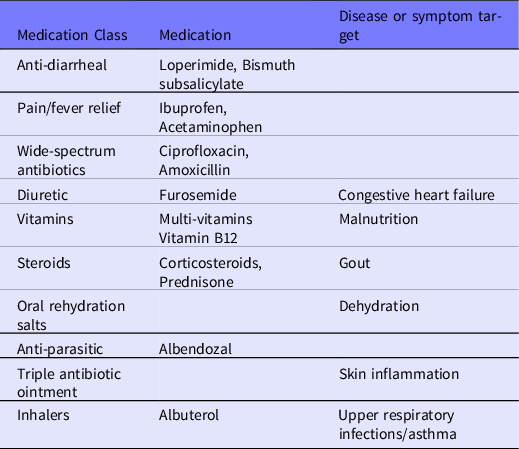
Table 2. Supplies for Chronic Illness
On May 12, 2015, the group traveled by bus to the ENG school in Kathmandu. Significant devastation was evident throughout the city with some people, having abandoned buildings and homes, living in makeshift tent cities (Figure 2, bottom left and right). The response team began treating children at the school but were forced to take a brief hiatus due to a 7.3 Mw aftershock, which originated east of the city in the Everest region. Reference Avouac, Meng and Wei23
On May 13, 2015, the team traveled throughout the most economically compromised neighborhoods in Kathmandu and set up a treatment center in a school room (Figure 3, top). The treatment center consisted of 2 clinics, 1 medical and the other for psychological trauma, a system the group subsequently replicated at each location.

Figure 3. Schools often served as makeshift clinics to provide medical care to local residents. Top, caring for patients in a temporary health camp set up in a school. Bottom left, less acute medical ailments such as earache become more common than trauma in the subacute to chronic aftermath of earthquakes. Bottom center and right, treatment for many children included counseling.
Earthquakes are often associated with a particular pattern of medical complications in which a preponderance of traumatic injuries in the acute aftermath of the disaster is subsequently followed by a subacute to chronic period of medical abnormalities resulting from impaired access to medical care. Reference Adhikari, Bhandari and Neupane12,Reference Aryal, Acharya and Shrestha14,Reference Bartels and Vanrooyen24 In accordance with this pattern, the primary medical issues the ENG/INCA team encountered included upper respiratory and gastrointestinal infections, sprains and fractures, intestinal parasites, foreign objects in ears, congestive heart failure, allergies, and psychosomatic issues including insomnia and panic (Figure 3, bottom left). Indeed, mental health issues were the most pronounced. Nearly everyone was experiencing symptoms of posttraumatic stress disorder, and depression and suicidal ideation were frequent. Behavioral regression was evident in the younger children, and the group ultimately provided psychological counseling to over 50 children throughout the duration of its deployment (Figure 3, bottom center and right).
On May 14, 2015, the group traveled to the Tenzing Hillary airport in Lukla, close to the origination of the major aftershock 2 d prior. From Lukla the group traversed through Phakding and onward to Monjo by means of the Himalaya trail. Along the Himalaya trail, given the overall lack of acute response, individuals were left to survive on their own, as no physicians or health professionals could be found. Damage from the aftershock was evident, as all of the structures between Phakding and Monjo were destroyed. Indeed, the persistence of intermittent major aftershocks (∼5-10 per d) discouraged sheltering in any infrastructure that remained, forcing the group to sleep outside despite the beginning of monsoon rains. Other than locals, the trail all the way to Monjo was empty of travelers (Figure 4, top left), and the trail itself was full of slides and fissures. Nearer the epicenter of the aftershock, many of the trails had been destroyed by landslides, requiring the group to find alternate routes. Lodging the next evening was provided by 1 of the accompanying Sherpas, with travel continuing the next day toward Namche Bazar, where another treatment clinic was hosted.

Figure 4. Only locals were encountered in isolated rural areas. Top left, the rugged terrain of the trail meant it was devoid of any travelers other than locals. Top center, patients were treated at makeshift health camps along the trail between villages. Bottom, map of Nepal; red circle identifies Kathmandu, and red box portrays inset region at right, near the focal origin of the 7.3 Mw aftershock on May 12. Right, inset region summarizing ENG/INCA group’s travel and treatment provided between May 14 and 17. Map used courtesy of © OpenStreetMap contributors (https://www.openstreetmap.org/copyright) under the Open Database License (https://opendatacommons.org/).
On May 15, 2015, the group traveled to Namche Bazar and set up a medical clinic in a small wooden school that was still structurally intact; the 1 clinic in the Everest region near the epicenter had been reduced to rubble. Numerous patients were treated, including a group of Nepali military medics who had been injured helicoptering into the valley, having been unwilling to traverse the path the group had used to get into the city. Similarly, the ENG/INCA group provided additional medical supplies to a Nepali military medic team that had reportedly exhausted their supplies 10 d prior.
On May 16, 2015, the group reverse-trekked its path back down into the valley, stopping at each village work or tent encampment to offer medical care to patients (Figure 4, top center).
On May 17, 2015, travel continued to Lukla, where 40 patients were treated in an abandoned German Red Cross tent. Furthermore, additional medical equipment was provided to a Swedish physician who was stationed at the medical clinic in Lukla (travel and treatment provided May 14-17 summarized in Figure 4, bottom and right), who said the ENG/INCA medical response team was the first he had seen to provide Western medical care in this region since the initial earthquake. No other nongovernmental organization (NGO) or health organization, government assistance, or foreign aid were present or available during the first mo after the earthquakes in any of the villages along the Himalaya trail with which we were familiar.
On May 18, 2015, the group returned to Kathmandu from Lukla and traveled to the Rising Ray School in Kathmandu to provide medical care.
On May 19, 2015, the group traveled to the 8th century city of Bhaktapur, a neighboring city of Kathmandu and the old capital of Nepal, to provide additional medical care. In total, during its week-long deployment, the medical response team from ENG and INCA was able to successfully provide care to 834 patients.
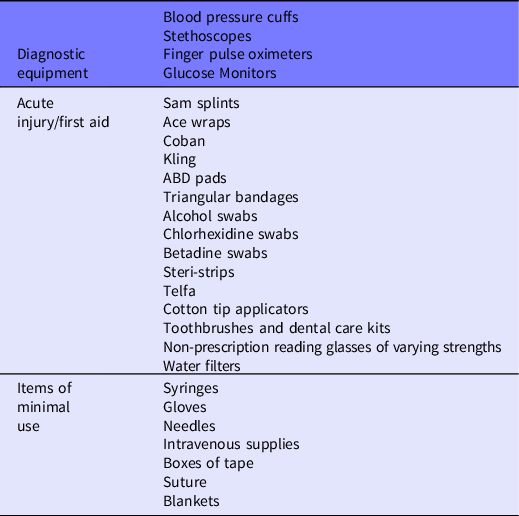
Supplies
The medical supplies that were brought along included 35-50 boxes (20 × 20 × 15” in size) filled with syringes, needles, dressings, alcohol preparations, saline vials, saline flushes, lactated ringers, scissors, forceps, and more (Table 3). A priority of the medications that would likely be most useful was determined by undertaking a prospective review of the United States Center for Disease Control’s Refugee Health Profile for Nepal and Bhutan. 25 In addition to medical care, psychological treatment was offered to care for trauma. Trauma was treated by group support sessions, individual consultations, and information packets distributed explaining the nature and process of traumatic stress.
Table 3. Other equipment and supplies
Chronic Issues and Future Engagement
Based upon the temporally dynamic pattern of medical issues associated with earthquakes and reports from medical personnel in Kathmandu immediately following the earthquake, Reference Aryal, Acharya and Shrestha14,Reference Bartels and Vanrooyen24 it was anticipated that the most frequently encountered injuries would not be acute in nature. This enabled the establishment of a secondary source of supplies and diagnostic equipment that would be directed toward injuries of a more chronic nature. Reference Bartels and Vanrooyen24 Many patients, for example, reported experiencing chronic or acute headaches precipitated by deteriorating eyesight. Likewise, the prominence of poor dental care was demonstrated by how frequently patients exhibited infected teeth and gums which, left untreated, can precipitate even more severe systemic issues. Most prominently noticeable was the need of treatment for mental illness, for which the availability of care is starkly absent.
To sustainably ameliorate these more chronic maladies, however, it will be necessary to marshal further effort and resources beyond acute disaster relief. Reference Aryal, Acharya and Shrestha14,Reference Bartels and Vanrooyen24 Although the treatment and trauma centers we established along our route were temporary, all of the medical and surgical supplies we brought into Nepal were given to locals before our departure. Given the acuity of the present mission, no formal follow-up was scheduled or envisioned. However, the ENG presence is so consistent—the ENG organization returns to this region every 6 to 12 mo—that follow-up encounters were inevitable in some cases. Nevertheless, the dearth of resources or health-care in the region in which we operated persists.
Discussion
Background
The UN has established a system of large overarching segments of humanitarian aid, referred to as clusters, each of which is intended to function globally, nationally, and locally. Reference Steets, Grünewald and Binder26 The WHO oversees the health cluster and thus manages everything from global-scale catastrophic prediction and health organization coordination to local health response implementation, in addition to coordination with other clusters. The foremost concern with the cluster system, as noted by the UN, Reference Steets, Grünewald and Binder26 is that its tendency to be overly top-down bureaucratically impedes the engagement of local players, hindering local implementation. To correct this shortcoming in the future, the UN’s recommendations are to:
‘…facilitate the participation of national and local NGOs and strengthen their capacities…by includ[ing] national and local NGOs in management and strategy development…Explore options for encouraging their participation…for example, by ensuring that more staff members have an appropriate understanding of the context and knowledge of the local situations’ (p. 83-84). Reference Steets, Grünewald and Binder26
The model described in this Concept, in which at least 1 partner organization is rooted in deep local knowledge of a region, is 1 method that may be able to close the gaps in the formal WHO health cluster system. Following the 2015 earthquake, coordinated response teams were absent in the numerous small outlying villages. However, these were the areas the ENG/INCA team had the greatest access to and in which it effected the greatest impact: Years of continuous involvement in this region facilitated understanding of it and helped to maximize local engagement.
Future
Seeking to apply the lessons learned during 1 natural disaster to improve the strategic response to another in the future must be a foremost operational goal of any medical response organization. Worryingly, updating our medical response strategies with lessons learned from the Gorkha earthquake response may prove particularly valuable given the region where the Gorkha earthquake hit. Nepal sits atop the geologic zone where the Indian and Eurasian plates tectonically converge, Reference Larson, Burgmann and Bilham27 and when the mainshock of the Gorkha earthquake struck northwest of Kathmandu along the prominent Main Himalayan Thrust fault, it subsequently propagated eastward, “unzipping” the fault. Reference Avouac, Meng and Wei23 Seismic modeling suggests earthquakes along the Main Himalayan Thrust fault cycle bimodally because of its friction and geometry: In this way, partial earthquakes (≤ Mw ∼7.8) transfer subsurface strain that was accumulated from tectonic convergence upward toward the surface, and this strain ultimately gets released by larger (∼Mw 8+), surface-rupturing great earthquakes, such as the 1934 Nepal-Bihar earthquake. Reference Dal Zilio, van Dinther and Gerya28,Reference Sapkota, Bollinger and Klinger29 Geophysicists believe the Gorkha earthquake dissipated below the surface along the fault, Reference Duputel, Vergne and Rivera30 thereby leaving a subsurface zone of accumulated stress near Kathmandu that will have to be released, most likely by means of a more severe earthquake an indeterminate number of years in the future. Reference Bilham3,Reference Mendoza, Ghosh and Karplus19,Reference Bilham31 In other words, belying its devastating effects, the Gorkha earthquake was probably not yet “the big one” that researchers have been predicting. Reference Bilham3,Reference Mendoza, Ghosh and Karplus19,Reference Bilham31 Consequently, applying successful methodologies from the Gorkha earthquake response to future natural disaster preparedness may be valuable not just for other yet unforeseen natural disasters but also perhaps for another, even more severe, earthquake predicted to strike the Nepali Himalayas.
To that end, previous efforts that sought to evaluate the international medical response to the Gorkha earthquake Reference Cook, Shrestha and Bo Htet5,Reference Amat Camacho, Karki and Subedi32–Reference Basu, Ghosh and Jana34 concluded that a critical goal for the future must continue to be the further training of locals in earthquake-prone areas, as they can be the most impactful, first in preparing for future natural disasters and then saving lives in the acute aftermath of an event. Reference Peleg6–Reference Platt, Gautam and Rupakhety8 Specific to Nepal, for example, it may be a plausible goal to train members of ENG in the use of wilderness diagnostic equipment, as outfitting them with it would prove to be an immediate “force multiplier” for Nepali public health going forward. Nevertheless, the hybrid approach reported here, in which international organizations meld complementary strengths with organizations that have on-the-ground expertise, proved to be an effective response strategy and one that other organizations may find helpful as a replicable model in seeking to increase the impact of medical responses to future natural disasters.
Recommendations for Hybrid Approaches
Both the benefits and difficulties for developing a hybrid approach to acute disasters in countries with minimal resources are related to the organizations’ experience and understanding of the region. Our experience following this effort supports the recommendation that consistent, accurate, and up-to-date information transfer is integral to the success of such interventions. Groups must have current and consistent communication with individuals or groups in the affected region as well as the ability to reach the destination in difficult circumstances. Given our continuous interactions with ENG team members in Nepal, for example, we were acutely aware of the extent of devastation present following the Gorkha earthquake. Initial inquiry disclosed the absence of any medical teams along the Himalaya trail, with minimal governmental presence in villages in response the disaster, signaling the need for a locally oriented response. Relying on local leaders for guidance and support ultimately proved critical for a successful response.
The significance of the involvement of the ENG organization in the present model is that it perfectly aligns with these criteria. ENG had years of involvement in the region affected by the Gorkha earthquake and with individuals in close proximity to the disaster, and this deep involvement was critical to increasing the response team’s access in the aftermath of the earthquake. It took many years and patience for ENG to earn credibility and the locals’ trust. Initially, male leaders attempted to control resources and earn goodwill for themselves until transition could be made to promoting volunteers and staff among the young women in the program, and the first children in the program are now helping run the organization. Multiple visits per year to individuals in each village developed profound local knowledge, relationships, and trust of the organization within the communities. In addition to just going to visit, ENG also brought desperately needed resources during visits, including teaching and school supplies, athletic equipment, medical supplies, English instruction, and academic scholarships for the children in greatest need. ENG set up regular health screenings and health clinics in villages as a way to get to know the families and provided consulting and instructional programs for educators and health professionals. It also facilitated access to couriers and organizational personnel that was essential to the mission. These capabilities were absent in INCA despite its decades of experience in surgical missions throughout the world. INCA, by contrast, was well versed in procuring the requisite medications, medical, surgical, and educational supplies to provide medical care in developing countries. INCA’s experience was less with emergent disaster response and more tailored to the development of facilities in areas with a paucity of resources. Meanwhile, these capabilities were absent in ENG despite decades of experience in missions to Nepal.
The primary considerations in a hybrid response are to provide acute, emergent care at an effective level that could not be achieved absent any of the component organizations, whether it be 2 or more. The organizations involved should have a history of significant impact based upon their historic goals, and the potential impact should be much greater than the simple combination of the multiple organizational components of a hybrid model. Moreover, the ideal, most suitable organizations are those with a deep historic presence in the region involved and those that historically are able to rapidly obtain the requisite medical supplies necessary for the success of the mission. This approach should predict the most success in acute responses to disasters, success that has the potential to exceed that of the current cluster approach in acute settings.
With better recognition of this approach, the UN/WHO can initiate a resource site that delineates the organizations willing to be involved in acute responses and their potential contributions. Using such a prospective approach, the determination of which organizations can contribute to a successful response and the initiation of communication between them can be made both simplistic and reproducible. This can only become more systematic when integrated into the umbrella of senior organizations.
Limitations
The conclusions we can recommend from this hybrid approach to natural disaster response are necessarily subject to limitations. One limitation is that this, our Gorkha earthquake response, is our first application of this model to a natural disaster, and it is conceivable that this approach may be less effective in other contexts. Because this approach relies on the joint application of organizations’ inherent capabilities, we expect it will be readily generalizable to other emergent medical responses. Indeed, our approach is fundamentally rooted in the public health model of community-based intervention, which has demonstrated efficacy in a variety of contexts and health conditions. Reference McLeroy, Norton and Kegler35–Reference Roussos and Fawcett37 Nevertheless, further evaluation will be necessary to validate the efficacy of this model in responding to other types of disasters. A second limitation is the timing of the response. Although the subacute response timing described herein bolstered the ability of these organizations to respond impactfully (eg, predictive tailoring of medical supplies, side-stepping prohibitive regulations, etc.), future disasters may demand responses in which timing is more restrictive. Future evaluation of this hybrid approach in settings requiring more acute or more delayed medical response timing is an important next step. A third limitation of our approach is that individual organizations risk duplicating efforts and inefficiently using local resources if inter-organizational communication is inadequate during preparation of a natural disaster response. The future impact of this limitation could be reduced by means of the aforementioned establishment by the UN/WHO of a resource site listing willing organizations and their potential contributions. Such a site would promote strategic inter-organizational communication and reduce redundant efforts, thereby bolstering disaster response efficiency.
Conclusions
The 2015 Gorkha earthquake was Nepal’s most severe natural disaster since the 1934 Nepal-Bihar earthquake, killing or injuring tens of thousands and displacing hundreds of thousands, and caused major aftershocks that lasted for weeks afterward. Two international partner organizations, ENG and INCA, coordinated the complementary resources of material medical supplies and human capital with locale-specific knowledge to reach rural and other poorly accessible areas of Nepal and treat nearly 1000 patients, a much greater medical response impact than would have been achievable had either organization mobilized alone. Although innumerable barriers confront the medical response to any natural disaster, a hybrid approach in which 2 organizations—optimally with at least 1 of the pair having on-the-ground knowledge—merge complementary strengths can be an effective strategy to deploy critical resources to poorly accessible areas and thereby maximize their impact. This hybrid model may be acutely valuable should another severe earthquake strike Nepal, the chance of which is rendered inevitable at some point by Nepal’s geologic position. Critically, however, this medical response strategy is easily tailorable and scalable to other natural disaster contexts by other medical relief organizations. Preemptive coordination between partner organizations with complementary strengths may further enhance the medical impact that can be achievable by international organizations responding to the next natural disaster.
Acknowledgments
The authors acknowledge the resources and support of Rady Children’s Hospital (RCHSD), San Diego, CA, particularly individual support from Matthew Parker and Monet Solberg. From Empower Nepali Girls, we acknowledge critical support from Pasang Temba Sherpa, Chhusang Sherpa, and Pema Sherpa, without whom the mission could not have achieved success.
Author contributions
D.M.L, J.K., and M.L.L. were critical to the implementation of the concept. D.M.L. and J.W.A. drafted the manuscript with input from all authors. The concept was overseen by J.K., J.R.C., and M.L.L.
Conflict of interest
None











