The findings from a longitudinal study of parenting by mothers with eating disorders (Stein et al, Reference Stein, Woolley and Cooper1994, Reference Stein, Murray and Cooper1996) suggest that intrusive and conflictual parenting, especially in the context of mealtimes, might be important in the intergenerational transmission of food-related disorders. If such a process were to operate, it is uncertain whether it would obtain only in cases of clinical severity, or whether a similar process might operate across a range of disturbance. We aimed to address these issues by examining, in a community sample, the role of the mother-child relationship in mediating the association between maternal eating disorder psychopathology and child feeding problems. Based on the limited amount of previous research, our hypothesis was that high levels of maternal eating disorder psychopathology would be related to specific disturbances in the quality of the mother-child relationship, that both the maternal eating disorder and the relationship disturbances would be related to the level of child feeding problems, and that mother-child relationship variables would mediate the association between maternal and child disturbance.
METHOD
Sampling
Pre-schools within the Reading area provided the base population for the study (see Wheland & Cooper, 2000). The mothers were asked to complete a self-report version of the Behaviour Screening Questionnaire (BSQ; Reference Richman and GrahamRichman & Graham, 1971), together with a questionnaire on child shyness (Reference Stevenson-Hinde and GloverStevenson-Hinde & Glover, 1996). The teachers completed the Pre-school Behaviour Checklist (PBCL; Reference McGuire and RichmanMcGuire & Richman, 1986) for all the children. Children with feeding problems were identified on the basis of maternal BSQ responses from ten schools. Of the 722 questionnaires sent out, 462 were returned satisfactorily completed by the mothers (64%). From these questionnaires, 56 children whose home language was English were identified as having a significant feeding problem. In 7 cases the mother could not be contacted (no telephone or wrong address), and 6 mothers refused to take further part in the study. The remaining 43 children were assessed. The mother of one of them reported at interview that the feeding problem had remitted some months previously; this child was excluded, and the remaining 42 children formed the ‘feeding problems’ sample.
Two comparison samples were identified for further study (from the same ten schools, plus two further schools). First, out of the full sample of 578 completed BSQs (out of a possible 867), a random sample of 1 in 10 (i.e. 44) of those who fulfilled criteria for a normal control sample (i.e. no marked feeding problem, fearfulness, shyness or behavioural disturbance) was selected for further study: 5 mothers could not be contacted (no telephone or wrong address) and 10 refused to take part in the study. The remaining 29 children were assessed, and formed the ‘normal’ control subgroup of this study. Second, a ‘disturbed’ comparison sample was identified: this comprised children who had no reported feeding problem, but who were reported to be fearful (three or more marked fears, or six or more mild fears on the BSQ or the PBCL), shy (mean score of 4.0 or more on the child shyness questionnaire) or to have significant behavioural disturbance (score of at least 10 on the BSQ or 12 on the PBCL, together with marked disturbance in at least one of the key areas of disturbance), or any combination of these three categories. A total of 95 English-speaking children fulfilled these criteria and were selected for further study: 10 mothers could not be contacted (no telephone or wrong address) and 6 refused to take part in the study, leaving 79 children in the ‘disturbed’ subgroup.
Maternal assessment
The mothers and children were assessed on two separate occasions in their own homes. A combination of interview, questionnaire and systematic observational measures was used. The eating behaviour of all the children was assessed by maternal interview, using the Feeding Problems and Eating Disorders Interview Schedule (Reference Harris, Booth, Cooper and SteinHarris & Booth, 1992), a reliable and valid method of assessing child feeding problems. In all the cases of feeding problems identified by the mother on the BSQ (bar the one excluded case referred to above), the feeding disturbance was confirmed at this interview. Furthermore, although in some of the children in the two comparison groups disturbances in feeding of a minor nature were identified by this interview, in no case did this approach the severity found in those within the feeding problems group. In addition to this interview, a family meal was filmed and rated (see below).
Two additional standardised interviews were used to assess the mothers: the Eating Disorder Examination (EDE; Reference Cooper, Cooper and FairburnCooper et al, 1989), which provides a detailed assessment of eating habits and attitudes (and a self-reported account of height and weight), and the Anxiety Disorders Interview Schedule (Reference Brown, DiNardo and BarlowBrown et al, 1994), which provides an assessment of DSM-IV anxiety and depressive disorders (American Psychiatric Association, 1994). For both measures an assessment of current state was made, as well as an assessment of lifetime psychiatric history. For each woman interviewed, DSM-IV diagnoses were made by the interviewer in consultation with one of the authors (P.J.C.). The rates of current and past DSM-IV Axis I disorders among the mothers of the three groups of children in this study have been reported in an earlier paper (Reference Whelan and CooperWhelan & Cooper, 2000). Three interviewers carried out the maternal mental state assessment masked to child status; in a few cases this could not be completed. The following results concern the sub-sample of 116 mother-child pairs for whom full maternal mental state and observational data were available: 35 from the feeding problems sample, 58 from the disturbed sample and 23 from the normal sample.
Observational assessment
The mealtime observations served two purposes: the first was to validate the children's assignment to the feeding problem category, and the second was to investigate the nature of the mother-child relationship in the context of child feeding. The mothers were asked to give their child their normal midday meal, and if the two normally ate together, then to do that also. The meal was recorded by video camera, with the researcher in another room to allow the participants to behave naturally. The mother was asked to call the researcher when the meal finished so that filming could be stopped. The children's mealtime behaviour was then coded (with the assessor masked to child group and maternal mental state), according to a system based upon items drawn from the Feeding Problems and Eating Disorders Interview Schedule: food refusal, faddiness, amount eaten and eating behaviour (e.g. spitting).
The filmed meal was also used to rate maternal management style. Six items relating to the environment and management of the child's mealtime were selected in order to assess the specific dimension of mealtime disorganisation: these items were location (kitchen or dining room), disposition (table and chair), presence of mother, mother eating with the child, child eating with siblings, and distractibility (e.g. watching television or play with toys). These six items were aggregated to form a single scale, which had adequate internal consistency (α=0.63).
In addition, the mothers and children were filmed interacting in a situation unrelated to eating: this was a task in which the children were instructed to explore the contents of a box, under conditions of apprehension, and the mother was instructed to assist them. A coding system was devised to assess the degree of strong maternal control and disharmony (Stein et al, Reference Stein, Woolley and Cooper1994, Reference Stein, Murray and Cooper1996). An index was derived by aggregating the standardised (z) scores of three variables: physical interventions, strong verbal directives and overall level of disharmony. Again, ratings were made masked to both child group and maternal psychiatric history. This index also had adequate internal consistency (α=0.66).
Statistical analyses
Path analytic techniques were employed to investigate the potential mediating role of the mother-child relationship variables (mealtime disorganisation and strong control/disharmony) in the association between maternal eating disorder psychopathology and child feeding problems. The data were modelled using the M-plus software package (Reference Muthen and MuthenMuthen & Muthen, 1998) using weighted least squares estimation with robust standard errors and assessed with the mean and variance adjusted chi-squared statistic. This modelling technique allows analyses to be conducted using categorical variables, and the use of robust estimators gives reliable estimations when the variable distributions are skewed and sample sizes are small (Reference Bentler and YuanBentler & Yuan, 1999). With the use of robust estimators, it is not possible to test the suitability of different models using the conventional approach of χ2 difference testing; thus models were compared according to other model fit indices, specifically the root mean square error of approximation (RMSEA), the comparative fit index (CFI) and the non-normed fit index (NNFI). For the RMSEA, values below 0.08 indicate a satisfactory fit and values below 0.05 indicate an excellent fit. For both the CFI and the NNFI, values above 0.95 indicate a satisfactory fit.
RESULTS
Sample characteristics
The mean age of the children with feeding problems was 55.4 months (s.d.=4.37), similar to that of those from the disturbed comparison group (56.3 months, s.d.=4.17) and the control group (57.0 months, s.d.=3.93; F (2,124)=0.47). Of the feeding problems group 44% were first-born children, compared with the same proportion in the disturbed comparison group and 35% of the normal controls (χ2=0.77, d.f.=2); and 13% of the feeding problems group were only children, compared with 10% of the disturbed comparison group and 4% of the normal controls (χ2=1.48, d.f.=2). In the feeding problems group 43% were girls, compared with 48% of the disturbed comparison group and exactly half of the normal controls (χ2=0.42, d.f.=2). The groups also did not differ with respect to social class distribution. When class was considered in two broad categories (upper/middle and working class), 51% of the feeding problem group came from the lower class category, compared with 40% of the disturbed comparison group and 39% of the control group (χ2=1.48, d.f.=2). The great majority of the mothers were either married or cohabiting (87%, 86% and 96% for the feeding problems, disturbed and normal groups, respectively;χ2=2.00, d.f.=2). The maternal body weights at assessment were equivalent for the three groups (for mean body mass index, F (2,112)=0.64). The age distributions of the women in the three groups were also extremely similar: the mean age for mothers of the children with feeding problems was 31.8 years (s.d.=4.72), for mothers of those in the disturbed comparison sample it was 32.2 years (s.d.=5.50) and for mothers of the healthy controls it was 32.3 years (s.d.=5.12; F (2,125)=0.84).
Validation of the presence of feeding problems
Because membership of the feeding problems group was based entirely on mothers’ reports on the BSQ of their child's problems, the possibility had to be considered that the reporting of child faddiness or appetite disturbance was a factitious projection made by the mothers rather than a feature of the children themselves. If such projection were systematically related to maternal eating disorder psychopathology, then any relationship found between child and maternal disturbance would be spurious, and the search for mediators would be folly. To eliminate this possibility, child behaviour during the filmed family meal was rated masked to both child group and maternal mental state. On the index of child feeding disturbance, the children in the feeding problems group were rated as significantly more disturbed than both the disturbed comparison children and the normal control children (χ2=20.6, d.f.=2, P<0.05 on post hoc tests for both comparisons). Furthermore, for the whole group of children, there was a strong relationship between the degree of feeding disturbance reported by the mother on the BSQ (using the ordinal scale described above) and the degree of disturbance in feeding evidenced by the child at the filmed meal (r=0.51, P<0.001). Notably, this relationship between maternally reported and independently observed child feeding disturbance was unrelated to the level of eating disorder psychopathology in the mother. Compared with the simple correlation between reported and observed child feeding problems, the partial correlation coefficient, controlling for the effect of current maternal EDE total score, was minimally changed (at 0.46); and controlling for maternal DSM-IV eating disorder history, the decrease was nugatory (i.e. from 0.51 to 0.48). These findings indicate that maternal reports of child feeding disturbance were unrelated to eating disorder psychopathology in the mother, and that the group of children identified by their mothers as having feeding problems did indeed have disturbed eating patterns.
Observational measures
The three study groups were compared on the two indices of the mother-child relationship: mealtime disorganisation (Fig. 1) and strong control/disharmony (Fig. 2). On both indices, ratings were significantly higher for the feeding problems group than for the other two groups (F (2,113)=9.88, P<0.001 and F (2,113)=7.26, P<0.001 respectively), with post hoctests indicating that the feeding problems group was significantly different from the other two groups (and that the other two groups were no different from each other).
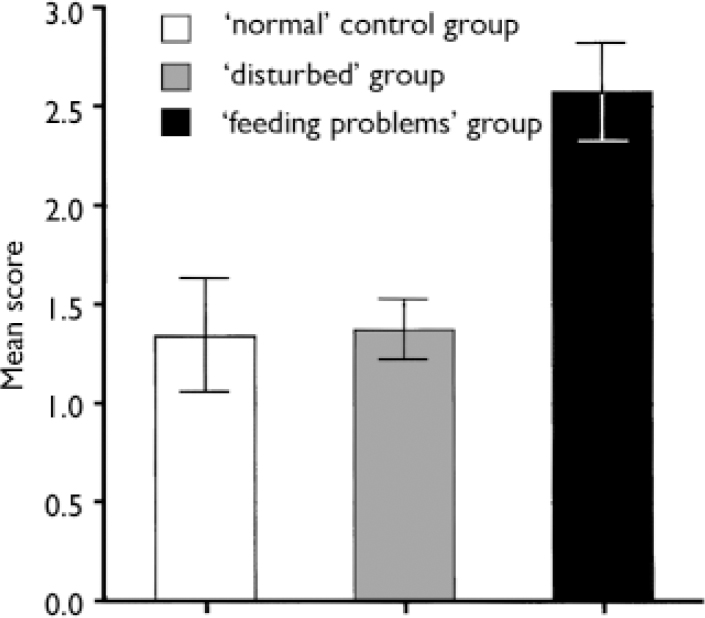
Fig. 1 Mealtime disorganisation: mean scores (1 standard error of the mean) for the three groups of children.
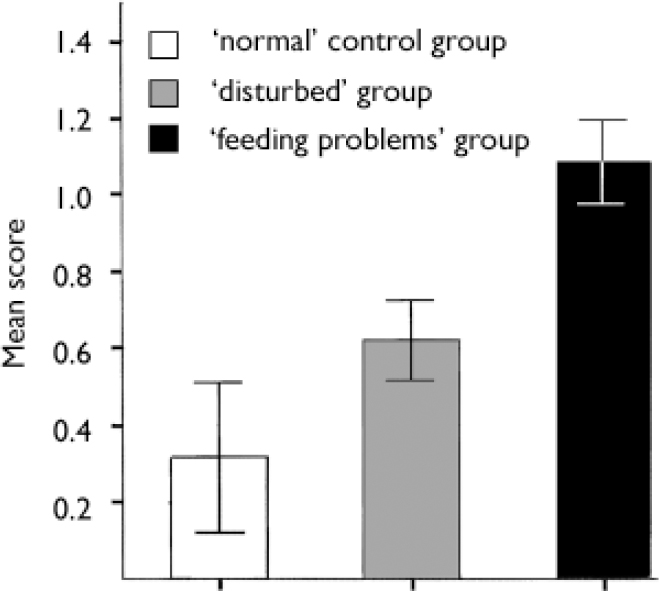
Fig. 2 Strong maternal control or disharmony: mean scores (1 standard error of the mean) for the three groups of children.
Path analysis
A child feeding problems variable was derived from the two relevant BSQ items and applied to the full sample of 116 children. This four-point ordinal scale corresponded to ‘no problems’ (score of 0 on both BSQ items), ‘minor problems’ (of 1 on either or both BSQ items), ‘moderate problems’ (score of 2 on one of the two BSQ items) and ‘marked problems’ (a score of 2 on both BSQ items). The number of children within each level was 44 (no problem), 36 (minor problem), 23 (moderate problem) and 13 (marked problem). The path analysis included only those children for whom complete data were available on the four critical variables: level of child feeding disturbance, current and past maternal eating disorder, mealtime disorganisation and maternal strong control/disharmony. This produced a sample of 116 children: 35 from the feeding problems group, 58 from the disturbed group and 23 from the normal control group.
Table 1 shows the univariate correlation matrix between the four critical variables. As hypothesised, both the presence of current maternal eating disorder psychopathology (i.e. EDE total score) and the two mother-child relationship variables were significantly associated with the extent of the feeding problem in the child. In addition, the two relationship variables were also significantly associated with the level of maternal eating disorder psychopathology. In order to investigate whether the mother-child relationship variables mediated the relationship between maternal eating disorder psychopathology and child feeding problems, a path analysis was conducted. A model was specified in which child feeding problems were predicted by the severity of current maternal eating disorder psychopathology, mealtime disorganisation and maternal strong control/ disharmony; and both mealtime disorganisation and maternal strong control/disharmony were predicted by the severity of maternal eating disorder psychopathology. This model provided a satisfactory level of fit according to all three model fit indices: χ2=0.55, d.f.=1, P=0.485; RMSEA=0.062, CFI=0.989, NNFI=0.960 (Fig. 3). In contrast to the univariate direct relationship between maternal eating disorder psychopathology and child feeding problems, the multivariate analysis showed that this direct pathway was no longer significant. It therefore appeared that the two mother-child relationship variables fully mediated the continuity between maternal eating disorder psychopathology and child feeding problems. Furthermore, when this mediational model was tested explicitly by fixing the direct pathway to zero and rerunning the analysis, the model fit indices showed additional improvement: χ2=1.421, d.f.=2, P=0.488; RMSEA=0.049; CFI=0.990; NNFI=0.974. Specifically, the RMSEA fell below the critical cut-off value of 0.05 for an excellent fit.
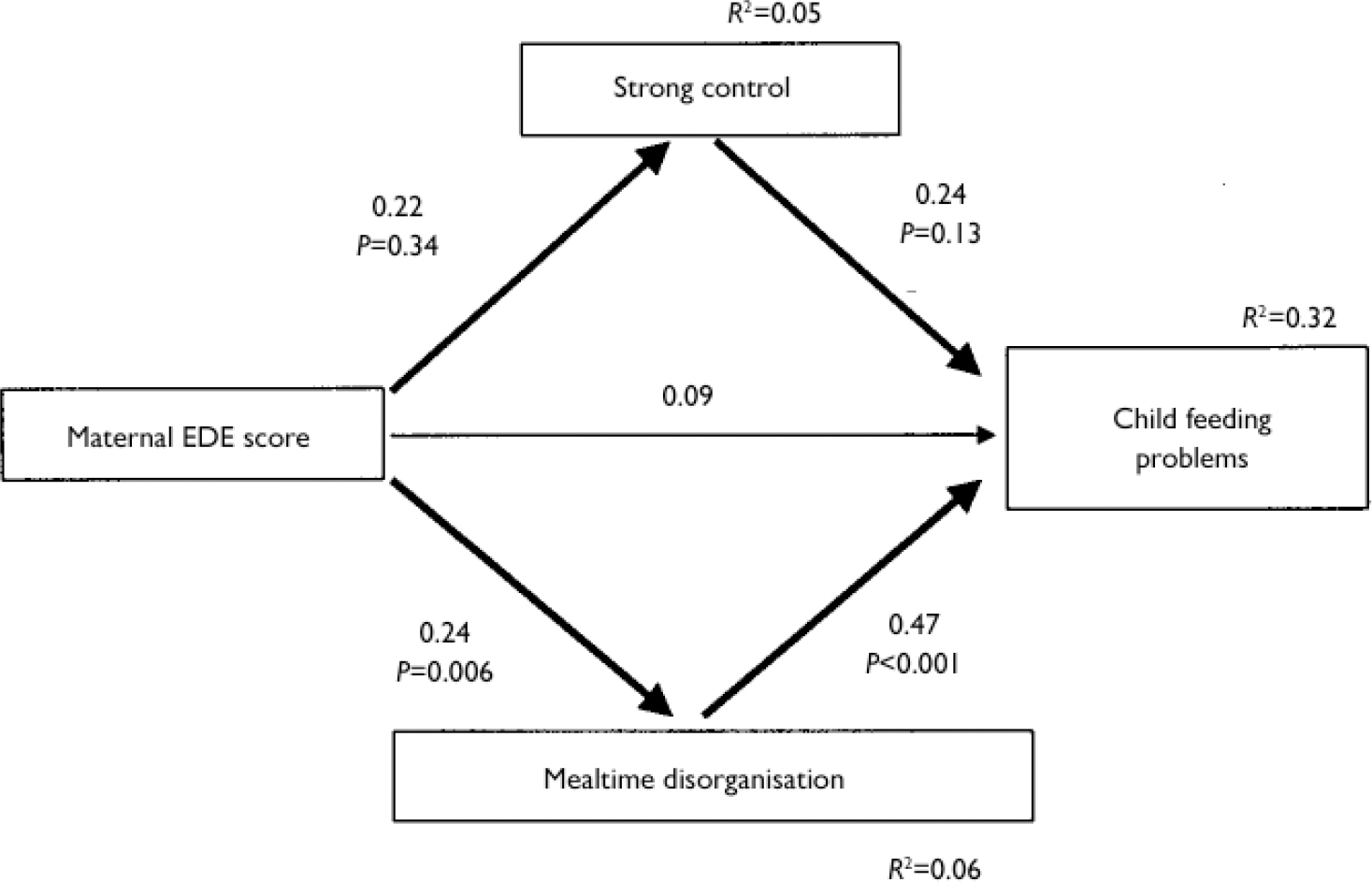
Fig. 3 Path analysis showing the prediction of the degree of child feeding problem by the level of maternal eating disorder psychopathology, the level of mealtime disorganisation and maternal strong control. EDE, Eating Disorder Examination.
Table 1 Univariate correlation matrix between the four critical variables (n=116, Spearman)
| Maternal EDE score | Mealtime disorganisation | Strong control | Feeding problem | |
|---|---|---|---|---|
| Maternal EDE score | 1.00 | |||
| Mealtime disorganisation | 0.21* | 1.00 | ||
| Strong control | 0.19* | 0.14 | 1.00 | |
| Feeding problem | 0.23* | 0.44** | 0.28** | 1.00 |
DISCUSSION
Family aggregation of eating disorders
Eating disorders aggregate in families, and show shared transmission between the different forms of disorder (Reference Lilenfeld, Kaye, Hock, Treasure and KatzmanLilenfeld & Kaye, 1998; Reference Strober, Freeman and LampertStrober et al, 2000). Thus, studies of the rate of eating disorders (anorexia nervosa, bulimia nervosa and their variants) in the first-degree relatives of patients with anorexia nervosa have shown an elevated risk compared with the risk in both the relatives of normal controls and in the relatives of patients with other forms of disorder (e.g. Reference Lilenfeld, Kaye and GreenoLilenfeld et al, 1998; Reference Strober, Freeman and LampertStrober et al, 2000). Similarly, the risk of an eating disorder among the relatives of patients with bulimia nervosa has been shown to be higher than that among controls (e.g. Reference Lilenfeld, Kaye and GreenoLilenfeld et al, 1998; Reference Strober, Freeman and LampertStrober et al, 2000). The degree to which this aggregation is accounted for by genetic and environmental variation is unclear. Although the few twin studies to have been conducted in the main reveal a strong genetic component, their interpretation is by no means clear (Reference Fairburn, Cowen and HarrisonFairburn et al, 1999), and the balance of the current evidence suggests an important aetiological role for both genetic and family-environmental factors.
Contribution of the family environment to family aggregation
The research on the contribution of the family environment to the intergenerational transmission of eating disorders is limited in both quantity and quality. Some case reports suggest an adverse impact of anorexic and bulimic behaviour on both foetal development and infant growth (e.g. Reference Treasure and RussellTreasure & Russell, 1988), and of an adverse effect of bulimia nervosa on parenting (e.g. Reference Stein and FairburnStein & Fairburn, 1989). However, there has been only one systematic study of the impact of maternal eating disorder on early caregiving and infant developmental progress (Stein et al, Reference Stein, Woolley and Cooper1994, Reference Stein, Murray and Cooper1996). In this study mothers with eating disorders and their year-old infants were compared with a control group of mothers and infants during both feeding and playing. At mealtimes mothers with eating disorders were found to be more intrusive, and there was more conflict between these mothers and their infants, compared with the control group; they were also more likely to be intrusive and controlling during play. In addition, the year-old infants of the mothers with eating disorders were significantly lighter than similarly aged infants of normal mothers and of mothers who had experienced postnatal depression (Reference Stein, Murray and CooperStein et al, 1996). The extent to which these disturbances in the early mother-infant relationship were related to the development of disturbances in eating in the child remains to be clarified by further longitudinal work.
Specificity in intergenerational transmission
Some evidence of specificity in intergenerational transmission comes from ‘bottom-up’ studies. Thus, Pike & Rodin (Reference Pike and Rodin1991), in a community sample of girls attending high school, found that those with disordered eating had mothers who (in comparison with the mothers of girls with no eating disturbance) themselves had disturbed eating habits and attitudes, and were more critical of their daughters’ weight and appearance. The clearest bottom-up evidence of inter-generational transmission comes from two studies of children with feeding problems (Reference Stein, Stein and WaltersStein et al, 1995; Reference Whelan and CooperWhelan & Cooper, 2000). In the earlier study, profiles on the self-report version of the EDE were compared between three groups: mothers of young children who had been referred to an out-patient child psychiatry clinic with a feeding disorder; mothers of children referred to the same clinic with a non-feeding form of behavioural disturbance; and mothers of a normal control group of children. On all the EDE sub-scales (restraint, bulimia, eating concern, weight concern and shape concern), the mothers of the children with feeding disorders had significantly higher mean scores than the mothers of the children from both the normal and the behaviourally disturbed control groups. The findings from this clinic-based study have recently been confirmed and extended in a community study, which avoids the problems of referral bias inherent in clinic samples. In a sample of children identified as having a feeding problem, the odds of a history of a maternal eating disorder were substantially higher than among the mothers of children with non-feeding forms of disturbance (Reference Whelan and CooperWhelan & Cooper, 2000).
The latter two studies suggest a specific association between maternal eating disorders and child feeding problems, and they suggest that intergenerational transmission may manifest itself early in child development. Clinically, this suggests that comprehensive assessment of children presenting with feeding problems should routinely include an assessment of the mother's eating history. Scientifically, it raises the question of the mechanism by which this relationship between child and maternal disorder is established and maintained. The rather modest contribution of genetics to the familiality of eating disorders (Reference Fairburn, Cowen and HarrisonFairburn et al, 1999) suggests that the family environment might well have a significant role. The fact that the parenting of infants of mothers with bulimia nervosa is disturbed, especially in relation to child feeding (Stein et al, Reference Stein, Woolley and Cooper1994, Reference Stein, Murray and Cooper1996), provides some empirical basis for such speculation. There is, however, surprisingly little other empirical support for this idea in the research literature.
Findings of this study
Our study indicated that two aspects of the family environment were strongly associated with the presence of child feeding problems: mealtime disorganisation, and a mother-child relationship characterised by strong maternal control and disharmony. For both these variables the group of children with feeding problems was clearly distinguished from both the normal control group and the disturbed comparison group. Although it is certainly possible that for both of these variables the disturbances identified were secondary to the child feeding problem, this is not a likely account of the basis to the associations found. The variables that made up the ‘mealtime disorganisation’ index were, in the main, gross descriptors of the home environment and the process of family meals. Whether the meal was served at a table with chairs, whether or not the mother ate with the child, and whether the meal was eaten in front of a television, are unlikely to have been influenced by the child's own eating behaviour. The maternal ‘strong control/disharmony’ index was also unlikely to have been substantially influenced by the extent of child feeding disturbance, since this variable was derived from a task that had nothing to do with food or eating. It seems, therefore, plausible that these two indices of family disturbance were factors that could have contributed to the development and maintenance of child feeding problems.
The path analysis revealed that the two family-environmental variables did, indeed, mediate the relationship between maternal eating disorder psychopathology and the level of child feeding disturbance. This suggests a mechanism for the transmission of feeding disturbance from mother to child: it appears that mothers with high levels of eating disorder psychopathology tend to provide a disorganised mealtime environment for their children and tend to have a controlling and disharmonious style of interacting with them, and in this context children are likely to develop disturbed eating habits such as faddiness and refusal.
Whether the processes elucidated in our study have any bearing on the intergenerational transmission of DSM-IV eating disorders remains an entirely open question, one that hangs on the relationship between early childhood feeding disturbance and later frank eating disorder. There is little previous research to illuminate this question, and the few findings that have been reported have been conflicting. Thus, Mitchell et al (Reference Mitchell, Boutacoff and Wilson1986) reported that the mothers of patients with bulimia nervosa rarely could identify a significant feeding problem before the onset of the eating disorder; Jacobs & Isaacs (Reference Jacobs and Isaacs1986), on the other hand, found that their patients with prepubertal anorexia nervosa had a higher rate of childhood feeding problems than both patients with anorexia nervosa of classical post-pubertal onset and a pre-pubertal group of patients with a non-eating form of disturbance. The most commonly cited evidence for an association between early feeding problems and later eating disorders comes from a study reported by Marchi & Cohen (Reference Marchi and Cohen1990). They reported early pica to be predictive of later bulimia nervosa, and early ‘picky’ eating to predict adolescent anorexia nervosa. However, although this study was longitudinal, assessments were made at a range of ages and the data were not truly prospective. Elucidation of this issue therefore awaits the findings of a systematic, prospective longitudinal study.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ ▪ Given the high rate of eating disorder among mothers of children with feeding problems, it is essential when assessing children with such disturbance to investigate the mother's eating history.
-
▪ ▪ Comprehensive assessment of child feeding problems should include observation of a family meal, as well as wider assessment of the quality of the mother-child relationship.
-
▪ ▪ It is likely that successful treatment of child feeding problems will involve a reorganisation of family meals and measures to improve the quality of the mother-child relationship.
LIMITATIONS
-
▪ ▪ Although supported by direct observations, the child feeding problems variable used in the predictive model was derived from maternal reports of child disturbance and could have been subject to bias.
-
▪ ▪ It is important to establish in future work that the relationships elucidated in this study also obtain in children with feeding disturbance of clinical levels of severity.
-
▪ ▪ The significance of the associations found in this study for the intergenerational transmission of DSM-IV eating disorders is uncertain, and can only be determined by longitudinal research.
Acknowledgements
We are grateful to the children and their mothers who took part in this. study. We are also indebted to Keith Evans and Helen McMullen of the Berkshire. Department of Education for identifying the schools, and to the staff of the. schools themselves for assisting in carrying out the screening. Marian Eke and. Catherine Herba helped with data collection.









eLetters
No eLetters have been published for this article.