Beyond the early writings and philosophies on the morality of suicide, the current focus has been on explaining why suicidal behavior occurs (Klonsky & May, Reference Klonsky and May2015; Klonsky, Saffer, & Bryan, Reference Klonsky, Saffer and Bryan2018; Van Orden et al., Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner2010). This chapter first summarizes several theories of suicide, with a focus on the eighteenth century to the present, and how they uniquely frame various aspects of pain and suffering that lead to suicide. We highlight how these theories evolved over time, with varying foci on individual and societal pathology, and how earlier theories are evident in present day views. We then conclude with a discussion of the known factors that confer and buffer against risk for suicide.
Suicide Theories
We can see the underpinnings of our current understanding of suicide as far back as the French psychiatrist Jean-Etienne Dominique Esquirol (Reference Esquirol1845). He viewed suicide as an involuntary behavior, the result of genetic, psychological, and social factors outside of one’s control. His view is one of the earliest indications of the shift from perceiving suicide as a sinful, volitional behavior within an individual to an understanding of it as a result of various biopsychosocial forces. These views are later reflected in the work of Emile Durkheim (see below) and have influenced our current understandings of suicide, which highlight the impact of complex biopsychosocial factors.
Early understandings of suicide also grappled with cognitive components of the phenomenon. Arthur Schopenhauer (Reference Schopenhauer1893), a German philosopher, suggested that the mind constructs one’s understanding of everything; therefore, suicide is due to distress resulting from cognitive errors that lead to the conclusion that one’s existence is the problem. Here, the fear of life outweighs the fear of death. Schopenhauer highlights that emotionally distressing events can remove objectivity, distorting one’s perceptions. Schopenhauer’s focus on cognitive errors and distortions can be seen in contemporary theories emphasizing the importance of believing oneself is a burden or does not belong (see Interpersonal Theory below), as well as cognitive interventions for suicide prevention. And with Schopenhauer’s focus on the events that can impair objectivity, he begins the discussion of external factors that can contribute to suicidogenic cognitions and drive suicide.
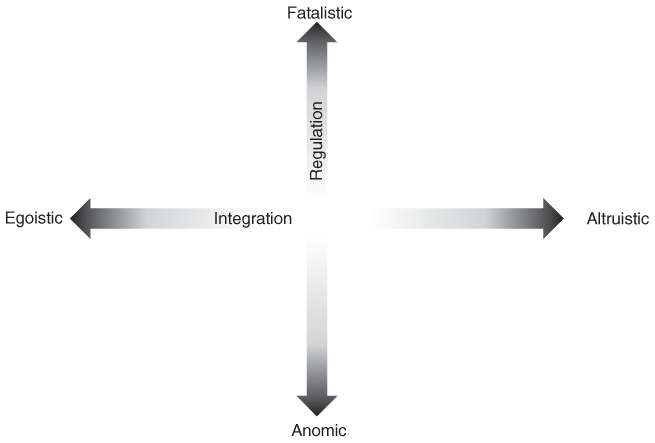
Similarly, Emile Durkheim (Reference Durkheim2005), the founder of French sociology, also focused on external drivers, suggesting that suicide is the result of the society in which one lives. Durkheim’s philosophies were steeped in the idea of collective consciousness, the view that a shared set of beliefs and knowledge within a group influences our sense of self, belonging, and behavior. As such, the social environment, as opposed to individual psychology, was the key construct in his understanding of suicide. Durkheim suggested that a society’s acceptance of suicide as an alternative is a symptom of larger societal dysfunction and theorized that suicide is a symptom of societal breakdown. With suicide reflecting the nature of a society’s social relationships, he created a typology categorizing suicide into four groups (altruistic, egoistic, anomic, and fatalistic; see Figure 2.1), each varying in degree of social integration and social regulation, with suicide risk increasing at the extremes of the continua.
Egoistic suicide occurs in a society with little sense of belonging, social integration, and connectedness. Excessive individuation results in hopelessness, meaninglessness, apathy, and negative mood. On the other hand, altruistic suicide is characterized by too much integration into society, with individual needs outweighed by those of society. Here, individual identity is lost or meaningless. Anomic suicide occurs in societies that lack social or moral regulation, most commonly during social, political, or economic unrest that leave people grappling with uncertainty and instability. At the high end of social regulation is fatalistic suicide, occurring when society is excessively regulated. Here, there is almost no change in social environment or role expectations, generating monotony and hopelessness. While Durkheim designated this a theoretical category, it may occur in oppressive regimes, where people would rather die than persevere.
Per Durkheim, the decreasing importance of state, religion, marriage, and family has resulted in a regulation deficit in modern society. These formerly core institutions no longer provide social structure and organization, resulting in a growing sense of alienation and social issues that have negative health consequences and increased suicide rates. He posited that, instead, work has become the central institution within modern society, so investing in corporations, workplaces, and occupational groups is a potential pathway for reinstating a collective consciousness. Although Durkheim’s theory is not without limitations (Mueller et al., Reference Mueller, Abrutyn, Pescosolido and Diefendorf2021), it remains a key foundational theory for understanding suicide.
Psychodynamic theories diminished the role that society plays in suicide and reflected the general understanding of human behavior as the result of psychological forces. The specific forces varied depending on the theory but were largely seated within the individual (Bowlby, Reference Bowlby1973; Hendin, Reference Hendin1991; Menninger, Reference Menninger1938). For example, Sigmund Freud (Reference Freud1938, Reference Freud, Freud, Strachey and Freud1957) emphasized the role of unconscious drives, particularly the death drive, Thanatos, as the underlying impetus for aggression, self-destructive behavior, and suicide. From his perspective, suicide can serve as a punishment or fulfillment of a wish. The latter suggests that suicide occurs when the person has identified so strongly with an object (another person, such as a parent), and they turn the wish of death for that object against themselves, indirectly fulfilling that wish.
Collaborators of Freud’s, who later fell out of favor with the psychodynamic leader, added their own perspective to the psychodynamic view of suicide. Alfred Adler (Reference Adler, Ansbacher and Ansbacher1964), for example, was one of the earliest to view suicide from a social psychology perspective, emphasizing roles for both individual characteristics and situational factors in the development of suicidality. This more holistic perspective aligned with the evolution of psychiatry and psychology at the time and also his theory of individual psychology where social and human contexts are essential to understanding and treating psychiatric concerns. In regard to suicide, Adler highlighted the role of social interest, a person’s connection with others and a sense of belonging in the community. As such, suicide is something that could be intervened upon by increasing social connectedness and relationships (Adler, Reference Adler, Ansbacher and Ansbacher1964; Ansbacher, Reference Ansbacher1969), a foreshadowing of later theories that incorporate aspects of belonging.
Edwin Shneidman (Reference Shneidman1981, Reference Shneidman1993), the founder of the American Association of Suicidology, identified intense psychological pain, which he called psychache, as the most significant contributor to suicide. Psychache is an overwhelming amount of emotional pain that, when it exceeds the individual’s capacity to cope with it, results in suicide. While his theory was influenced by his predecessors in that it is individually focused, it can be paired with interpersonal and sociological explanations and thus helped move psychology out of its focus on psychoanalytic explanations. Shneidman’s movement away from psychodynamic explanations and his emphasis on overwhelming psychological pain has influenced later researchers and theorists, particularly those emphasizing the role of escape. This can be seen with Baumeister (Reference Baumeister1990) describing suicide as a means of escape from an aversive state of mind or self-awareness, Linehan (Reference Linehan1993) highlighting the role of escaping difficult emotions, Williams (Reference Williams2001) suggesting suicide as an escape from defeat or entrapment (similar to arrested flight per Gilbert & Allan, Reference Gilbert and Allan1998), and Beck et al. (Reference Beck, Kovacs and Weissman1975) and Abramson et al. (Reference Abramson, Alloy, Hogan, Whitehouse, Gibb, Hankin, Cornette, Joiner and Rudd2002) adding to this by highlighting the role of hopelessness. Indeed, significant effort has been spent to characterize the various aspects of intense psychological pain.
Shortcomings of the preceding theories include the limited differentiation of suicide ideation and behavior, emphasis on single variables, and no clear mechanism by which ideation transitions to behavior. More recent theories addressed these gaps by embracing an ideation-to-action framework (Klonsky, Saffer, & Bryan, Reference Klonsky, Saffer and Bryan2018). These theories include the Interpersonal-Psychological Theory – also called the Interpersonal Theory – of Suicide (Joiner, Reference Joiner2005; Van Orden et al., Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner2010), the Integrated Motivational–Volitional (IMV; O’Connor & Kirtley, Reference O’Connor and Kirtley2018) Model, the Three-Step Theory (3ST; Klonsky & May, Reference Klonsky and May2015), and the Fluid Vulnerability Theory (FVT) (Rudd, Reference Rudd, Berman, Joiner, Nock, Silverman, Mandrusiak and Witte2006). These models explore pathways to suicide ideation and ultimately behavior. This is important considering a larger proportion of the population experiences ideation than behavior; these groups are likely qualitatively different, and it is necessary to understand the overlapping and unique processes that result in suicidal thoughts, actions, and deaths.
Interpersonal Theory (Joiner, Reference Joiner2005; Van Orden et al., Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner2010) is one of the most influential and empirically supported theories of suicide. This theory indicates that suicide is the result of a combination of both the desire and the ability to kill oneself. The desire to die by suicide is a function of self-perceptions related to others, specifically social cognitions about thwarted belongingness and perceived burdensomeness (see Table 2.1). When thwarted belongingness and perceived burdensomeness persist and one begins to feel hopeless, desire for suicide will emerge.
Table 2.1 Interpersonal theory of suicide constructs (Joiner, Reference Joiner2005; Van Orden et al., Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner2010)
| Construct | Occurs when | Representative cognitions |
|---|---|---|
| Thwarted belongingness | Unmet need for social connectedness | “I am all alone.” “I don’t fit in here.” |
| Perceived burdensomeness | Unmet need for social competence (e.g., relationship problems, unemployment) | “I am such a drain on other people.” “It would be better for everyone else if I were gone.” |
This desire transforms into suicide behavior when the person develops the capability to overcome their natural instincts to avoid pain, injury, and death (Joiner, Reference Joiner2005; Smith et al., Reference Smith, Stanley, Joiner, Sachs-Ericsson and Van Orden2016; Van Orden et al., Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner2010). Suicide capability fluctuates over time (Law & Anestis, Reference Law and Anestis2021) and is largely developed through an opponent process and habituation. The more the person experiences pain- or fear-inducing events, the less the events affect them. When such events occur repeatedly, the initial aversive response is suppressed. Indeed, capability for suicide is increased among those with previous suicide attempts, self-harm, familiarity with the idea of suicide and death, and a high pain threshold. Capability for suicide behavior can be acquired through life experiences that are known risk factors for suicide, such as sexual trauma, violence, and intravenous drug use (Joiner, Reference Joiner2005). Thus, the mechanism by which these risk factors contribute to suicide may be by increasing suicide capability. There is strong empirical support for Interpersonal Theory, its constructs, and their relationships, though some have highlighted a need for further clarification of constructs and better measurement tools (Klonsky, Saffer, & Bryan, Reference Klonsky, Saffer and Bryan2018; Ma et al., Reference Ma, Batterham, Calear and Han2016; Stewart et al., Reference Stewart, Eaddy, Horton, Hughes and Kennard2017).
Another ideation-to-action theory, the Integrated Motivational–Volitional (IMV; O’Connor & Kirtley, Reference O’Connor and Kirtley2018) Model of suicidal behavior is heavily influenced by the Cry of Pain Theory (Williams, Reference Williams2001), which suggests that suicide is a response to circumstances with three components: defeat, no escape, and no rescue. The IMV model breaks suicide into three phases that highlight the roles of and relationship between defeat, humiliation, and entrapment (O’Connor & Kirtley, Reference O’Connor and Kirtley2018). The Pre-Motivational Phase describes the biopsychosocial context in which suicide ideation and behavior emerge. Then, in the Motivational Phase, negative feelings of defeat and their interaction with poor coping and problem-solving skills ultimately contribute to feeling trapped. This experience, feeling trapped, contributes to viewing suicide as an alternative to negative life experiences and drives suicidal intent (O’Connor & Kirtley, Reference O’Connor and Kirtley2018). When there is an increased capacity for suicide, impulsivity, planning, imitation/contagion, access to lethal means, and other facilitating factors, intent transforms into suicide behavior in the Volitional Phase. There is support for the IMV model, with evidence that defeat and entrapment are strongly associated with suicide ideation (SI) and that variables broader than just acquired capability differentiate those with ideation vs. attempts (Dhingra et al., Reference Dhingra, Boduszek and O’Connor2015). However, further validation of this model and adaptations for certain groups may be necessary (Pollak et al., Reference Pollak, Guzmán, Shin and Cha2021).
Klonsky and May’s (Reference Klonsky and May2015) 3ST defines the pain that can generate SI more broadly than other ideation-to-action theories and does not limit this to psychological pain. This theory suggests that suicide behavior is explained by four components (pain, hopelessness, connection, and capability for suicide), and both pain and hopelessness must be present for suicide desire to emerge. In the absence of hopelessness, energy would instead be diverted to coping rather than toward escape or avoidance. As pain and hopelessness intensify or persist, they erode the buffering effects of connectedness (i.e., social support, roles, and purpose) that make life worth living. The extent to which pain and suffering overwhelm an individual’s connectedness determines the intensity of suicide desire. Similar to other ideation-to-action theories, 3ST suggests that suicidal desire leads to a suicide attempt when suicide capability exists. Here, suicide capability is determined by factors that go beyond acquired capability, and includes broader experiences that reduce fear of pain, injury, and death, dispositional factors (e.g., temperament, genetics), and practical factors (e.g., access to means). Klonsky and May’s (Reference Klonsky and May2015) preliminary research on this model demonstrated that pain and hopelessness combine to account for a large proportion of the variance in SI and may predict SI to a greater extent than just thwarted belongingness and perceived burdensomeness, as proposed by Interpersonal Theory. Further, the model’s broader variables related to suicide capability each predicted suicide attempt history beyond what was predicted by current and lifetime SI (Klonsky & May, Reference Klonsky and May2015). Additional support for the 3ST model comes from studies in the UK (Dhingra, Klonsky, & Tapola, Reference Dhingra, Klonsky and Tapola2019), China (Yang, Liu, Chen, & Li, Reference Yang, Liu, Chen and Li2019), and Canada (Tsai et al., Reference Tsai, Lari, Saffy and Klonsky2021).
A final ideation-to-action framework, the FVT (Rudd, Reference Rudd, Berman, Joiner, Nock, Silverman, Mandrusiak and Witte2006), is based on a cognitive-behavioral framework suggesting people may be vulnerable to suicide as a stress response, a “suicidal mode” (Rudd, Reference Rudd, Yates, Sweeny, Robbins and Cohen2000). FVT also uniquely addresses temporal dynamics and periods of ambivalence around suicide. The model assumes that suicide risk operates in a nonlinear fashion, has both stable and dynamic aspects, and is resolved when multiple components of the “suicidal mode” are addressed. Like other models, FVT posits that cognitions can drive suicide but is less restrictive in terms of which cognitions are suicidogenic. This model does not focus on burdensomeness or belongingness but rather highlights a suicidal belief system, comprised of many thoughts that can contribute, singly or in combination, to suicide. The model also highlights the role that mechanisms like cognitive inflexibility and emotion regulation deficits can play in fostering such a belief system. There is support for this theory, showing that a wider range of cognitions better discriminate those with SI vs. attempts vs. non-suicidal self-injury (Bryan et al., Reference Bryan, Rudd, Wertenberger, Etienne, Ray-Sannerud, Morrow and Young-McCaughon2014; Klonsky, Saffer, & Bryan, Reference Klonsky, Saffer and Bryan2018). Further, measures that assess a wider range of cognitions (e.g., unlovability, unbearability) better predict suicide attempts and crisis intensity relative to more narrow measures of thwarted belonginess or perceived burdensomeness and hopelessness (Bryan et al., Reference Bryan, Rudd, Wertenberger, Etienne, Ray-Sannerud, Morrow and Young-McCaughon2014). This is not to say that burdensomeness or thwarted belonging are not suicidogenic but are likely among numerous cognitive pathways that lead to suicide.
More recently, Macintyre and colleagues (Reference Macintyre, Mansell, Pratt and Tai2021) have applied Perceptual Control Theory (PCT; Powers, Reference Powers1973), a transdiagnostic framework of well-being and distress, to suicide, specifically focusing on crisis periods. The authors argue that although hopelessness, entrapment, thwarted belonginess, and burdensomeness are integral to suicide, these cognitive–affective states result from chronic, unresolved, distressing goal conflict (e.g., increasing belonging without feeling like they are burdening others). As the conflict goes unresolved and the person becomes aware of this incompatibility, there can be a perceived loss of control great enough to generate a crisis. It is at this point that suicide is viewed as way to regain control and achieve a goal, such as ending emotional pain. Macintyre and colleagues (Reference Macintyre, Mansell, Pratt and Tai2021) further argue that because individuals experiencing SI often experience cognitive constriction, with a bias toward suicide-related stimuli and rumination (Cha et al., Reference Cha, Najmi, Park, Finn and Nock2010; Rogers, Gallyer, & Joiner, Reference Rogers, Gallyer and Joiner2021), they may lose sight of how suicide impacts the attainment of other goals. The authors suggest that this limited awareness is the common mechanism underlying suicide attempts, regardless of the constellation of specific risk factors present. Thus, they suggest that treatment target this mechanism rather than the cognitive–affective states that emerge from it (e.g., burdensomeness) and focus on increasing awareness of higher-order goals and identifying effective ways to achieve these goals.
There is no shortage of theories on the underpinnings of suicide. All of these theories highlight various painful aspects of the human experience (albeit at times with overlapping and poorly defined constructs; Millner, Robinaugh, & Nock, Reference Millner, Robinaugh and Nock2020; see Figure 2.2) that overwhelm coping skills, emotion regulation, and biological systems to transition into suffering, and ultimately suicide. In the next section, we highlight briefly what is known about the specific risk factors that contribute to this process.

Figure 2.2 The overlapping vague constructs historically used in suicide theories.
Risk Factors for Suicide
As theories of suicide are developed and evaluated, they must be able to accommodate each of the many known suicide risk factors. Risk factors are categorized into either static or dynamic risk factors. Static risk factors are stable characteristics (e.g., age, sex, and race) that confer a foundational risk for suicide, whereas dynamic risk factors vacillate over an individual’s life and can be targeted in treatment (e.g., alcohol use and relationship conflict) (Steele et al., 2017). Figure 2.3 depicts how risk (and protective) factors can be categorized across ecological levels (individual, interpersonal, community, and societal), capturing the broader context of factors that drive suicide.
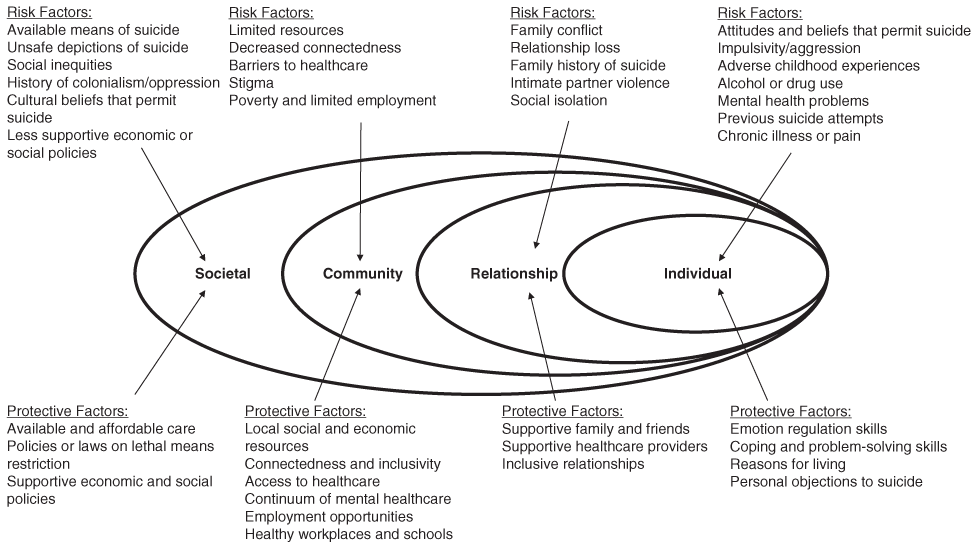
Figure 2.3 The social–ecological model of suicide.
Individual-Level Risk Factors
At the individual level, within-person risk factors, such as clinical characteristics or family history, are critical to addressing suicide risk. For example, significant research has demonstrated that a history of suicide attempts increases risk of future attempts (Beghi & Rosenbaum, Reference Beghi and Rosenbaum2010; Hawton et al., Reference Hawton, Sutton, Haw, Sinclair and Harriss2005; Nanayakkara et al., Reference Nanayakkara, Misch, Chang and Henry2013). Further, those who make multiple attempts have significantly greater odds of making subsequent attempts compared to those with ideation or a single attempt (Miranda et al., Reference Miranda, Scott, Hicks, Wilcox, Munfakh and Shaffer2008), and having multiple attempts increases the odds of eventual suicide death (Reid, Reference Reid2009). It should be noted, though, that most individuals who attempt to die by suicide will not actually go on to die by suicide (Owens, Reference Owens, Horrocks and House2002).
Many, but not all, individuals who die by suicide have mental health diagnoses. While mental illness is common among people who die by suicide (Bertolote et al., Reference Bertolote, Fleischmann, De Leo and Wasserman2004; Ferrari et al., Reference Ferrari, Norman, Freedman, Baxter, Pirkis, Harris and Whiteford2014), most people with a mental illness do not attempt suicide (Van Orden et al., Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner2010). Some diagnoses are known to confer greater risk. For example, individuals with bipolar disorder are at – twenty to thirty times greater suicide risk than the general population. Indeed, bipolar disorder has the highest suicide rate of all psychiatric diagnoses, and up to one-half of individuals with bipolar disorder make one or more suicide attempts (Miller & Black, Reference Miller and Black2020). However, Stone et al. (Reference Stone, Simon, Fowler, Kegler, Yuan, Holland and Crosby2018) reported that over half of those in twenty-seven U.S. states who died by suicide between 1999 and 2016 had no known mental illness. Similarly, Ahmedani et al. (Reference Ahmedani, Simon, Stewart, Beck, Waitzfelder, Rossom and Solberg2014) showed only about half of those who died by suicide had mental health diagnoses in the year before their death. This shows the complex relationship between mental health and suicide and that addressing only a clinical population (i.e., those with a psychiatric diagnosis) will overlook a proportion of people who die by suicide.
Alcohol and substance use can increase the risk of suicidal behavior by impairing judgment, reducing impulse control, and compounding negative life events and problems (Esang & Ahmed, Reference Esang and Ahmed2018). In addition to increasing suicide risk, numerous suicides take place during intoxication. Esang and Ahmed (Reference Esang and Ahmed2018) reported notable proportions of suicide deaths involve alcohol (22%), opiates (20%), marijuana (10%), cocaine (5%), and amphetamines (3%). Co-occurring mental health and substance use disorders further amplify risk, often in a cycle where mental health symptoms and substance use exacerbate one another (Carra et al., 2014; Effinger & Stewart, Reference Effinger and Stewart2012). Understanding how substance use and psychiatric disorders increase risk independently and in combination is essential to evaluating suicide risk.
Suicide also occurs more frequently among those with a history of violence, aggressive behavior, and impulsivity (Gvion & Apter, Reference Gvion and Apter2011). Numerous studies have documented that individuals with greater impulsivity are more likely to experience SI or engage in suicide behavior (Conner, Meldrum, Wieczorek, Duberstein, & Welte, Reference Conner, Meldrum, Wieczorek, Duberstein and Welte2004; Hull-Blanks, Kerr, & Robinson Kurpius, Reference Hull-Blanks, Kerr and Robinson Kurpius2004; Maser et al., Reference Maser, Akiskal, Schettler, Scheftner, Mueller, Endicott and Clayton2002; Neufeld & O’Rourke, Reference Neufeld and O’Rourke2009). Impulsivity is associated with the lethality and number of past attempts (Chesin, Jeglic, & Stanley, Reference Chesin, Jeglic and Stanley2010) and may increase suicide risk beyond the risk associated with mental health diagnoses (Chesin, Jeglic, & Stanley, Reference Chesin, Jeglic and Stanley2010; Dumais et al., Reference Dumais, Lesage, Alda, Rouleau, Dumont, Chawky and Turecki2005), particularly among those lacking social support (Kleiman et al., Reference Kleiman, Riskind, Schaefer and Weingarden2012).
Beyond their own clinical characteristics, an individual’s family history of suicide is a particularly strong risk factor. Studies of twins and adopted children suggest that suicide is genetically transmitted (Glowinski et al., Reference Glowinski, Bucholz, Nelson, Fu, Madden, Reich and Heath2001; Statham et al., Reference Statham, Heath, Madden, Bucholz, Bierut, Dinwiddie and Martin1998), with an early study (Roy et al., Reference Roy, Segal, Centerwall and Robinette1991) reporting that 11.3% of monozygotic twin pairs were concordant for suicide compared with 1.8% of dizygotic twin pairs. While some have suggested that these findings may be driven by the genetic predisposition for mental health problems, evidence suggests that the genetic contribution to suicide is independent of the genetic transmission of psychiatric disorders (Mann et al., Reference Mann, Waternaux, Haas and Malone1999; Powell et al., Reference Powell, Geddes, Deeks, Goldacre and Hawton2000; Qin et al., Reference Qin, Agerbo and Mortensen2003; Runeson & Åsberg Reference Runeson and Åsberg2003). Thus, assessment of family history of psychiatric diagnoses and suicide is necessary.
Serious medical diagnoses and chronic illnesses can also increase suicide risk (Ferro et al., Reference Ferro, Rhodes, Kimber, Duncan, Boyle, Georgiades and MacMillan2017; Greydanus, Patel, & Pratt, Reference Chesin, Jeglic and Stanley2010; Gürhan et al., Reference Gürhan, Beşer, Polat and Koç2019). One meta-analysis demonstrated that the risk of suicide is 100 times greater among people living with HIV/AIDS than in the general population (Pelton et al., Reference Pelton, Ciarletta, Wisnousky, Lazzara, Manglani, Ba and Ssentongo2021). Another meta-analysis (Du et al., Reference Du, Shi, Yu, Liu, Jin, Fu and Chen2020) found that individuals with cancer had a high incidence of suicide. Similarly, severe heart diseases, such as heart failure, are associated with increased suicide risk (Liu et al., Reference Liu, Wang, Weng, Cheng, Yeh, Bai and Chang2018). This risk is particularly elevated within six months of diagnosis (Du et al., Reference Du, Shi, Yu, Liu, Jin, Fu and Chen2020; Liu et al., Reference Liu, Wang, Weng, Cheng, Yeh, Bai and Chang2018), and appointments where individuals receive or recently received a diagnosis are an opportunity for screening.
Personal circumstances (e.g., legal, financial) are individual-level factors that can drive suicide risk. Elevated risk has been reported among individuals with legal issues, particularly criminal offenses (Fazel et al., Reference Fazel, Cartwright, Norman-Nott and Hawton2008; Pratt et al., Reference Pratt, Piper, Appleby, Webb and Shaw2006). Suicide risk is also greater among those who are unemployed (Cunningham et al., Reference Cunningham, Milner, Gibb, Rijnberg, Disney and Kavanagh2021; Milner, Page, & LaMontagne, Reference Milner, Page and LaMontagne2013), and a meta-analysis reported that individuals with debt are almost eight times more likely to die by suicide (Richardson, Elliott, & Roberts, Reference Richardson, Elliott and Roberts2013). Thorough assessment of financial and legal concerns is important, and suicide risk screening may be warranted in settings that come in contact with those experiencing legal and financial problems.
While there are many risk factors for suicide identified in the general population, more specific risk factors may exist among certain populations. For example, there have been efforts to identify risk factors in different phases of life (Steele et al., Reference Steele, Thrower, Noroian and Saleh2018), individuals with psychiatric diagnoses (Bhatt et al., Reference Bhatt, Perera, Zielinski, Eisen, Yeung, El-Sheikh and Samaan2018), certain groups of Veterans (Lee et al., Reference Lee, Kearns, Wisco, Green, Gradus, Sloan and Marx2018), and women (Chaudron & Caine, Reference Chaudron and Caine2004), among others. Such specificity for risk factors among specific groups, and their intersections, would likely be beneficial to person-centered prevention.
Interpersonal-Level Risk Factors
In line with many of aforementioned theories (Durkheim, Reference Durkheim2005; Joiner, Reference Joiner2005), research has demonstrated that suicide risk is impacted by interpersonal factors. Indeed, social factors (e.g., social isolation, loneliness, and low social support) have consistently been identified as risk factors for suicide ideation and behaviors across the lifespan and cultures (Calati et al., Reference Calati, Ferrari, Brittner, Oasi, Olié, Carvalho and Courtet2019; Draper, Reference Draper2014; King and Merchant, Reference King and Merchant2008). Relationship loss, conflict, and dissolution are associated with suicide risk (Bridge et al., Reference Bridge, Goldstein and Brent2006; Séguin et al., Reference Séguin, Beauchamp, Robert, DiMambro and Turecki2014), and divorce can be a precipitating factor in suicide (Kposowa, Reference Kposowa2003; Yip et al., Reference Yip, Yousuf, Chan, Yung and Wu2015). Individuals who are separated, divorced, widowed, or never married are at increased suicide risk compared to married people (Jamison et al., Reference Jamison, Mintz, Bol and Herndon2017, Reference Jamison, Bol and Mintz2019), with certain groups more greatly impacted by separation and divorce (Wyder, Ward, & De Leo, Reference Wyder, Ward and De Leo2009). A narrative review of the literature (Calati et al., Reference Calati, Ferrari, Brittner, Oasi, Olié, Carvalho and Courtet2019) found that the social constructs associated with suicidal outcomes were marital status, living alone, social isolation, loneliness, alienation, and belongingness. Interestingly, both living alone and the perception of being lonely are associated with suicide ideation and attempts (Calati et al., Reference Calati, Ferrari, Brittner, Oasi, Olié, Carvalho and Courtet2019).
Beyond relationship status, interpersonal dynamics can also confer suicide risk. Child abuse and adverse childhood experiences (ACEs) are particularly strong risk factors for suicide. Increased risk for suicidality among those who experience child abuse or neglect has been reported in numerous populations (Devries et al., Reference Devries, Mak, Child, Falder, Bacchus, Astbury and Watts2014; Dube et al., Reference Dube, Anda, Felitti, Chapman, Williamson and Giles2001; Jardim et al., Reference Jardim, Novelo, Spanemberg, von Gunten, Engroff, Nogueira and Neto2018; Ng et al., Reference Ng, Yong, Ho, Lim and Yeo2018; Thompson et al., Reference Thompson, Kingree and Lamis2019). Childhood experiences appear to be particularly impactful, with one study reporting that childhood physical, sexual, and emotional abuse were associated with recent suicide attempts, whereas adult sexual or physical assaults were not (Briere, Madni, & Godbout, Reference Briere, Madni and Godbout2016). One larger, retrospective cohort study found that those who reported having experienced emotional, physical, or sexual abuse were two to five times more likely to have attempted suicide at some point in their lives (Dube et al., Reference Dube, Anda, Felitti, Chapman, Williamson and Giles2001). Further, ACEs may have a dose–response relationship with suicide; the number of ACEs is associated with increased odds of suicide ideation and attempts (Bhatta et al., Reference Bhatta, Jefferis, Kavadas, Alemagno and Shaffer-King2014; Liu & Tien, Reference Liu and Tein2005; Serafini et al., Reference Serafini, Muzio, Piccinini, Flouri, Ferrigno, Pompili and Amore2015; Thompson et al., Reference Thompson, Kingree and Lamis2019).
Violence in adulthood may also be associated with suicide (Devries et al., Reference Devries, Watts, Yoshihama, Kiss, Schraiber and Deyessa2011), both indirectly via mental health consequences and as an independent risk factor (Currier et al., Reference Currier, Holland, Jones and Sheu2014; Lambert et al., Reference Lambert, Copeland-Linder and Ialongo2008). This particularly impacts women, for whom physical and sexual violence are prevalent worldwide (García-Moreno et al., Reference García-Moreno, Pallitto, Devries, Stöckl, Watts and Abrahams2013). Lifetime prevalence estimates of violence against women reach as high as 50% (Alhabib, Nur, & Jones, Reference Alhabib, Nur and Jones2010). Intimate partner violence (IPV) is associated with suicide behavior and death by suicide (Brown & Seals, Reference Brown and Seals2019; Randle & Graham, Reference Randle and Graham2011; Wolford-Clevenger, Reference Wolford-Clevenger, Vann and Smith2016), particularly for women (MacIsaac, Bugeja, & Jelinek, Reference MacIsaac, Bugeja and Jelinek2017), especially Black women (Taft et al., Reference Taft, Bryant-Davis, Woodward, Tillman and Torres2009). IPV and recent altercations with significant others have been associated with the suicide risk for pregnant and postpartum women (Adu et al., Reference Adu, Brown, Asaolu and Sanderson2019). More than half of pregnancy-associated suicides involved intimate partner conflict (Palladino et al., Reference Palladino, Singh, Campbell, Flynn and Gold2011), and experiencing IPV was associated with more than nine times great odds of SI among low-income pregnant women (Alhusen et al., Reference Alhusen, Frohman and Purcell2015). Assessing for abuse and violence exposure is critical to understanding an individual’s suicide risk, and assessing for SI in settings that encounter individuals with abuse histories (e.g., shelters) may be beneficial.
The structure of a person’s social network matters in terms of suicide risk and suicide contagion (Bearman & Moody, Reference Bearman and Moody2004; Mueller & Abrutyn, Reference Mueller and Abrutyn2016). For example, adolescent and early adulthood exposure to friends who died by suicide increases the likelihood of suicide ideation and behavior (Bearman & Moody, Reference Bearman and Moody2004; Mueller, Abrutyn, & Stockton, Reference Mueller and Abrutyn2015). The impact of social networks can be broad, as evidenced by the fact that knowledge of friends of friends who attempted suicide was associated with more seriously considering suicide (Baller & Richardson, Reference Baller and Richardson2009). Interestingly, the impact of networks appears to have gendered effects, with adolescent girls having specific social structures (i.e., very small networks, or intransitive networks where friends are not friends with each other) being at increased risk of suicidality (Bearman & Moody, Reference Bearman and Moody2004). Interpersonal loss, status, dynamics, and structure all impact suicide risk, directly and indirectly, and should be assessed thoroughly. These interpersonal dynamics also likely interact with community- and societal-level variables that warrant attention.
Community- and Societal-Level Risk Factors
At the next ecological level, suicide risk is impacted by societal beliefs, norms, and messaging about mental health and suicide. For example, stigmatizing views of people who experience SI (e.g., weak, unable to cope) have been reported in many groups and countries (e.g., Nicholas et al., Reference Nicholas, Haregu, Henderson and Armstrong2022). Greater anticipated stigma is associated with increased suicidality, and this is partially mediated by secrecy (Mayer et al., Reference Mayer, Rüsch, Frey, Nadorff, Drapeau, Sheehan and Oexle2020). Stigma can contribute to suicide by preventing help seeking during a crisis (Batterham, Calear, & Chistensen, Reference Batterham, Calear and Christensen2013; Ben-Zeev et al., Reference Ben-Zeev, Corrigan, Britt and Langford2012; Niederkrotenthaler et al., Reference Niederkrotenthaler, Reidenberg, Till and Gould2014; Van Sickle et al., Reference Chan, Bhatti, Meader, Stockton, Evans, O’Connor and Kendall2016). Thus, interventions to increase literacy about suicide and reduce stigma have been suggested (Batterham, Calear, & Christensen, Reference Batterham, Calear and Christensen2013; Carpiniello & Pinna, Reference Carpiniello and Pinna2017), such as targeting sources of stigmatizing messages, such as communities, healthcare providers, or media portrayals (Carpiniello, Girau, & Orrù, Reference Carpiniello, Girau and Orrù2007; Frey et al., Reference Frey, Hans and Cerel2016; Van Sickle et al., Reference VanSickle, Werbel, Perera, Pak, DeYoung and Ghahramanlou-Holloway2016).
Media portrayals of suicide play a significant role in suicide risk. The media (i.e., newspapers, television, movies, Internet) contribute to sociocultural beliefs of suicide that drive stigma and can provide information about suicide (e.g., how to access means, lethality of means). Frighteningly, over three-quarters of a sample of individuals who attempted suicide obtained logistical information about suicide from media sources (Stack & Bowman, Reference Stack, Bowman, Niederkrotenthaler and Stack2017). Media can also contribute to suicide behavior and contagion (Gould, Reference Gould2001), particularly if the story is about a real person, the audience closely identifies with them, is a celebrity, or is covered extensively (Fink et al., Reference Fink, Santaella-Tenorio and Keyes2018; Gould, Reference Gould2001; Stack, Reference Stack2003, Reference Stack2005). Celebrity suicides often garner significant media attention, and a large review found that the suicide of a political or entertainment celebrity were 5.27 times more likely to be associated with a contagion than non-celebrity suicides (Stack, Reference Stack2005). One meta-analysis estimated that suicide risk increased by 13% after media reports of celebrity suicide (Niederkrotenthaler et al., Reference Niederkrotenthaler, Braun, Pirkis, Till, Stack, Sinyor and Spittal2020). Beyond news reporting, television shows can increase suicide. In the first three months of the airing of “13 Reasons Why,” which focused on the suicide of a 17-year-old girl with significant social stressors, suicide increased by 21.7% among teenaged females (compared to 12.4% of males) (Niederkrotenthaler et al., Reference Niederkrotenthaler, Stack, Till, Sinyor, Pirkis, Garcia and Tran2019). As such, there are recommendations for media portrayals of suicide (e.g., providing crisis line numbers, not disclosing suicide means; see www.reportingonsuicide.org for more information).
Another societal-level issue that is strongly related to suicide is access to lethal means, particularly firearms. Firearm access can be influenced at local (e.g., gun storage within the home) and national (e.g., gun laws) levels, and is hotly debated in the United States. Firearm availability is associated with suicide risk (Andres & Hempstead, Reference Andres and Hempstead2011; Anglemyer et al., Reference Anglemyer, Horvath and Rutherford2014; Fleegler et al., Reference Fleegler, Lee, Monuteaux, Hemenway and Mannix2013; Kposowa, Hamilton, & Wang, Reference Kposowa, Hamilton and Wang2016), and one meta-analysis found that firearm availability increased the odds of suicide by 3.24 times (Anglemyer et al., Reference Anglemyer, Horvath and Rutherford2014). Groups and communities differ in the value placed on firearms (Parker et al., Reference Parker, Menasce Horowitz, Igielnik, Oliphant and Brown2017), and regions with greater access to firearms have higher suicide rates (Anestis & Houtsma, Reference Anestis and Houtsma2018). However, some have found no relationship between gun availability and suicide rates (Kleck, Reference Kleck2019, Reference Kleck2022; though see Lane, Reference Lane2022), highlighting that the relationship between firearm availability and suicide may be more complex at the societal than individual level (Stack, Reference Stack2021).
Financial issues may also be more complicated at higher ecological levels. Just as financial problems increase individual suicide risk, economic recessions are associated with increased suicides (Barr et al., Reference Barr, Taylor-Robinson, Scott-Samuel, McKee and Stuckler2012; Chang et al., Reference Chang, Stuckler, Yip and Gunnell2013; Haw et al., Reference Haw, Hawton, Gunnell and Platt2015; Oyesanya et al., Reference Oyesanya, Lopez-Morinigo and Dutta2015), possibly due to unemployment (Barr et al., Reference Barr, Taylor-Robinson, Scott-Samuel, McKee and Stuckler2012; Chang et al., Reference Chang, Gunnell, Sterne, Lu and Cheng2009) and debt (Reeves et al., Reference Reeves, McKee, Gunnell, Chang, Basu, Barr and Stuckler2015). Trends in bankruptcies have been linked to national suicide rates, with one study suggesting that a 1% increase in company liquidations was associated with a 0.08% increase in suicide (Altinanahtar & Halicioglu, Reference Altinanahtar and Halicioglu2009). Increasing minimum wage may slow suicide rate growth (Gertner et al., Reference Gertner, Rotter and Shafer2019) and may reduce suicide disparities between socioeconomic groups (Kaufman et al., Reference Kaufman, Salas-Hernández, Komro and Livingston2020). Particularly relevant in 2023 is inflation, an economic issue associated with increased suicidality. Oksak et al. (Reference Okşak, Koyuncu and Yilmaz2021) reported that a 1% increase in inflation was associated with a 0.09% increase in suicide. Thus, the economy is particularly important to understanding larger contexts that may foster suicide.
Sociopolitical contexts and changes are also important. Wars and presidential elections may be related to suicide rates (Page et al., Reference Page, Morrell and Taylor2002; Stack, Reference Stack2002; Tomlinson, Reference Tomlinson2012), though effects may depend on the level of local social integration (Classen & Dunn, Reference Classen and Dunn2010), and some have failed to find an association (Wasserman, Reference Wasserman1983). Societal conflict and oppression can also contribute to suicide. Kyriopoulos and colleagues (Reference Kyriopoulos, Vandoros and Kawachi2022) demonstrated that in months with at least one killing of a Black person by police, there was a slight increase in suicides among Black Americans in the same census division. Social policies and laws can also have an effect, with suicide rates impacted by government levels of social welfare spending (Flavin & Radcliff, Reference Flavin and Radcliff2009; Minoiu and Andres, Reference Minoiu and Andres2008; Rambotti, Reference Rambotti2020; Tuttle, Reference Tuttle2018; Yur’yev et al., Reference Yuryev, Värnik, Värnik, Sisask and Leppik2012) and laws regarding lethal means and alcohol availability (Carpenter, Reference Carpenter2004; Kivisto and Phalen, Reference Kivisto and Phalen2018; Markowitz et al., Reference Markowitz, Chatterji and Kaestner2003; Xuan et al., Reference Xuan, Naimi, Kaplan, Bagge, Few, Maisto and Freeman2016). Lawmakers might consider the impact of proposed laws on their constituents with increased suicide rates attended to as a potential risk.
Protective Factors
In one sense, suicide is the result of the presence of risk factors that outweigh or overwhelm protective factors that buffer against suicide. There is less research about protective factors than about risk factors, but identifying and understanding them is essential in efforts to mitigate suicide risk. Factors that are characterized as protective against suicide have included strong coping skills, problem-solving ability, adherence to cultural or religious beliefs that discourage suicide, social support, and limited access to lethal means (CDC, 2022). Many of these listed here are the inverse of identified risk factors (e.g., social support vs. social isolation, lethal means access vs. restriction). Thus, it is important to not only lack a risk factor but to build up skills and resources in the opposing direction.
Coping and problem-solving skills are essential to navigating challenges, and the role of coping in suicide has been explored in various populations (Gould et al., Reference Gould, Velting, Kleinman, Lucas, Thomas and Chung2004; Horwitz et al., Reference Horwitz, Hill and King2011; Li and Zhang, Reference Li and Zhang2012; Liu et al., Reference Liu, Gentzler, George and Kovacs2009; Nrugham et al., Reference Nrugham, Holen and Sund2012; Speckens & Hawton, Reference Speckens and Hawton2005). Many studies (Li & Zhang, Reference Li and Zhang2012; Liu et al., Reference Liu, Gentzler, George and Kovacs2009; Nrugham et al., Reference Nrugham, Holen and Sund2012) have demonstrated that productive, problem-focused coping strategies are negatively associated with depression and/or suicide behavior, with some suggestion that emotion-oriented coping (e.g., trying to control distress via avoidance) may be harmful (Mirkovic et al., Reference Mirkovic, Labelle, Guilé, Belloncle, Bodeau, Knafo and Gérardin2015). Adolescents with past suicide behavior have greater deficits in problem-solving (Speckens & Hawton, Reference Speckens and Hawton2005) and are less likely to adopt a problem-solving coping strategy (Evans et al., Reference Evans, Hawton and Rodham2005; Nrugham et al., Reference Nrugham, Holen and Sund2012) than those without such a history. Although coping deficits are associated with depression, the association between coping deficits and suicide may exist independently of depressive symptoms (Labelle et al., Reference Labelle, Breton, Pouliot, Dufresne and Berthiaume2013; Li & Zhang, Reference Li and Zhang2012;). One French study of adolescents hospitalized for attempting suicide showed that individuals who no longer had suicidal thoughts had made greater use of productive coping strategies (Mirkovic et al., Reference Mirkovic, Labelle, Guilé, Belloncle, Bodeau, Knafo and Gérardin2015). Thus, improving coping skills, particularly for adolescents, may offer protection against suicide. Suicide-related coping (Stanley et al., Reference Stanley, Green, Ghahramanlou-Holloway, Brenner and Brown2017), coping that is applied specifically in response to suicidal urges (Interian et al., Reference Interian, Chesin, Kline, St. Hill, King, Miller and Stanley2021), is also important. Individuals who report some ability to control their suicidal thoughts are less likely to make a first suicide attempt (Nock et al., Reference Nock, Millner, Joiner, Gutierrez, Han, Hwang and Kessler2018), and individuals at high risk for suicide are less likely to experience a suicidal event within 90 days if they endorsed greater suicide-related coping (Interian et al., Reference Interian, Chesin, Kline, St. Hill, King, Miller and Stanley2021). Bolstering productive coping skills broadly, and specifically regarding suicide, can be an important component of individual suicide prevention.
Culture and religion can be protective in that they affect the types of stressors that lead to suicide, the meaning linked to stressors and suicide, and emotional and suicidal expression (Chu et al., Reference Chu, Goldblum, Floyd and Bongar2010). Indeed, one study of people hospitalized with depression found that individuals who had not attempted suicide reported greater moral objections to suicide, fears of social disapproval if they attempted suicide, fear of suicide, and sense of responsibility for their family, compared to those who had a suicide attempt (Malone et al., Reference Malone, Oquendo, Haas, Ellis, Li and Mann2000). Many of these factors can be driven by cultural beliefs and norms. These findings have been borne out elsewhere, with moral and religious objections being identified as protective against suicide (Dervic et al., Reference Dervic, Oquendo, Grunebaum, Ellis, Burke and Mann2004; Koenig et al., 2001; Lizardi et al., Reference Lizardi, Dervic, Grunebaum, Burke, Mann and Oquendo2008; Rieger et al., Reference Rieger, Peter and Roberts2015) and attendance at religious services being associated with decreased suicide risk (Chen et al., Reference Chen, Koh, Kawachi, Botticelli and VanderWeele2020; VanderWeele et al., Reference Chen, Koh, Kawachi, Botticelli and VanderWeele2020). Further, suicide rates in more religious countries are lower than rates in secular countries (Gearing & Lizardi, Reference Gearing and Lizardi2009), and a cross-national analysis found that individuals who are religiously committed, engaged with their religious community, and/or living in countries with high levels of religiosity are less accepting of suicide (Dervic et al., Reference Dervic, Oquendo, Grunebaum, Ellis, Burke and Mann2004; Neeleman et al., Reference Neeleman, Halpern, Leon and Lewis1997).
Religion may reduce suicide risk through several mechanisms. Many religions condemn suicide and violence (Gearing & Alonzo, Reference Gearing and Alonzo2018), so it follows that those committed to their religion do not view suicide as an option, or incorporate these values or the perceived consequences into their contemplation of suicide. Religion may also provide coping strategies during a crisis, such as prayer or social support via the congregation and clergy (Gearing & Alonzo, Reference Gearing and Alonzo2018; Krause et al., Reference Krause, Ellison, Shaw, Marcum and Boardman2001; Robins & Fiske, Reference Robins and Fiske2009). Religion may also instill meaning and purpose, with those with stronger religious views endorsing more reasons for living (Caribé et al., Reference Caribé, Nunez, Montal, Ribeiro, Sarmento, Quarantini and Miranda-Scippa2012; Dervic et al., Reference Dervic, Carballo, Baca-Garcia, Galfalvy, Mann, Brent and Oquendo2011; Rieger et al., Reference Rieger, Peter and Roberts2015). Religiosity may also indirectly buffer against suicide by reducing risk factors by prohibiting aggressive behavior and substance use (Dervic et al., Reference Dervic, Oquendo, Grunebaum, Ellis, Burke and Mann2004, Reference Dervic, Carballo, Baca-Garcia, Galfalvy, Mann, Brent and Oquendo2011). Indeed, religiosity is inversely associated with risk factors for suicide, including depression, hopelessness, alcoholism and substance abuse, and anxiety (Bonelli et al., Reference Bonelli, Dew, Koenig, Rosmarin and Vasegh2012; Koenig, Reference Koenig2012; Koenig et al., Reference Koenig, Koenig, King and Carson2012).
While religiosity has been associated with reduced suicide (Caribé et al., Reference Caribé, Nunez, Montal, Ribeiro, Sarmento, Quarantini and Miranda-Scippa2012; Chen et al., Reference Chen, Koh, Kawachi, Botticelli and VanderWeele2020; Dervic et al., Reference Dervic, Oquendo, Grunebaum, Ellis, Burke and Mann2004; Gearing & Lizardi, Reference Lizardi, Dervic, Grunebaum, Burke, Mann and Oquendo2008; Koenig et al., 2001; Lizardi et al., Reference Lizardi, Dervic, Grunebaum, Burke, Mann and Oquendo2008; Neeleman et al., Reference Neeleman, Halpern, Leon and Lewis1997; Rieger et al., Reference Rieger, Peter and Roberts2015; VanderWeele et al., Reference Chen, Koh, Kawachi, Botticelli and VanderWeele2020), there have been some discrepant findings (Koenig, Reference Koenig2012). It has been suggested that religiosity is associated with reduced suicide behavior, but not ideation (Burshtein et al., Reference Burshtein, Dohrenwend, Levav, Werbeloff, Davidson and Weiser2016), and some have reported that religiosity is a suicide risk factor (Jia & Zhang, Reference Jia and Zhang2012; Sidhartha & Jena, Reference Sidhartha and Jena2006). This may be due, in part, to different definitions of religiosity (e.g., attendance at services vs. religious orientation vs. personal practices), which differentially impact suicide (Robins & Fiske, Reference Robins and Fiske2009). Further, the influence of religiosity on suicide may vary by sex, age, ethnicity, country/culture studied, and type of religious coping used (Gearing & Alonzo, Reference Gearing and Alonzo2018; McKenzie et al., Reference McKenzie, Van Os, Samele, Van Horn, Tattan and Murray2003; Rosmarin et al., Reference Rosmarin, Bigda-Peyton, Öngur, Pargament and Björgvinsson2013; Sisask et al., Reference Sisask, Värnik, lves, Bertolote, Bolhari, Botega and Wasserman2010). Thus, this protective factor must be assessed and understood in context with other risk and protective factors.
Social support and connection can reduce suicide ideation and risk, particularly for individuals with high pain and high hopelessness (Klonsky & May, Reference Klonsky and May2015). Social support can be broadly defined as the availability of friends and family who provide psychological, emotional, and material resources (Hutchison, Reference Hutchison1999). One landmark study found that social support has a direct, positive effect on health and well-being, and indirect effects by providing resources and buffering against stress (Cohen & Wills, Reference Cohen and Wills1985). Social support is associated with lower likelihood of a lifetime suicide attempt, even after controlling for diverse clinical and demographic variables (Kleiman & Liu, Reference Kleiman and Liu2013). Even the perception that social support is available may reduce suicide ideation or behavior, though the protective effects of perceived social support may be influenced by whether or not the support is accessed (Chioqueta & Stiles, Reference Chioqueta and Stiles2007; Kleiman & Riskind, Reference Kleiman and Liu2013; You, Van Orden, & Conner, Reference You, Van Orden and Conner2011). Supportive and collaborative connections with healthcare providers can also reduce suicide risk and ideation (Gysin-Maillart et al., Reference Gysin-Maillart, Schwab, Soravia, Megert and Michel2016; Ilgen et al., Reference Ilgen, Czyz, Welsh, Zeber, Bauer and Kilbourne2009; Simon et al., Reference Simon, Specht and Doederlein2016), placing clinicians and other providers in a key role to bolster social support and the utilization of such networks.
Accessible mental healthcare is an essential piece of suicide prevention. There are low and inequitable rates of mental health treatment engagement, in part driven by lack of access (Wang et al., Reference Wang, Lane, Olfson, Pincus, Wells and Kessler2005). Treatment designed to be efficiently and effectively delivered can increase utilization (Coffey, Reference Coffey2007). The Henry Ford Health System, a large health maintenance organization, implemented a program focused on eliminating suicide among its members via core tenets of effectiveness, safety, patient centeredness, timeliness, efficiency, and equity. Their system of screening and follow-up care resulted in an 82% reduction in suicide between baseline and intervention (Coffey, Reference Coffey2006; Coffey & Coffey, Reference Coffey, Coffey and Ahmedani2013; Coffey et al., Reference Coffey, Coffey and Ahmedani2015). Further, visible and accessible mental healthcare can normalize help – seeking, decrease stigma, and increase service utilization. Indeed, states where mental health parity laws have been implemented have seen significant increases in self-reported mental health service utilization (Harris, Carpenter, & Bao, Reference Harris, Carpenter and Bao2006), and about a 5% reduction in suicide rates (Lang, Reference Lang2013). Thus, focusing on increased mental healthcare access can be critical to fostering protective factors.
Over the past centuries, the various aspects of pain and suffering that lead to suicide have varied in title, measurement, and construction, but we have learned that there must be sufficient pain, suffering, or distress that overwhelms the existing internal and external resources available to a person. Beyond the models that explain how a person begins to contemplate suicide, or propels from SI into action and behavior, we have also learned about evidence-based risk factors that contribute to this trajectory and variables that may buffer against risk. Beyond addressing risk factors, we must bear in mind the available and modifiable resources within an individual and in society that can be bolstered to protect against overwhelming the system and suicide (see Table 2.2).
Table 2.2 Suicide risk and protective factors
| Risk factors | Protective factors |
|---|---|
| Current suicide ideation | Safe environments |
| Current suicidal intent | Coping skills |
| Current suicidal plan | Problem-solving skills |
| Preparatory behaviors | Meaning and purpose in life |
| Current mental health symptoms | Reasons for living |
| Current alcohol or substance abuse | Social support and connectedness |
| Personal history of suicide attempts | Moral, cultural, or religious beliefs against suicide |
| Family history | Trusting relationship with healthcare provider |
| Caucasian or White race | Access to high-quality healthcare |
| Unmarried | Employment |
| Living alone | |
| Loneliness or lack of social support | |
| Interpersonal loss | |
| Medical illness | |
| Unemployment |
Chapter 3 similarly focuses on the cumulative impacts of stressors and the need for balance and buffering within a system to avoid it being overwhelmed, but from a biological perspective. With the foundational understanding of sociological and psychological perspectives toward suicide, we now transition to how these events, experiences, and perceptions can impact, and at times break down, biological systems and contribute to suicide.