Introduction
In December 2019, a series of respiratory illnesses caused by a novel coronavirus, officially named Coronavirus Disease 2019 (COVID-19), was detected in Wuhan city, Hubei Province of China, and this disease spread rapidly around the country and the world. As of 30 March 2020, 693 282 patients with COVID-19 have been reported, and 33 106 deaths have been confirmed worldwide [1]. The disease is believed to be transmitted mostly via droplets or close contact, and the incubation period ranges from 2 to 14 days [Reference Singhal2]. The typical symptoms are fever, dry cough, myalgia and fatigue [Reference Singhal2]. COVID-19 has the characteristics of rapid transmission, atypical clinical symptoms and easily affecting both lungs, leading to missed diagnoses and misdiagnoses [Reference Huang3–Reference Chang7].
According to the ‘Prevention & Control Program for Novel Coronavirus Pneumonia (Trial) 6th Edition’ enacted by China's National Health Commission [8], close contacts are defined as those who did not use effective protection and had close contact with suspected or confirmed cases 2 days before the onset of symptoms. To date, accumulated evidence has indicated person-to-person transmission to be the cause of most infections [Reference Huang3, Reference Chan9–Reference Phan L11]. Li had demonstrated that person-to-person transmission occurred among close contacts since the mid-December 2019 [Reference Li10].
The massive levels of human movement that occurred during the traditional Chinese New Year holidays fuelled the epidemic. Cases had also been reported in other provinces of China, as well as in other countries with no history of travel to Wuhan, which suggested that local person-to-person transmission was occurring in these areas. At present, a total of 42 confirmed cases of COVID-19 have been reported in Dazhou, Sichuan Province, China, among which are many family cluster cases [12]. With the development of the epidemic, the proportion of clustered outbreaks is increasing. Cluster outbreaks have become a major component of outbreak development throughout the country [13, 14]. It is important to note that while, at present, the number of new cases has recently been reduced in China, they have increased exponentially in other countries, including South Korea, Italy and the United States [Reference Ki15–17], which is a major threat to public health [Reference Deng and Peng18]. Here, we report the epidemiological, clinical, radiological and laboratory findings of a family cluster of five patients and provide guidance for the management of this outbreak.
Methods
Study design and patients
We performed a retrospective study of a family cluster of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection involving five patients admitted to the isolation ward of Dazhou Central Hospital in February 2020. This study was reviewed and approved by the Medical Ethics Committee of Dazhou Central Hospital (approval number 2020014).
Definitions
Determination of cluster epidemic
In reference to the Guidelines for Epidemiological Survey of Cluster Epidemic of COVID-19 (Tentative, 1st edition), a cluster epidemic refers to 2 or more confirmed cases or asymptomatic infected cases identified in a small area (e.g. a family, a construction site, an organisation) within 14 days, and there is the possibility of person-to-person transmission due to close contact or a possibility of infection due to common exposure.
Epidemiological survey
In reference to the Guidelines for Epidemiological Survey of Cluster Epidemic of COVID-19 (Tentative, 1st edition), a first-generation case normally refers to the earliest affected case, i.e., the first case in the cluster epidemic. A second-generation case should generally meet all of the following criteria: (1) history of contact with the first-generation case within 1−14 days prior to disease onset; (2) no history of travel to or residence in Wuhan or its peripheries or other communities reporting any cases and (3) no history of suspected exposure, such as hospital visit, or no evident community transmission in the area where the case was located. To determine a third- or later-generation case, reference can be made to the criteria for determining a second-generation case.
Data collection
We obtained epidemiological, clinical, laboratory, management and outcome data from the hospital's electronic record system. If data missing from the records were needed, we obtained the data by direct communication with the attending physicians and other health care providers. Throat-swab specimens from the upper respiratory tract were obtained from the patients and sent to the Dazhou Centre for Disease Control and Prevention (CDC) to detect COVID-19 by applying quantitative polymerase chain reaction analysis [Reference Huang3]. All patients were tested for respiratory pathogens and for the nucleic acid of influenza viruses A and B. For each case, computed tomography (CT) was performed upon admission. Laboratory assessments include a complete blood count and serum biochemistry.
Diagnostic standard
Diagnoses were performed according to the ‘Diagnosis & Treatment Scheme for Novel Coronavirus Pneumonia (Trial) 6th edition’ enacted by the National Health Commission of the People's Republic of China [19].
Results
General information
The family cluster comprised five patients aged 28–82 years, median age 52 years, including 1 (20%) patient with underlying diseases (hypertension and coronary heart disease) (Table 1).
Table 1. Summary of clinical features and laboratory results of the family cluster infected with COVID-19

WBC, white blood cell; ALT, alanine aminotransferase; AST, aspartate aminotransferase; CKMB, creatine kinase–MB; LDH, lactate dehydrogenase; ESR, erythrocyte sedimentation rate.
Clinical manifestations and epidemiological characteristics
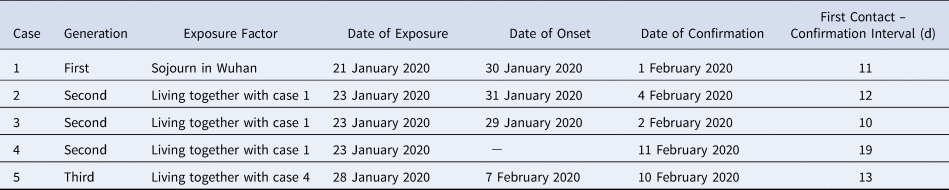
To better understand the transmission characteristics of COVID-19 outside Wuhan city, we carefully clarified the contact history of each case. Case 1 was a 56-year-old woman who had a history of travel to the city of Wuhan, Hubei province, on 21–22 January 2020 (Table 2 and Fig. 1). On 22 January 2020, case 1 returned to Dazhou and stayed with her mother (case 2), daughter (case 3) and daughter-in-law (case 4) from 23 to 27 January 2020. Case 1 developed fever and cough on 30 January 2020. On 28 January 2020, before case 1 showed any symptoms, case 4 had dinner and stayed with her mother (case 5). Cases 2–5 were all local Dazhou residents who had no history of contact with any patient with confirmed or suspected COVID-19 in the previous 14 days. On 1 February 2020, case 1 visited the hospital and tested positive for SARS-CoV-2 infection. The Dazhou CDC responded immediately and put case 1's family members (cases 2–5) in isolation, and they underwent epidemiological investigations and nucleic acid tests. Case 2, 3 and 5 successively developed fever, cough and fatigue symptoms, and were declared positive for SARS-CoV-2 infection on 4, 2 and 10 February, respectively. The nucleic acid test was also positive for case 4. however, she had no symptoms of infection, even during hospitalisation. As an asymptomatic patient, case 4 had transmitted the virus to case 5. This cluster demonstrated the existence of a three-generation transmission chain (Table 2). Of note, one asymptomatic case was found in this study.

Fig. 1. Relationship between the course and transmission of one case in familial cluster outbreak.
Table 2. Familial cluster outbreak of five COVID-19 cases
Radiological and laboratory findings
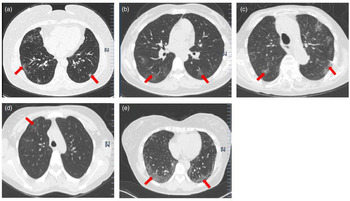
At the time of admission, all the cases had abnormal chest CT findings. As shown in Figure 2, case 1 showed multifocal ground-glass opacity (GGO), predominantly involving subpleural regions of both lung CT scans. Case 2 showed patchy GGO of both lungs. Cases 3 and 5 showed multifocal GGO, especially around the outer bands of the lungs on CT scans, which were compatible with changes observed in viral pneumonia. Case 4 had no clinical symptoms, but chest CT showed patchy GGO in the right upper lobe. As shown in Table 1, all the cases had normal or reduced white blood cell counts, and cases 2–5 developed lymphocytopenia, which was consistent with the main characteristic of viral infection. In terms of inflammation indicators, all the patients on admission presented an elevated serum erythrocyte sedimentation rate (ESR), but no elevated C-reactive protein or procalcitonin. Case 4 had higher levels of bilirubin and lactate dehydrogenase (LDH). The other laboratory test results did not show significant abnormalities.

Fig. 2. Chest CT imaging of case 1 (a), case 2 (b), case 3 (c), case 4 (d) and case 5 (E). (a) CT shows multifocal GGO involving the subpleural regions of both lungs (red arrow). (b) CT shows patchy GGOs of both lungs (red arrow). (c and e) CT shows multifocal patchy GGOs that primarily appear at the peripheral area of both lungs (red arrow). (d) CT shows patchy GGOs in the right upper lobe (red arrow).
Discussion
As of 30 March 2020, more than 80 000 laboratory-confirmed cases of infection with SARS-CoV-2 had been reported in China [20]. The early stage of the COVID-19 epidemic was dominated by sporadic cases. With the expansion and spread of the virus, interpersonal and concentrated transmission has occurred in multiple communities and families across the country. With the gradual reduction of imported cases, the number of second-generation cases is increasing, especially cases of family clusters. In this study, we provide epidemiological and clinical data on a familial cluster of SARS-CoV-2 infection involving five patients in Dazhou, China.
The symptoms of this novel pneumonia were non-specific. As in previous studies, fever, cough and fatigue were the most common onset symptoms [Reference Huang3–Reference Chan9]. Case 3 in this cluster had diarrhoea but no respiratory symptoms and fever. Case 4 had no symptoms during admission, which increased the difficulty of achieving the diagnosis. We speculated that, during transmission, various transmitters would cause different numbers of secondary cases and present varied severity levels of the disease. Furthermore, the immune response among patients varies due to great individual differences. Differences in clinical symptoms therefore arise. Nevertheless, these atypical initial symptoms also deserve attention similar to the more common symptoms. For instance, there have been reports of patients with COVID-19 presenting with diarrhoea as the initial symptom of illness onset [Reference Wang21]. Previous studies have found the levels of ESR and LDH increased in asymptomatic patients. In our study, as an asymptomatic patient, laboratory findings of case 4 had abnormalities in indicators such as raised bilirubin, ESR and slightly raised LDH. Notably, compared with symptomatic patients, these indicators soon returned to normal during our follow-up [Reference Ma22, Reference Wu23]. As with viral pneumonia due to other aetiologies, patients infected by COVID-19 show CT manifestation of GGO in the lungs [Reference Huang3–Reference Chang7, Reference Wang21, Reference Xu24].
In this familial cluster outbreak, case 1 had a history of exposure in Wuhan and could be defined as the source of infection for this outbreak. Case 3 had the onset before the primary case; thus, we can conclude that primary cases are infectious in the incubation period. Of the 3063 tourists tested for SARS-CoV-2 on the ‘Diamond Princess’ 328 had been reported as having asymptomatic cases of coronavirus infection, which suggests a large number of infected individuals with no or slight symptoms [Reference Mizumoto25]. Zou et al. had found that the viral loads of symptomatic and asymptomatic patients were similar, which suggest the transmission potential of asymptomatic patients [Reference Zou26]. We further provide evidence for transmission from an asymptomatic infector to a cohabiting family member that led to COVID-19 pneumonia. These findings indicate that asymptomatic infectors could cause person-to-person transmission, and they should therefore be considered sources of COVID-19 infection. By screening close contacts with a nucleic acid test, which is the main diagnostic indicator, we could locate patients, especially asymptomatic carriers as soon as possible.
Currently, with the resumption of business and education, massive crowd, movements and hence contact, inevitably take place. Moreover, the number of imported backflow cases has also been growing, which objectively provides an opportunity for the novel coronavirus to spread. Therefore, although the confirmed cases of COVID-19 have declined, we should continue to maintain the intensity of scrutiny and investigation for potential cases, paying significant attention to the potential risk of clustering among various groups so as to prevent the domestic epidemiological trend from rising for the second time.
Acknowledgements
The authors thank Fanwei Zeng, Fanxin Zeng, Chun Liu, Cheng Liu, Wenlai Zhou and Lin Xu (Dazhou Central Hospital) for supporting this study.
Conflict of interest
None.
Data availability statements
The data that support the findings of this study are available from the corresponding author, S.Y., upon reasonable request.