Book contents
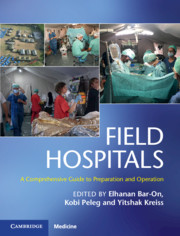
- Field Hospitals
- Field Hospitals
- Copyright page
- Contents
- Contributors
- Preface
- Section 1 History
- Section 2 Scenarios
- Section 3 Operational Considerations
- Section 4 Clinical Considerations
- Chapter 13 Advanced Triage Management for Emergency Medical Teams
- Chapter 14 Medical Aspects in a Field Hospital
- Chapter 15 Pediatrics in a Field Hospital
- Chapter 16 Surgery in a Field Hospital
- Chapter 17 Wound Management in a Field Hospital Environment
- Chapter 18 Orthopedics in a Field Hospital
- Chapter 19 Burn Care in a Field Hospital Environment
- Chapter 20 Obstetrics and Gynecology in a Field Hospital
- Chapter 21 Otolaryngology and Maxillofacial Surgery in a Field Hospital
- Chapter 22 Ophthalmology in a Field Hospital
- Chapter 23 Anesthesia and Pain Management in Field Hospitals
- Chapter 24 Intensive Care Unit Buildup Within a Field Hospital Setting
- Chapter 25 Infectious Diseases and Public Health in a Field Hospital
- Chapter 26 Primary and Ambulatory Care in a Field Hospital in Disaster Areas
- Chapter 27 Mental Health in a Field Hospital
- Chapter 28 Nursing in a Field Hospital
- Section 5 Additional Contextual Considerations
- Index
- Plate Section (PDF Only)
- References
Chapter 27 - Mental Health in a Field Hospital
from Section 4 - Clinical Considerations
Published online by Cambridge University Press: 09 January 2020
- Field Hospitals
- Field Hospitals
- Copyright page
- Contents
- Contributors
- Preface
- Section 1 History
- Section 2 Scenarios
- Section 3 Operational Considerations
- Section 4 Clinical Considerations
- Chapter 13 Advanced Triage Management for Emergency Medical Teams
- Chapter 14 Medical Aspects in a Field Hospital
- Chapter 15 Pediatrics in a Field Hospital
- Chapter 16 Surgery in a Field Hospital
- Chapter 17 Wound Management in a Field Hospital Environment
- Chapter 18 Orthopedics in a Field Hospital
- Chapter 19 Burn Care in a Field Hospital Environment
- Chapter 20 Obstetrics and Gynecology in a Field Hospital
- Chapter 21 Otolaryngology and Maxillofacial Surgery in a Field Hospital
- Chapter 22 Ophthalmology in a Field Hospital
- Chapter 23 Anesthesia and Pain Management in Field Hospitals
- Chapter 24 Intensive Care Unit Buildup Within a Field Hospital Setting
- Chapter 25 Infectious Diseases and Public Health in a Field Hospital
- Chapter 26 Primary and Ambulatory Care in a Field Hospital in Disaster Areas
- Chapter 27 Mental Health in a Field Hospital
- Chapter 28 Nursing in a Field Hospital
- Section 5 Additional Contextual Considerations
- Index
- Plate Section (PDF Only)
- References
Summary
Working in a field hospital after manmade or nature disasters is a demanding mission, known to cause various physical and mental bad outcomes, from depression to post-traumatic stress disorder. The mental health professional (MHP) is critical for every field hospital and humanitarian missions. At the immediate aftermath of the trauma, his or her main mission is to help the other teams to cope with the sights and difficult decision making and, in later stages, the role is enlarged to helping the coping of disaster casualties as well as community leaders. The MHP’s part starts prior to leaving for the mission, with building the team’s resiliency, and ends weeks after coming back from the mission making sure no personnel suffers from secondary traumatization. The demands from the MHP varies when the mission is in high resources country versus low ones, with its differences on the hospital teams condition, urgency, and mental and physical load. Yet, he or she would always have a place in working with the teams during working hours and in a daily closure (through a modified debriefing), liaisons, and actual patient’s treatment, and that should be his or her main mission in field hospital activity.
- Type
- Chapter
- Information
- Field HospitalsA Comprehensive Guide to Preparation and Operation, pp. 262 - 268Publisher: Cambridge University PressPrint publication year: 2020