Introduction
Adults who engage in regular physical activity (PA) have lower rates of diabetes, obesity, hypertension, depression, stroke, cardiovascular disease and premature death (Lee et al., Reference Lee, Shiroma, Lobelo, Puska, Blair and Katzmarzyk2012). For adults and older adults the recommended level of PA is at least 150 min of moderate-to-vigorous physical activity (MVPA) or 75 min of vigorous PA weekly, or a combination of both, which can be achieved in 10 min bouts [World Health Organisation, 2010; Department of Health (DoH), 2011]. Levels of PA decrease with age. This is pertinent issue as PA can also help prevent loss of independence, frailty and cognitive decline in older adults (Mcgowan et al., Reference Mcgowan, Devereux-Fitzgerald, Powell and French2017). A total of 71% of men and 66% of women aged 35–44 report meeting the DoH recommendations; however, by the age of 65–74 this falls to only 58% of men and 52% of women (Health Survey for England, 2012). Objective PA measurements suggest that in reality far fewer people are meeting these recommendations (Health Survey for England, 2008).
Walking is considered one of the best forms of PA; it is convenient, low impact, and develops and sustains physical fitness (Morris and Hardman, Reference Morris and Hardman1997). Trials have demonstrated the success of pedometer interventions for increasing walking (Bravata et al., Reference Bravata, Smith-Spangler, Sundaram, Gienger, Lin, Lewis, Stave, Olkin and Sirard2007; Harris et al., Reference Harris, Kerry, Victor, Ekelund, Woodcock, Iliffe, Whincup, Beighton, Ussher, Limb, David, Brewin, Adams, Rogers and Cook2015; Harris et al., Reference Harris, Kerry, Limb, Victor, Iliffe, Ussher, Whincup, Ekelund, Fox-Rushby, Furness, Anokye, Ibison, Dewilde, David, Howard, Dale, Smith and Cook2017). However, little is known about the long-term sustainability of interventions which aim to promote PA, with a meta-analysis (Hobbs et al., Reference Hobbs, Godfrey, Lara, Errington, Meyer, Rochester, White, Mathers and Sniehotta2013) and Cochrane review (Richards et al., Reference Richards, Hillsdon, Thorogood and Foster2013) calling for more trials with longer follow-up. There is evidence that PA disengagement typically occurs about six to seven months after an intervention has ended (Martin and Sinden, Reference Martin and Sinden2001; Hillsdon et al., Reference Hillsdon, Foster and Thorogood2005). For PA to result in sustained health benefits it needs to be practised on an ongoing basis (Reiner et al., Reference Reiner, Niermann, Jekauc and Woll2013); therefore greater emphasis needs to be placed on interventions which promote PA maintenance. There is no accepted definition of post-trial PA level maintenance (Kahlert, Reference Kahlert2015). One frequently used definition of successful maintenance is participating in regular PA for six months post-intervention (Rhodes et al., Reference Rhodes, Plotnikoff and Courneya2008). We extend this definition to include what people are doing/can do to remain physically active in the longer term (ie, beyond the six months usually referred to).
Whilst several studies have explored the features of interventions associated with the long-term effectiveness of PA interventions (O’brien et al., Reference O’brien, Mcdonald, Araujo-Soares, Lara, Errington, Godfrey, Meyer, Rochester, Mathers, White and Sniehotta2015) there has been very little research exploring the specific factors that motivate individuals to sustain PA post-intervention. Previous research into these factors has focussed on the barriers and facilitators to engaging in PA (Horne and Tierney, Reference Horne and Tierney2012; Mailey et al., Reference Mailey, Huberty, Dinkel and Mcauley2014; Alvarado et al., Reference Alvarado, Murphy and Guell2015; Martins et al., Reference Martins, Marques, Sarmento and Carreiro Da Costa2015). Additional research to distinguish what factors lead to successful and unsuccessful PA maintenance has been recommended (Marcus et al., Reference Marcus, Dubbert, Forsyth, Mckenzie, Stone, Dunn and Blair2000; Boutelle et al., Reference Boutelle, Jeffery and French2004).
Background to the Pedometer And Consultation Evaluation (PACE-UP) trial and three-year follow-up
PACE-UP was a three-arm randomised control trial undertaken in seven general practices in South West London, United Kingdom. It recruited between October 2012 and October 2013, with 12-month follow-up completed by October 2014. The aim was to increase PA levels in inactive patients (those not achieving current UK PA guidelines) aged 45–75 years, using a complex intervention based on pedometer step-count feedback with and without practice nurse PA consultations (Harris et al., Reference Harris, Kerry, Limb, Victor, Iliffe, Ussher, Whincup, Ekelund, Fox-Rushby, Furness, Anokye, Ibison, Dewilde, David, Howard, Dale, Smith and Cook2017).
One intervention arm (n=346) received a pedometer and diary and three individually tailored PA practice nurse consultations towards following a 12-week walking-based programme using behaviour change techniques such as self-monitoring, goal setting, boosting motivation and anticipation of setbacks. The second arm (n=339) were posted out a pedometer, PA handbook, a diary and written instructions for a 12-week pedometer-based walking programme, based on individual baseline blinded pedometer step-count. There were no meetings with the practice nurse in this arm. Both intervention arms were asked to post back completed diaries after the three-month intervention. The control arm (n=338) continued with their usual PA. After the 12-month follow-up, the control arm participants were offered the intervention; 66% chose to have the pedometer, handbook and diary posted to them and 20% opted for a nurse appointment to discuss their PA, where they also received these materials.
Results at 12 months showed that participants in the nurse and postal arms achieved statistically and clinically significantly higher levels of PA both in terms of step-count and accelerometer-assessed minutes spent in MVPA compared with the control group, and that there was no significant difference in PA levels between the two intervention arms. However, the nurse group had significantly greater confidence in their ability to exercise compared with the other two groups; this may be an important factor in longer-term PA maintenance (Harris et al., Reference Harris, Kerry, Limb, Victor, Iliffe, Ussher, Whincup, Ekelund, Fox-Rushby, Furness, Anokye, Ibison, Dewilde, David, Howard, Dale, Smith and Cook2017). After the 12-month follow-up, qualitative work explored the initial barriers and facilitators to increasing PA levels for participants in both intervention arms (Normansell et al., Reference Normansell, Smith, Victor, Cook, Kerry, Iliffe, Ussher, Fox-Rushby, Whincup and Harris2014). Important barriers identified included poor physical health, mistrust of monitoring equipment, an inflexible routine, work and other commitments, and bad weather. Facilitators included desire for a healthy lifestyle, a flexible routine, social support and a belief in the importance of PA for health.
Three-year follow-up qualitative evaluation
Aim of the study
The three-year PACE-UP follow-up, conducted from October 2015 to November 2016, aimed to determine whether participants’ PA levels had been sustained beyond 12 months.
The aim of the qualitative evaluation was to examine the facilitators and barriers associated with PA maintenance three years post-intervention and to explore what resources could aid PA maintenance.
Methods
Sampling and recruitment
The trial statistician randomly sampled the three trial arms for participants who had completed a three-year follow-up and had consented to be approached for interview. Although aware of which group the participant was in, the interviewers were blinded to participants’ PA levels both during the trial and at three-year follow-up.
Participants were contacted via email and telephone to arrange a telephone interview with either CW or CB. Prior to the interview, participants were reminded of consent to be interviewed, assured of anonymity and confidentiality, and reassured that they were free to stop the interview at anytime without providing a reason. If happy to continue, consent was then sought for the interview to be audio-recorded. Stratification within each of the participant groups ensured that the interview sample included both genders and represented a range of ages and ethnicities. On completion of the interview, participants were offered a £10 high-street gift voucher to thank them for taking part.
Interview schedule
The interview schedules were developed through discussions with the qualitative team (TH, CW, CB, CV and RN). There were slight differences between the questions asked to the intervention groups (postal and nurse) and to the control group participants (see Appendix 1). After the first few interviews, recordings were shared with the team and interview questions were refined to include some open questions and to make some questions clearer.
Analysis
Interviews were transcribed verbatim by an external source, checked for accuracy and potential identifying features were removed. Early transcripts were circulated to the research team to ensure consistency between the interviewers and to help assess when data saturation had been reached. The data were then analysed using thematic analysis (Braun and Clarke, Reference Braun and Clarke2006). The analysis took a semantic approach with the themes identified using the ‘explicit or surface meanings of the data’ (Braun and Clarke, Reference Braun and Clarke2006: 84) and did not attempt to provide an in-depth conceptual description and understanding, therefore staying ‘closer’ to the data obtained (Neergaard et al., Reference Neergaard, Olesen, Andersen and Sondergaard2009). Transcripts were read repeatedly by CW and CB and coding was initially of phrases or words which captured the participant’s feelings about the trial. Where there was consensus about the emerging phrases or words they were clustered in themes. An inductive approach was used to see which themes arose naturally from the data, rather than having prescribed categories.
Findings
Between March and April 2016, 105 participants were randomly selected, 96 were contacted and all agreed to participate.Footnote 1 Telephone interviews were arranged and undertaken with 60 participants (20 from each-arm of the trial). Although data saturation was achieved before completing the 60 interviews, recruitment continued to ensure views from participants of different demographic profiles. Of those recruited 70% were aged 60–75 years old, 62% female and 87% White. Interviews lasted between 4 and 22 min (median 10 min, mean 11 min). One participant had difficulty hearing, so they were emailed the questions to complete.
Two key themes and related sub-themes were identified from the analyses which will now be presented and illustrated with verbatim quotes (below, with additional supporting quotes in Appendix 2). Participants also reflected on what additional resources they would find useful to support PA maintenance.
Long-term effect of the PACE-UP trial
Within this key theme, three sub-themes were identified (Figure 1); increased awareness, lifestyle changes and pedometer use.
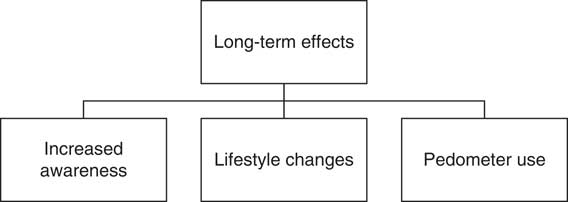
Figure 1 Three sub-themes relating to the long-term effect of the PACE-UP trial
Increased awareness
The majority of participants felt since the PACE-UP trial they had an awareness of PA, regardless of whether they thought the trial had actually changed their PA levels. Some participants described developing an awareness of the importance of PA and how much PA they should be doing:
I think it’s made me more aware of the need to walk more but discipline the PACE-UP trial has provided I suppose, in terms of monitoring how many steps I do per day, and what you actually need to do to achieve that number of steps per day, it’s made me more aware of the need to actually commit to doing some exercise a day, just strolling around the house, and going to the shops occasionally doesn’t really make much difference. It doesn’t meet the sort of threshold that you need to reach to ensure that you lead a healthy lifestyle, so I think it’s the discipline of PACE-UP has had an effect on my perception of health and wellbeing.
(Male, aged 56, white British, postal group)
Others described having a better understanding of the amount and intensity of PA needed to meet the guidelines and how this can be built up gradually over the day:
… it has given me a lot of insight and support really , doing small amounts of physical activity regularly has been you know/having the pace-o-meter on … it made a huge difference as opposed to the mind set of, oh, I’ve got to do an hour in the gym. Actually 10 minutes solid walking somewhere, several times a day, actually builds stuff up …. it’s given me insight and therefore changed the mindset … its actually also given me confidence … and support in a curious kind of way. I just feel, when I’m down, and I think oh God, I’m too tired to do anything, it actually boosts me on that kind of level, on the motivational level.
(Female, aged 69, white British, nurse group)
Lifestyle changes
Participants attributed a number of positive lifestyle changes to being involved in the PACE-UP trial, including walking rather than using motorised transport, walking during work lunch breaks and walking up escalators:
I make myself walk more than I did before because it was very easy to you know catch the bus and come back on the bus, whereas now I rarely catch the bus down [the hill]. I’m always walking.
(Female, aged 63, white British, postal group)
Well it just sort of sprung me in to action with regard to doing a little bit of walking every day, so I try to incorporate at least 10 minutes, but ideally at least 15, at lunch time … I’ll just mosey around the block a couple of times from work and it has made me feel a lot better.
(Female, aged 60, white Irish, postal group)
There was some indication that these lifestyle changes were sustainable in nature:
[PACE-UP] just reinforced the importance of just keeping up the exercise and just being aware that it’s a lifelong thing now. We’ll just continue like this. Yes, that’s what we’ll do really.
(Male, aged 53, white British, postal group)
Whilst some participants used the above strategies to integrate healthy behaviours into their lifestyle, others explained that an inflexible routine, and a preference for sedentary activities, prevented a positive walking habit formation:
I’m/not exactly inactive, but as soon as I get home from work, the feet go up and you know that’s it. I don’t go anywhere unless I really have to.
(Female, aged 61, white British, postal group)
Pedometer use
Participants had differing views towards the effectiveness of the pedometer intervention for aiding PA maintenance. For some, they felt using the pedometer helped ‘kick-start’ regular PA:
Well, before the PACE-UP trial I had no incentive. And that really did help me. That put me/gave me the first steps as it were, got me on the right track, and then going to the gym and getting somebody there who could set out a routine for me and encourage me and things, next step, and then got the Fit Bit as well at Christmas, and then that’s really helped.
(Female, aged 51, unknown, nurse group)
The participants continuing to use the pedometer post-intervention found it a useful motivational tool for goal setting and self-monitoring:
I try to ensure that I reach 10000 a day, although I don’t always do/achieve that, but I know that that’s my benchmark and therefore if I fall below it I believe I haven’t done enough exercise for that day.
(Male, aged 56, white British, postal group)
For others, they felt using the pedometer increased PA initially but reported the ‘novelty’ of wearing it had worn off. Participants stopped wearing the pedometer for numerous reasons including finding it inconvenient or inaccurate.
I think it made me more aware of walking as a means of health and I was very interested to count how many paces I did per day, that was quite fascinating to count and watch/it’s quite addictive isn’t it, counting … on a long-term basis I can’t keep wearing that thing all the time, it irritates me to wear it and I forget to switch it on and it doesn’t work as a practical method.
(Female, aged 50, white British, postal group)
A minority of participants stated that using the pedometer had a negative impact on them psychologically. Participants commented on feeling demoralised and ‘like a failure’ (Male, aged 63, white British, postal group) if they had not managed to meet each daily step target:
It doesn’t motivate me to do more, but its makes me feel guilty for not doing more.
(Male, aged 56, white British, postal group)
However, although some participants were no longer using the pedometer provided as part of the PACE-UP trial, a few reported using other PA monitoring devices such as mobile phones and Fit-Bits.
I kept forgetting to put the pedometer on, but I always had my phone on me, so I thought well I’ll just use my phone. So it made more sense because I’ve got it handy. And then, when I do go for a walk, it’s nice to have it on me … rather than another piece of equipment
(Female, aged 52, white other, control group)
Facilitators and barriers to PA maintenance
Most of the themes relating to the facilitators and barriers to maintaining PA were the inverse of each other; these included weather/season, health, self-motivation, ageing and social support. Time, was the only theme described as a barrier to maintaining PA and not a facilitator (Figure 2).
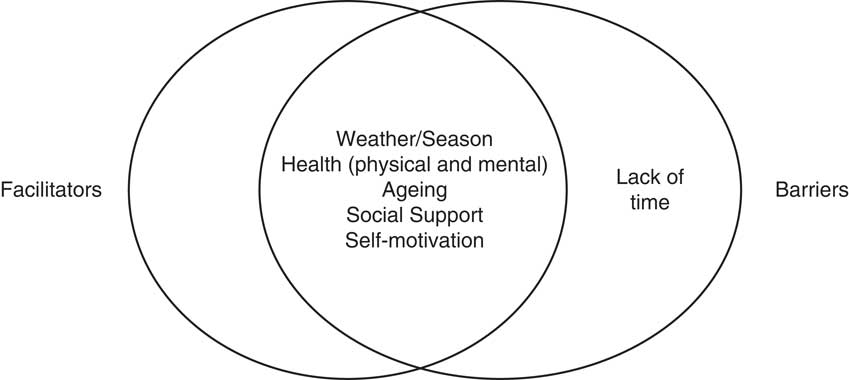
Figure 2 Barriers and facilitators to physical activity maintenance
Weather and season
For many participants, the weather and season were important factors linked to PA motivation and engagement.
It depends on the weather for me … when the weather is fantastic and you wake up and the sun is shining, I can’t wait to get out, and then on the days when you wake up and it’s so grey, the mood just isn’t there.
(Female, aged 63, Caribbean, nurse group)
For some, bad weather prevented undertaking PA, whilst for others PA was guided by the season:
I toyed with the idea of walking in to XXXXX yesterday and I certainly had the time but the rain came down and it put me off.
(Male, aged 64, white British, postal group)
Health (physical and mental)
Health was mentioned by many as a reason for continued engagement in PA. Participants cited the following physical health motivators: keeping fit; preventing long-term health conditions; managing existing health conditions; keeping in shape; losing weight; and helping with an injury. Whilst some participants spoke about general health-related benefits of PA others spoke about specific ailments:
The more active I am, the better the arthritis is, so I know if I’ve sat down for even more than half an hour, when I get up, I’m stiff, so I know to keep myself lubricated. I need to be walking as much as possible and that’s why I swim as well, so that’s my main motivation really, is to just keep the joints as lubricated as possible.
(Female, aged 61, white Irish, postal group)
Participants also spoke about the mental health benefits of PA and how PA makes them feel better, more alert and have a more positive outlook on life.
Physical activity, it’s important, not only for things like weight control, but also for things like reducing the ageing process, but also keeping your mind physically active and … having a better positive view of life, so having a physical exercise routine doesn’t just improve your physical well-being, but it does improve your mental well-being … I certainly do feel more mentally alert and I feel happier after having done some exercise, so I think that’s the take-away for me from the PACE-UP trial is the acknowledgement or the understanding that keeping up some sort of physical routine is good obviously physically, but also good mentally.
(Male, aged 56, white British, postal group)
Having physical limitations was also cited as a barrier to PA. For some this was linked to specific health conditions such as arthritis, whilst for others it was the general aches and pains related to ageing that limited PA:
I’ve got an ongoing problem where I get pain, so there’s no way I’m going to be going out walking if I don’t have to.
(Female, aged 61, white British, postal group)
Concerns about possible adverse health events as a consequence of increasing PA was also seen as a barrier to engagement. One participant was unsure of the safest way to increase their activity levels as they got older and felt there needed to be better advice and guidance:
… I’m just a little bit afraid of becoming more active, simply because you feel that, well, I’m doing quite well with what I’m doing, so what’s the point of sort of having a risk of a heart attack or something like that, suddenly break in to a stride and start running, so maybe a bit of guidance on what’s going to happen to you if you do step up your exercise plan.
(Male, aged 67, white British, postal group)
Self-motivation
Many participants cited self-motivation as an important reason for engaging in PA and a few explained that it was the PACE-UP trial that had provided them with self-motivation.
You started something and then I continued by myself
(Female aged 56, white British, control group)
Whilst some participants reported having the resources (park, gym, etc.) to be active they explained the main barrier to not participating in activity was a lack of self-motivation.
In my area things the resources are there it is just for me to be a bit more committed, a bit more motivated, to do it.
(Female, aged 57, Asian other, control group)
For some, lack of self-motivation was linked to a misconception about the long-term benefits of engaging PA and potential health outcomes:
If somebody turned around to me and said, you’re going to have to walk 10000 steps a day, otherwise you’re going to die in two years’ time, that might do it, but I haven’t got that … I’ve got to do this otherwise it’s a serious serious thing, because I’m not that unfit. I’m just not doing enough really, you should walk 10000 steps a day, and actually I haven’t and I don’t and I know I should.
(Male, aged 56, white British, postal group)
Ageing
Some participants placed importance on PA as a way of staying young and active and trying to slow down the ageing process.
… with advancing years, you’re more aware that/and as the saying goes, if you don’t use it, you lose it, and I’m very much aware of that now.
(Female, aged 73, white British, control group)
A few participants spoke about age as a barrier to PA and how participating in sport had become harder as they got older. For some this was because they found PA ‘more of a strain’ (Female, aged 59, white British, nurse group).
I used to, you know, play squash and I used to coach rugby and I played hockey and things like that, I don’t do those things any more. Sometimes I think I should but it’s/as you get older it gets a bit harder to do them.
(Male, aged 59, white British, control group)
Participants had differing opinions over retirement and whether or not having more leisure time would affect PA levels. Some participants saw not working as an opportunity for additional PA, whereas others felt that not having a daily commute would reduce PA levels.
I work between 30 and 40 hours a week still and I don’t actually have much time for anything else at the moment, nor do I have a lot of energy left. I am aiming to retire in 18 months, when I’m 70, so one of the things that I want to do is to take up swimming and to do more yoga, so it really/my main activities are walking, yoga and swimming, when I take it up, again.
(Female, aged 69, white British, nurse group)
I always walked to work and you know and I wasn’t quite concerned, but when you retire, you start becoming more relaxed and haven’t got the pressure of getting up and doing things straight away, so your lifestyle’s more relaxed, hence, you don’t do [as much] physical exercise as you think you’re doing.
(Female, aged 64, white British, control group)
Social support
Although a few participants stated a preference for solitary activities, many participants spoke about the importance of having friends and family to motivate them to participate in PA. For some, this motivation came from making a commitment to exercise with someone else. For others, social support provided them with confidence to try new activities or encouragement to push themselves further. Support from and accountability to family and friends were therefore seen as common facilitators to PA.
… I do have a friend that I walk with on a Thursday, so I’ll say, ooh, I don’t really feel like walking today and she’ll say, oh come on, get a move on, and she’ll/we’ll just both say oh shall we walk just a little bit further and we’ll walk a little bit further, or you know/or push each other up the hill in a way, so we motivate each other …
(Female, aged 52, white other, control group)
PA was also seen as an opportunity to meet new people:
There isn’t much reward coming from the physical activity, there has to be something else rewarding really … I think/well the social thing is one thing that actually helps really. That keeps me going to the class.
(Female, aged 69, white British, control group)
Family members were also seen as indirect motivators with some participants expressing a desire to keep up with younger family members as an incentive to maintain an active, healthy lifestyle.
To remain independent, and I’ve got nieces and a nephew … I need to be active to keep up with them because they are young. I just need to keep up with everyone else really. I don’t want to slow down and become old. Unfortunately, I’m not really motivated by anything else.
(Female, aged 65, white British, nurse group)
A few participants spoke about how participating in the trial had positively influenced the PA of those around them:
It’s been beneficial for me and to friends … I’ve got a particular friend that used to never worry about steps, but now talks about steps all the time, and that’s partly through my talking about my own experience with PACE-UP.
(Male, aged 56, white British, postal group)
In contrast, not having anyone with whom to participate in activity was seen as a barrier, with participants reporting that lack of social support led to a reduction in walking:
I like walking but my friend that I used to go walking with quite a lot has moved away, so there’s not so much incentive now to go for a walk.
(Female, aged 59, white British, nurse group)
Lack of time
Time was identified as a barrier by nearly half of participants, making it the most frequently cited barrier, and was the only theme not identified as a facilitator. Lack of time included being ‘too busy’, ‘family responsibilities’ (looking after children, caring for relatives) and ‘work commitments’.
To me my reluctance to do physical activity was really based on I’d say laziness … and if you are working full time … it takes discipline I think to do things in a time when you’re supposed/you should be relaxing after work, the thought of actually doing physical exercise, which didn’t at the time seem to me to be a relaxing activity, but a chore, deterred me from doing any physical exercise really.
(Male, aged 56, white British, postal group)
Even though some participants had a strong sense of self-motivation to participate in PA, time was still the limiting factor to them engaging in this behaviour.
It’s not because I don’t want to do the exercise, or … or that I haven’t got the motivation to do it, it is just finding time.
(Female, aged 54, white British, nurse group)
Some participants were able to find solutions to having a lack of time, including integrating physical activity into their schedule.
…I do have an issue of time really, which is why I find walking to and from school is quite a good thing because it makes me have exercise and it’s killing two birds with one stone, because it’s something that needs to be done as well.
(Female, aged 49, white British, postal group)
As seen in a previous quote, others were able to overcome the barrier of time by incorporating multiple short bouts of PA into each day.
Oh I’ve got to do an hour in the gym. Actually 10 minutes solid walking somewhere, several times a day, actually builds stuff up.
(Female, aged 69, white British, nurse group)
Reflections from trial participants
At the end of the interview participants were asked to comment on what additional support could be provided to aid PA maintenance, and were offered examples which included; text messaging, online resources, annual nurse appointments and walking groups. Participants also provided other useful suggestions.
Annual nurse appointments
Overall participants were positive about the option of seeing a nurse annually to discuss their PA. Participants felt having a nurse (or an authoritative figure) to report to regularly would provide ‘accountability’ and remind them to participate in/undertake/maintain PA levels.
I was probably more motivated through the trial than I was once that stopped, so if I had a regular point/an appointment that meant I checked in with somebody on a regular basis, I’d probably be more motivated, so external accountability has always been quite useful.
(Male, aged 66, white British, nurse group)
Walking groups
Again the role of social support was viewed as helpful to engaging in PA. However, it was important to participants that walking groups included people of similar fitness levels and were at a convenient time.
I suppose maybe if there were walking groups around for people I mean I know there are walking groups, but they’re usually for people who are fitter than me.
(Female, aged 68, white British, postal group)
Some participants viewed organised walking groups as too restrictive and would prefer to be part of a group that was ‘more spontaneous than arranged’ (Male, aged 67, white British, postal group).
Text messages and online resources
Participants had differing opinions over the use of text messages and online resources to encourage PA maintenance, with some having a strong preference for one over the other.
Some participants favoured the idea of being able to go online at their ‘own time’ (Female, aged 63, white British, control group) to find PA guidance and viewed text messages as ‘intrusive’ (Male, aged 56, white British, postal group) and a ‘nuisance’ (Female, aged 52, white other, nurse group).
Others preferred the idea of regular text message reminders to be physically active and felt that they would be less likely to view online resources as that required them to be ‘a bit more proactive’ (Female, aged 51, unknown, nurse group).
Additional ideas suggested by participants
A few participants spoke about the value of a more holistic nurse consultation, suggesting nurses include advice and information on diet as well as PA:
… if you wanted any thoughts about the trial and how it could be, not necessarily improved, but how it could be adapted slightly to talk about diet as well, because I think that the two go hand in hand, the exercise and the diet.
(Female, aged 50, white British, nurse group)
Others spoke about a need for more opportunities for older people to participate in PA and difficulty with some established activities:
I think it would be good if there was some sort of community, like a walk once a week …, if you’re a bit older, it becomes a little bit difficult to join particular classes.
(Male, aged 56, white British, postal group)
Some participants felt there were no additional resources that could be provided to encourage PA maintenance and that being active was ultimately down to self-motivation.
These days one gets plenty of messages about being physically active. I don’t think/if people are not active it’s not because they don’t know they should be, and that certainly applies to me, out of inertia, laziness, busyness, you know, there are all sorts of reasons why I’m not as active as I could be, but it’s not because you don’t give me the information or anything like that.
(Male, aged 59, white British, control group)
Discussion
Main findings
This qualitative evaluation identified perceived barriers and facilitators to being physically active three years after participants took part in a PA intervention. An important finding was that the results of each theme were consistent across the three arms of the trial (nurse, postal and control) with no group differences emerging. Most participants reported an increased awareness of PA as well as an increased understanding about the importance of PA for health and knowledge about the amount of PA required to meet PA guidelines. Participants highlighted different barriers and facilitators to being able to stay physically active in the longer term, which were predominantly the inverse of each other and were similar across the three groups. Important facilitators and barriers included: weather; health; self-motivation; ageing; and social support. Lack of time was the most frequently cited barrier to maintaining PA. Participants provided useful insights on what additional resources could encourage them to stay physically active in the longer term.
Comparison with other studies
To our knowledge, this is the first qualitative study to explore the barriers and facilitators to PA maintenance three years after a PA walking intervention has been delivered.
Interestingly, the majority of barriers and facilitators found in this study were also reported in the previous qualitative exploration of reasons for participating in the PACE-UP trial (Normansell et al., Reference Normansell, Smith, Victor, Cook, Kerry, Iliffe, Ussher, Fox-Rushby, Whincup and Harris2014). This provides support for the credibility of our work and suggests that barriers and facilitators may be similar for both PA adoption and maintenance (Tulloch et al., Reference Tulloch, Sweet, Fortier, Capstick, Kenny and Sigal2013).
Of note, time as a facilitator (as well as a barrier) emerged from the 12-month interview data, with participants reporting the benefits of having a flexible routine which allowed them to fit in more PA. In this study, time was the most frequently stated barrier to PA, this is consistent previous research (Kowal and Fortier, Reference Kowal and Fortier2007; Reichert et al., Reference Reichert, Barros, Domingues and Hallal2007; Evenson et al., Reference Evenson, Moos, Carrier and Siega-Riz2008; Costello et al., Reference Costello, Kafchinski, Vrazel and Sullivan2011; Kelly et al., Reference Kelly, Martin, Kuhn, Cowan, Brayne and Lafortune2016). Whilst we found that time was not identified as a facilitator, some participants were able to find strategies to overcome it as a barrier.
A systematic review, which explored barriers and facilitators to the uptake and maintenance of healthy behaviours by mid-life adults, also reported similar findings to our study. Additional barriers and facilitators identified in the review included; socio-economic status (SES), ethnicity, gender and transport issues (Kelly et al., Reference Kelly, Martin, Kuhn, Cowan, Brayne and Lafortune2016). Consistent with our findings Kelly et al. (Reference Kelly, Martin, Kuhn, Cowan, Brayne and Lafortune2016) also found health to be both a facilitator and a barrier to PA. Fear of illness and ageing, previous illness and other health-related issues (eg, weight loss, feel good factor) were recognised as facilitators. Conversely, existing ailments or chronic health conditions were cited as barriers to PA. Whilst we did not find any differences in terms of age, previous studies have found health to be more frequently cited, as a barrier to PA, with increasing age (Booth et al., Reference Booth, Bauman, Owen and Gore1997; Sørensen and Gill, Reference Sørensen and Gill2008).
Consistent with a study exploring the effectiveness of a pedometer to increase PA in primary care six months post-intervention (Mckay et al., Reference Mckay, Wright, Lowry, Steele, Ryde and Mutrie2009), our participants spoke about the pedometer helping initially until the novelty of wearing it had worn off or until they found other ways to monitor PA.
Social support has been found to be important for both behaviour initiation and maintenance (Mcauley et al., Reference Mcauley, Jerome, Elavsky, Marquez and Ramsey2003; Floegel et al., Reference Floegel, Giacobbi, Dzierzewski, Aiken-Morgan, Roberts, Mccrae, Marsiske and Buman2015). In our study, social support was associated with remaining physically active in the longer term. Other participants spoke about lack of social support being a barrier to PA, explaining they were less likely to engage in PA if they did not have a companion. Kelly et al. (Reference Kelly, Martin, Kuhn, Cowan, Brayne and Lafortune2016) included studies that identified social support as a facilitator (Hooker et al., Reference Hooker, Wilcox, Rheaume, Burroughs and Friedman2011; Babakus and Thompson, Reference Babakus and Thompson2012) and those that identified lack of social support as a barrier (Im et al., Reference Im, Ko, Hwang, Chee, Stuifbergen, Walker and Brown2013). Whilst we had too few participants from different ethnic groups to comment on important effects, cultural and ethnic differences can help to explain why some people place more importance on social support, in terms of PA, than others. The notion of ‘individual-versus family oriented PA’ has been well documented in the literature (Berg et al., Reference Berg, Cromwell and Arnett2002; Belza et al., Reference Belza, Walwick, Shiu-Thornton, Schwartz, Taylor and Logerfo2004). One study found that ethnic minority women place more value on the role of family-orientated activities than white women (Im et al., Reference Im, Ko, Hwang, Chee, Stuifbergen, Walker and Brown2013).
One recurring topic across themes was having someone to report to regularly motivated individuals to participate in PA. Frequent contact with participants during the maintenance phase of an intervention has been found to be important (Marcus et al., Reference Marcus, Dubbert, Forsyth, Mckenzie, Stone, Dunn and Blair2000); however, little is known about what needs to happen during these contacts, the frequency they need to occur and at what point they can cease and behaviour still be maintained. Participants in our study had differing opinions over what additional support could have been provided to encourage PA. This highlights the need for some aspects of the PA interventions to be tailored to the individual. Previous research states that for behaviour change to be successful strategies need to be developed by gender, age, risk status, ethnicity and baseline activity (Marcus et al., Reference Marcus, Dubbert, Forsyth, Mckenzie, Stone, Dunn and Blair2000; Berg et al., Reference Berg, Cromwell and Arnett2002; Sørensen and Gill, Reference Sørensen and Gill2008). Maintenance of PA following the end of an intervention may also be influenced by attitudes and behaviours, as well as pre-existing individual characteristics (Bock et al., Reference Bock, Marcus, Pinto and Forsyth2001).
Strengths and limitations
We were able to recruit and interview a large sample of participants (n=60). Participants included both men and women of varying ages. Everyone who we managed to successfully make contact with agreed to take part in the interview indicating an excellent take-up rate.
Qualitative research is based on researchers’ interpretations, and therefore open to researcher bias (Mays and Pope, Reference Mays and Pope1995). The researchers undertaking the analysis were aware of the facilitators and barriers identified from qualitative interviews at 12 months (Normansell et al., Reference Normansell, Smith, Victor, Cook, Kerry, Iliffe, Ussher, Fox-Rushby, Whincup and Harris2014). It was important that, while undertaking the data analysis, the researchers avoided the unconscious ‘seeing’ of data they expected to find (Crabtree and Miller, Reference Crabtree and Miller1999) and did not force the data into preconceived categories (Charmaz, Reference Charmaz2006). We mitigated these risks by conducting the interviews and transcriptions by two researchers working independently (CB and CW). Emergent themes were discussed, circulated to the larger research group and any discrepancies were resolved through discussion. Having the wider team actively involved in the analysis increased credibility and trustworthiness of the data interpretation (Noble and Smith, Reference Noble and Smith2015). Illustrative verbatim quotes are provided for each sub-theme to demonstrate the relationship between the interpretation and the evidence increasing trustworthiness.
Limitations of this research should also be acknowledged. The PACE-UP trial, from which the participants were sampled, was conducted in South West London. Although a diverse area in terms of ethnicity and SES, care should be taken when transferring the findings to a wider context, especially as those interviewed were mostly Caucasian. As with all research, our findings only represent the views of those who consented to be contacted. Whilst we made contact with those declining to participate in the PACE-UP main trial to explore reasons for non-participation (Normansell et al., Reference Normansell, Holmes, Victor, Cook, Kerry, Iliffe, Ussher, Fox-Rushby, Whincup and Harris2016), we did not attempt to contact those declining to take part in the three-year follow-up. Our findings therefore only represent those participants that continued with the PACE-UP trial at three years. Participants who did not consent to be interviewed or who dropped out from the follow-up might have differing views and issues surrounding PA maintenance that we were unable to capture. Our exploratory between-group comparisons may also be limited by contamination of the control group after 12 months following all participants being offered a PA intervention.
We acknowledged the potential influence that being aware of the findings from the previous qualitative study, carried out shortly after the PACE-UP intervention was delivered (Normansell et al., Reference Normansell, Smith, Victor, Cook, Kerry, Iliffe, Ussher, Fox-Rushby, Whincup and Harris2014), could have had upon our interpretation and analysis. We adopted strategies to mitigate this. However, one further strategy to minimise ‘researcher bias’ that we would seek to include in future research would be a wider discussion of results with either study participants, experts by experience (those who do/do not exercise) and those involved in service delivery.
We did not attempt to correlate participants’ views with any objective measure of PA and interviewed participants without knowledge of their objective PA levels, either earlier on in the trial, or at the three-year follow-up. This was a deliberate decision for a number of reasons; first, PA levels can vary over time and during different seasons; second, we were interviewing participants over a short time period (March to April 2016); whilst their most recent objective PA monitoring from the three-year follow-up could have been anytime between October 2015 and March 2016. Finally, the length of time between providing objective three-year follow-up data and being interviewed differed for different participants.
Implications
Identifying reliable predictors of PA allows researchers and practitioners to structure interventions effectively to influence long-term behaviour change. Given that many participants mentioned an increased awareness of the importance of PA three years post-intervention, the challenge is how to translate this knowledge into sustainable behaviour change.
Future research needs to focus on techniques to overcome barriers to PA. For example, addressing lack of time by better incorporating PA into daily life or by considering strategies for prioritising PA when there are competing sedentary activities. Efforts to overcome lack of time, should consider the DoH guidelines suggesting that the recommended 150 min of MVPA a week can be achieved in bouts of just 10 min or more, for example, brisk walking is a good way of integrating PA into daily life. Many participants in our study attributed positive lifestyle changes to the PACE-UP trial, for example, walking rather than using motorised transport. For those who cited time as a barrier, providing them with examples of how others have successfully integrated PA into their daily routine and made sustained behaviour changes, may be beneficial. Previous research supports this suggestion, demonstrating that PA advice from realistic exercise leaders, or role models in the community, is potentially more effective in encouraging PA participation than advice from unrealistic role models (Allender et al., Reference Allender, Cowburn and Foster2006; Buman et al., Reference Buman, Giacobbi, Dzierzewski, Aiken Morgan, Mccrae, Roberts and Marsiske2011).
Participant’s had differing opinions over whether retirement would increase or decrease PA levels and this posits whether retirement, as a transitional point in life, could provide a key opportunity to deliver PA interventions to improve health (Baxter et al., Reference Baxter, Johnson, Payne, Buckley-Woods, Blank, Hock, Daley, Taylor, Pavey, Mountain and Goyder2016). Whilst we did not unpick the relationship between mid-life/older and retired/working individuals it would be interesting to see whether different barriers and facilitators are important for these participant groups.
Another challenge is how to transform PA barriers to facilitators, for example, demonstrating the value of PA for many chronic health conditions to change this from inhibiting to promoting PA. Efforts to increase PA need to focus on increasing awareness and confidence about the levels of exercise and types of activities that are not only safe, but may be beneficial for specific health conditions that become more common as people age (Sharma et al., Reference Sharma, Sargent and Stacy2005; Kaewthummanukul and Brown, Reference Kaewthummanukul and Brown2006).
Conclusion
Interviews with 60 participants three years after taking part in a PA intervention revealed that most reported an increased awareness of PA, regardless of whether they had been in one of the intervention groups or the control groups. They also identified perceived barriers and facilitators to being physically active and provided constructive ideas for encouraging PA maintenance which could be incorporated into future interventions. A challenge for future PA interventions is how to transform barriers into facilitators, for example, educating participants about the value of PA for many chronic health conditions, to change this from inhibiting, to promoting PA.
Acknowledgements
The research was supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care South London at King’s College Hospital NHS Foundation Trust. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the DoH. The authors would like to thank the South West London (UK) general practices who supported this study: Upper Tooting Road Practice, Tooting; Chatfield Practice, Battersea; Wrythe Green Practice, Carshalton; Francis Grove Practice, Wimbledon; Putneymead Practice Putney; Heathfield Practice Putney; and Cricket Green Practice, Mitcham and all the patients from these practices who participated.
Financial Support
The project was funded by the Health Technology Assessment (HTA) Programme of the NIHR (project number HTA 10/32/02) and will be published in full in HTA. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the HTA programme, NIHR, the National Health Service or the DoH. The funding body was not involved in the study design, collection of data, analysis and interpretation of data, writing of the manuscript or the decision to submit the manuscript for publication.
Conflicts of Interest
None.
Ethical Standards
Ethical approval for this study was granted by the London (Hampstead) Research Ethics Committee (12L/LO/0219). Trial registration: ISRCTN 98538934. St George’s University of London was the study sponsor.
Appendix 1
Example interview schedule for participants in the intervention groups and the control groups.
Intervention group
Main questions
-
1. Can you tell me about what physical activity you did last week? Was that a typical week for you?
-
2. Do you think taking part in the PACE-UP trial has changed the physical activity you are doing now?
-
3. Is there anything about the PACE-UP trial that you particularly remember? i.e. take home message
-
4. Do you still use the pedometer, diary or handbook given to you after the PACE-UP trial? If so, how often do you use them? If no, do you use anything else? i.e phone, fitbit.
-
5. What normally motivates you to be physically active? Is that different to how it was before you participated in PACE-UP?
-
6. Would you recommend the PACE-UP trial to family and friends?
-
7. Are there any additional resources or support that you could suggest that might help to keep you physically active? i.e family, friends, text messages, online resources, annual visit to nurse, walking groups ….
Closing
That was all the questions I had for you, is there anything else you would like to add or think I’ve missed?
Control group
Main questions
-
1. Can you tell me about what physical activity you did last week? Was that a typical week for you?
-
2. Do you think taking part in the PACE-UP trial has changed the physical activity you are doing now?
-
3. Is there anything about the PACE-UP trial that you particularly remember? i.e. take home message
-
4. What normally motivates you to be physically active? Is that different to how it was before you participated in PACE-UP?
-
5. As a participant in the study you may have received a pedometer, diary and handbook after the main trial was over. Did you find these resources helpful? Have you continued to use any of these resources? Do you use anything else? i.e phone, fitbit …
-
6. Would you recommend the PACE-UP trial to family and friends?
-
7. Are there any additional resources or support that you could suggest that might help to keep you ‘physically active?’ i.e. family, friends, text messages, online resources, annual visit to nurse, walking groups ….
Closing
That was all the questions I had for you, is there anything else you would like to add or think I’ve missed?
Prompt sheet
Pedometer use
-
∙ In what way do you think using a pedometer influences your physical activity?
Barriers to being physically active
-
∙ Are there any barriers or difficulties you’ve had to overcome when it comes to physical activity?
Motivation
-
∙ Do you set yourself any physical activity targets/goals? If yes, prompt more.
-
∙ Do you adopt any strategies to help you stay motivated to be physically active? If yes, prompt more.
Peer/social support and physical activity
Under question 5 if not discussed.
Appendix 2
Table A1 Themes and sub-themes with additional supporting quotes