The Democratic Republic of the Congo (DRC) is the largest country in sub-Saharan Africa with a population of over 84 million people (2018)(1). The macroeconomic and financial development of the DRC has been rapidly increasing since 2001. The gross domestic product (GDP) of the DRC increased from 7·4 billion dollars to 50·4 billion dollars in 2019(2), making the DRC one of the fastest-growing economies in the world(Reference Kuwonu3). Despite the significant economic growth and abundance of mineral and agricultural resources, large disparities between socio-economic statuses continue to exist in the DRC. According to data from the World Bank, 73 % of the Congolese population, or approximately 60 million people in 2018, lived on less than $1·90 a day, and one out of six people lived in extreme poverty(4). Over the past decade, the DRC has been affected by waves of civil wars and unceasing domestic conflicts. Violence, mass displacement and the destruction of infrastructure have devastated the health of the population(5,6) . As of 2008, an estimated 5·4 million deaths occurred as a result of the armed conflict between 1998 and 2007(Reference Hailegebriel7), mainly due to disease and starvation(8).
The DRC has among the highest percentages of chronic child malnutrition, or stunting, in the world with lasting consequences for the children who suffer from this nutritional disorder(Reference Watkins9). Malnutrition during early childhood is associated with adverse effects on cognitive and physical development(Reference Victora, Adair and Fall10,Reference Black, Victora and Walker11) and failure of proper development during the ‘critical age window of 1000 days’ can lead to cognitive and physical deficits in adulthood(Reference Roth and David Sweatt12,Reference Prentice, Ward and Goldberg13) . This can in turn result in poorer educational and economic outcomes(Reference Grantham-McGregor14–Reference Bleakley16). According to the 2018 Human Capital Index (HCI) which measures the survival of children using key health determinants, the DRC ranked 146 out of 157 countries(Reference Luo, Qu and Rockett17), indicating high mortality rates in children in the DRC.
Apart from the effects of malnutrition on stunting, studies have examined the association between factors such as socio-economic inequalities due to unequal distribution of power, wealth and resources with stunting in children(Reference Link and Phelan18–Reference Chirwa, Mantempa and Kinziunga21). Higher educational attainments of parents and place of residence were found to be positively related to the nutritional statuses of children(Reference Kanjilal, Mazumdar and Mukherjee19,Reference Kennedy, Nantel and Brouwer22–Reference Emina, Kandala and Inungu24) . However, there is a need for studies to further explore the risk of stunting at different levels of determination to identify key factors contributing to the progression of stunting in the DRC, especially at a national level. For this study, a conceptual framework for determinants of malnutrition was utilised to compare the importance of determinants (e.g. geographical and socio-economic indicators) at different levels and their impacts on household income and health service inequalities in the DRC(Reference Kandala, Madungu and Emina25). The findings of this study aim to provide decision-makers with comparative information on the impact of different factors affecting the nutritional statuses of children to provide empirical and evidence-based guidance to inform future interventions and policies(Reference Ruel and Alderman20,Reference Kaur26–Reference Rosenzweig and Wolpin29) .
Methods
Data
Data from the 2018 Multiple Indicator Cluster Survey (MICS-Palu) were utilised for this study. The MICS is a nationally representative household survey of children aged 0–5 years, women aged 15–49 years and men aged 15–59 years. This survey was conducted by the National Institute of Statistics and the Ministry of Planning of the DRC, in collaboration with the UNICEF and the United States Agency for International Development/Centres for Disease Control (USAID/CDC). The MICS generated more than 150 key indicators that provided disaggregated data on the situation of children and women, and the living situations of the population in the areas of health, nutrition, education, security, hygiene and sanitation.
Multi-stage stratified cluster sampling was employed for the selection of the survey sample. Both urban and rural areas across all twenty-six provinces in the DRC were included. Additionally, urban and rural areas were identified as the main sampling strata using a two-stage selection method. The urban and rural areas within each province were identified as the main sampling strata, and the sample of households was selected in two stages. Within each stratum, 721 clusters were selected systematically with probability proportional to size. After a household listing was carried out within the cluster, a systematic sample of thirty households was drawn in each cluster.
Variables
Height-for-age Z score (HAZ), weight-for-age Z score (WAZ) and weight-for-height Z score (WHZ) were analysed using the 2006 WHO child growth standards(30). A plausibility criterion of –6 to 6 sd from the median of the reference population has been used for WAZ and WHZ, and –7 to 7 sd from the median of the reference population for HAZ. We defined stunting as HAZ more than 2 sd below the median of the reference population, underweight as WAZ more than 2 sd below the median, wasting as WHZ more than 2 sd below the median and overweight as WHZ more than 2 sd above the median.
Four outcomes of maternal healthcare were selected for our study: delivery at a healthcare facility (public/private), antenatal care coverage (defined as four or more antenatal care visits), skilled attendants at birth and postnatal care (defined as a health check-up while in the facility or at home following delivery, or a postnatal care visit within 2 d after delivery).
Handwashing behaviours, clean water sources and improved toilet facilities were selected to analyse household sanitation. Correct handwashing behaviour was assessed using the availability of proper handwashing facilities, clean water and soap. Improved sources of drinking water were assessed with the use of the following types of water supply: piped water, tube well/borehole, protected dug well, protected spring, rainwater collection, and packaged or delivered water. Improved toilet facilities were assessed with the use of flush or pour flush to piped sewer systems, septic tanks, or pit latrines, ventilated improved pit latrines, pit latrines with slabs, and composting toilets.
Household economic status (measured using the wealth index) was utilised to measure health inequalities. Principal components analysis was performed to construct the wealth index by using the information on the ownership of consumer goods, dwelling characteristics and other characteristics that were related to household’s wealth, to generate weights (factor scores) for each of the items used(31). Highest educational attainment of mothers (no formal education or pre-school, primary school, secondary school, and tertiary and above), child’s weight at birth, age (in months), sex (male or female) and place of residence (rural or urban) were also taken into account.
Statistical analysis
Univariable and multivariable associations between the nutritional statuses of children and individual determinants such as the child’s age and sex, mother’s education level, maternal healthcare including the use of qualified birthing facilities, antenatal visits of more than four times, skilled attendants at birth, postnatal care checks, and household determinants including household wealth index and place of residence (urban v. rural) were analysed. The covariates were chosen based on previous literature on malnutrition in developing countries(Reference Novignon, Aboagye and Agyemang32,Reference Di Cesare, Bhatti and Soofi33) . The mixed-effects model with a random intercept specified at the primary sampling unit level was used to adjust for unmeasured factors that might affect the nutritional status of children. These features of the regression model also account for complex survey design. All the children included in the model were matched to their mother by ‘Cluster number, Household number and Mother’s line number’ provided by the original questionnaires for both adults and children.
Results
Descriptive characteristics
The characteristics of the participants are presented in Table 1. A total of 21 456 children under 5 years of age and 21 756 women of childbearing age in the DRC were analysed for this study. Among the 21 456 children under 5 years of age, the participants had a mean age of 2·44 years, a mean HAZ, WAZ and WHZ of –1·6, –1·05 and –0·15, respectively. The national prevalence rate of underweight, stunting and wasting was found to be 23·33 %, 42·05 %, and 6·54 %, respectively, whilst the prevalence rate of overweight was 3·80 %. The majority of children resided in rural areas (58·42 %). The majority of mothers had either no formal/pre-school education or primary school education (53·06 %). For the maternal healthcare coverage, the utility rate of antenatal visits over four times, delivery at health facilities, skilled attendants at birth and postnatal health checks were 43·21 %, 81·53 %, 85·20 %, and 56·59 %, respectively. In terms of domestic sanitation, the coverage of handwashing facilities, improved toilet and improved water were 56·73 %, 28·77 % and 54·66 %, respectively.
Table 1 Descriptive statistics for main variables in the analysis

Factors associated with children’s nutritional status – socio-economic inequalities
Figure 1 illustrated the distribution of wealth across all twenty-six provinces in the DRC. Households in the lowest wealth quintile are concentrated among the central provinces of the DRC and account for 46 %–60 % of households whereas, in western and southeastern provinces such as Kongo Central and Haut-Katanga, households in the lowest wealth quintile accounted for a smaller proportion (9 %–15 % of households). In Kinshasa, however, the proportion of households in the lowest wealth quintile was below 9 %.

Fig. 1 Distribution of the lowest wealth quintile households across the DRC. DRC, The Democratic Republic of the Congo
Nutrition status among children and maternal healthcare access differed across wealth quintiles. Higher household economic status was protective against children’s stunting (HAZ) and underweight (WAZ). However, such a protective effect was not found among wasting and overweight (WHZ) in Fig. 2. Therefore, children’s nutritional status was mainly assessed by WAZ and HAZ later in this study. Maternal healthcare, including the percentage of mothers with access to qualified birthing locations, antenatal care, skilled attendants at birth and postnatal care, was positively associated with the increasing household wealth (from the lowest to the highest wealth quintile) (Fig. 2).

Fig. 2 The children’s nutritional status and maternal healthcare indicators according to decile of wealth index
After matching, there were 20 202 mother–child dyads. Among them, 10 959 mothers had given birth within 2 years before the investigation and thus had information on maternal healthcare and were included in the regression analysis. Results from the crude random intercept linear regression estimating the association of the nutritional status of children with mother’s maternal healthcare and household socio-demographic factors indicate that among children, HAZ and WAZ were positively associated with maternal healthcare and domestic sanitation (Table 2). However, when employing a multivariable-adjusted regression, there was no statistically significant association between the nutritional status of children and maternal healthcare or domestic sanitation. The wealth index appeared to be positively associated with HAZ and WAZ. Likewise, mothers’ education level was also positively associated with HAZ and WAZ among children. Average WAZ was higher among children whose mothers had secondary level schooling, secondary school and above compared to those whose mothers had no formal schooling.
Table 2 Crude and adjusted associations of the nutritional status of children with maternal healthcare for the mother and household socio-demographic factors
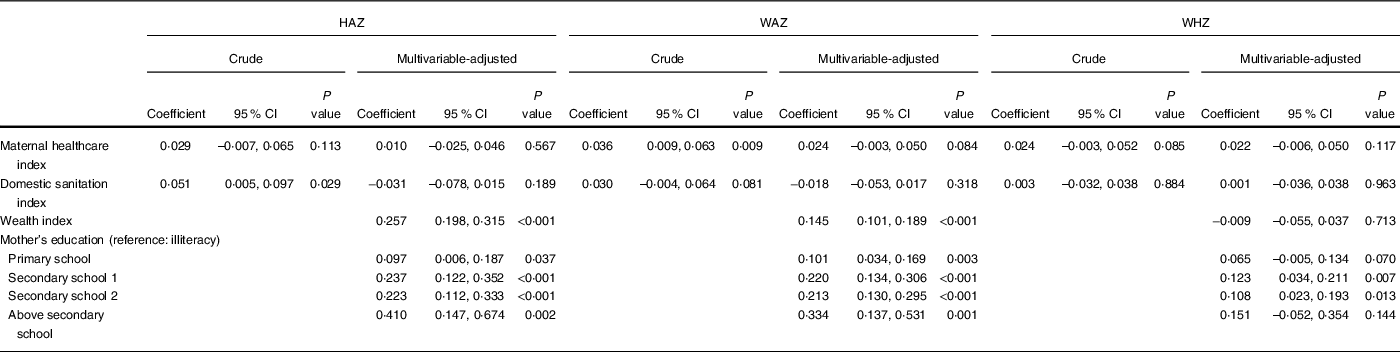
HAZ, height-for-age Z score; WAZ, weight-for-age Z score; WHZ, weight-for-height Z score.
Estimations from all models are adjusted for the place of residence (rural/urban), household size, child’s age (months) and sex, and mother's age (years).
Factors associated with children’s nutritional status and maternal healthcare access geographical inequalities
Figure 3 demonstrated province-specific net spatial effects of nutrition status among children, including the prevalence of underweight, stunting, wasting and overweight in the DRC. Darker colours correspond to higher prevalence, whereas lighter colours correspond to lower prevalence. Our mapping exhibited three key observations. Firstly, the prevalence of malnutrition among children was generally higher among central provinces in the DRC. Secondly, southwest provinces, including Kwango, Kwilu, Kasaï and Kasaï-Central, exhibited a higher prevalence of stunting and underweight among children. Thirdly, taking into account that eastern provinces are subjected to ongoing conflict, nutrition status was poorer among children in these regions.
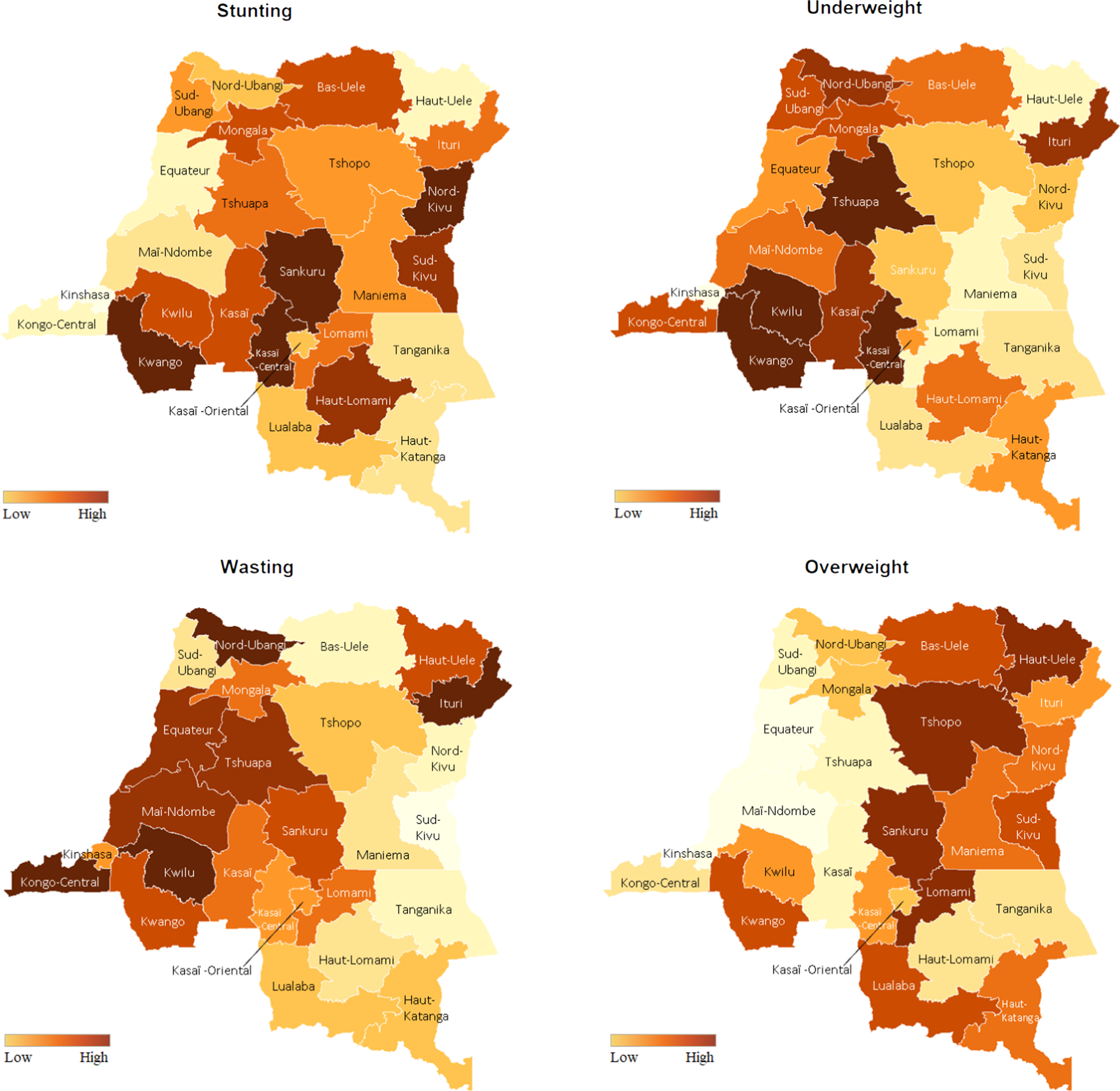
Fig. 3 The prevalence of underweight, stunting, wasting and distribution of economic status across the country
Maternal healthcare access coverage, including delivery at health facilities, antenatal care, skilled attendants at birth and postnatal care among women, is demonstrated in Fig. 4. Notably, western, eastern and southeastern provinces, such as Kongo Central, Kinshasa, and the Haut-Katanga, generally had good maternal healthcare conditions, in contrast to the lowest wealth quintile households being concentrated among the central provinces (Fig. 1). Additionally, it is worth noting that Kinshasa, the capital of the DRC, had both the best maternal healthcare and nutritional status among children in the country.
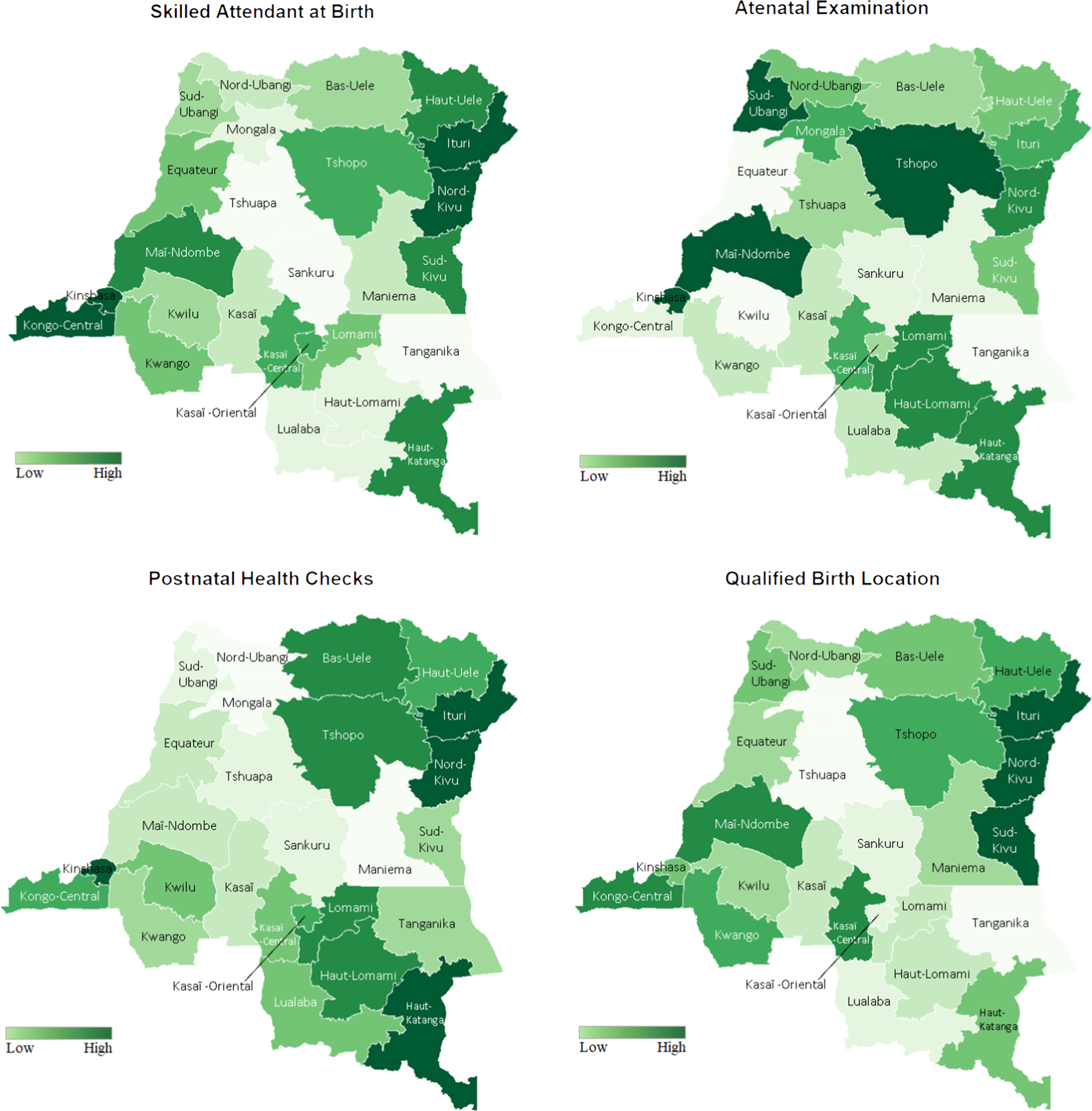
Fig. 4 The coverage of qualified birth delivery location, antenatal care (ANC), skilled attendants at birth and postnatal care (PNC) among women
Factors associated with children’s nutritional status (children’s height-for-age Z score and weight-for-age Z score) stratified by the lowest/highest wealth quintile in rural and urban settings
In the multivariable-adjusted analysis in Table 3, we stratified individuals from the lowest and highest wealth quintile and find that neither maternal healthcare index nor domestic sanitation index was associated with children’s HAZ and WAZ. Individuals falling within the lowest wealth quintile and living in rural areas had a lower HAZ (–0·585 (95 % CI –0·871, –0·300); P < 0·001) compared to those living in urban areas. Additionally, the mother’s education level was found to be a protective factor of children’s nutritional status. Average WAZ was higher among children whose mother had secondary school 2 (0·385 (95 % CI 0·161, 0·609); P = 0·001) and above secondary school (0·652 (95 % CI 0·222, 1·082); P = 0·003) education levels compared to children whose mothers had no schooling. Among the children falling within the highest wealth quintile, WAZ has a significant association with the wealth index only. On average, a one-score increase in wealth index was associated with a 0·347 increase in WAZ ((95 % CI 0·119, 0·576); P = 0·003). Furthermore, among those in the highest wealth quintile, there was no statistically significant association between the area of residence, mother’s education level and children’s nutritional status. Additionally, the result for the WHZ of children was also presented in the Appendix.
Table 3 Nutritional status of children from the households of the lowest and highest wealth quintile

HAZ, height-for-age Z score; WAZ, weight-for-age Z score.
Estimations are also adjusted for household size, child’s age (months), weight at birth (kg), child’s sex, and mother’s age (years).
Discussion
This study illustrates the DRC’s national profile of malnutrition among children between 2017 and 2018 using the nationally representative MICS survey. In comparison to the DRC’s MICS survey between 2010 and 2017(Reference Erwin34), the prevalence of stunting decreased from 43 % to 42 %, the prevalence of underweight decreased from 29 % to 23 % and the prevalence of wasting decreased from 7 % to 6·5 %, respectively. This trend is comparable to findings from the DRC’s 2013 Demographic Health Survey (DHS)(Reference Erwin34), where the prevalence of stunting, underweight and wasting were 43 %, 22·6 % and 7·9 %, respectively. In addition, a recent study that assessed malnutrition among children in forty-seven low-income and middle-income countries using 4–6 rounds of MICS(Reference Emerson, Savage and Llewellyn35) between 2010 and 2017 found that the overall average rate of stunting, underweight and wasting was 32·5 %, 18·7 %, and 4·6 %, respectively. These rates are much lower than that of the DRC. Hence, malnutrition remains a significant health burden in the DRC.
This study also found a relationship between malnutrition, maternal healthcare coverage and the geographic distribution of provinces in the DRC. Central provinces in the DRC generally had a higher prevalence of malnutrition among children as well as lower coverage of maternal healthcare. This can be attributed to relatively unprosperous economies in these provinces (Fig. 1). Although these provinces have agricultural potential, due to the vast deposits of diamonds, people tend to rely on the artisanal mining industry for a living, instead of involving in agriculture(Reference Rodriguez-Alvarez, Lanborena and Borrell36). The deterioration of the transportation network also poses negative impacts on food security(Reference Weijs, Hilhorst and Ferf37). Provinces in this region are landlocked with irregular train service in bad condition, which is difficult to reach. Furthermore, the violence that erupted in Kasaï during the August 2016 hindered the transportation of essential supplies, which negatively impacted the economy, causing price hikes on items such as food. As a consequence, hundreds of thousands of malnourished children were at increased risk of starvation(Reference Rodriguez-Alvarez, Lanborena and Borrell36).
Over the years, the DRC’s Katanga region has been faced with chronic instability. However, children’s nutrition status and the coverage of maternal healthcare are relatively better in comparison to central provinces, which could be attributed to several factors. Firstly, the Katanga region is one of the three main economic hubs in the DRC with large commercial and industrial bases, highly developed mining industries, and agricultural sectors(38). Secondly, vast investments and international health assistance have been concentrated in this region. For example, as of 2018, Doctors Without Borders run comprehensive medical programmes including maternal and paediatric health care in these provinces(Reference Fox, Himawan and France39). As a result, people residing in these regions are more likely to have access to healthcare resources as well as the motivation to utilise these services.
Our study further confirms the relationship between malnutrition and socio-economic inequalities. Results of the descriptive analysis show that as households’ wealth index scores increased, the prevalence of malnutrition decreases, while the coverage rate for maternal healthcare services increases. As Muennig and Su pointed out, money plays an important role in the health of individuals, especially in very poor countries where food is a critical element of survival and requires financial capabilities(Reference Muennig and Su40). The random intercept linear regression model in our study (Table 2) confirms that the household’s wealth significantly improves the nutrition status of the children. The relationship between poverty and malnutrition has also been elaborated by Müller and Krawinkel, such that poverty leads to insufficient household food security, insufficient child and maternal care, and unhealthy environments(Reference Müller and Krawinkel41), which in turn cause malnutrition.
Historically, many studies in developing countries (such as Ethiopia, Indonesia and Bangladesh) have proved that community factors, such as domestic sanitation and healthcare service, are closely related to variations in children’s nutritional status(Reference Wirth, Rohner and Petry42–Reference Islam, Zafar Ullah and Mainali44). Insufficient health services and an unhealthy environment are also important contextual factors that may contribute to worsening rates of malnutrition in the UNICEF framework of causes of malnutrition (UNICEF 1990)(45). As demonstrated by the UNICEF framework, malnutrition is determined by a range of factors relying on the implementation of interventions by a multitude of sectors. Previous researches showed a strong relationship between the nutritional status of children and its immediate and underlying determinants. For example, in Gabon, feeding practices and access to improved water and sanitation were the best predictors of stunting(Reference Blaney, Beaudry and Latham46). In both Bangladesh and Vietnam, household food security, better caregiver nutrition knowledge and hygiene practices were positively associated with stunting(Reference Nguyen, Headey and Frongillo47). However, results in Congo show that underlying causes such as domestic sanitation and maternal healthcare have little impact on children’s malnutrition while taking basic causes, namely economic structure into account. Using the principal component factor method, we identify the maternal healthcare index as a proxy for healthcare accessibility among households. To our surprise, the maternal healthcare index had no statistically significant association with children’s nutrition status after including household wealth score and mother’s education level. One potential explanation for this finding is that the child nutrition programme may have not been well integrated with maternal healthcare programmes in the DRC, as a result of a fragmented health system that is observed across and within disease control programmes. According to the country report from WHO, between 2006 and 2012, altogether 195 projects and programmes in the health sector of the DRC had external funding but lacked functional coordination among the different health programmes, even when housed in the same building(48). In conclusion, even though maternal healthcare is accessible to households, it may not ensure the availability of child healthcare. Another possible explanation on why the maternal healthcare index has no impact on children’s nutrition status may be attributed to quality issues present in the healthcare delivery system. Since the 1990s, governmental funding for the public health sector has declined in the DRC, and health financing is highly accounted for by out-of-pocket payments (39 % in 2016(8)) and external aid (42·5 % in 2017(8)). With little public funding and weak national leadership, health sector regulation in the DRC has digressed. Additionally, in 2017, the infant mortality in the DRC was 43 per 1000 live births, the child mortality was 70 per 1000 births(Reference Gill, Jones and Hammett49) and the maternal mortality ratio was estimated at 693 per 100 000 live births in 2015(Reference Li, Liu and Sun50). Although healthcare accessibility exists, poor-quality healthcare at delivery may prohibit children from fully benefiting from these services.
To further assess the factors associated with children’s nutrition status among vulnerable populations, we extracted 20 % of the poorest households and 20 % of the richest households from the overall population. We followed this by employing a multivariate regression where we found that residing in urban areas and children whose mothers had secondary schooling and higher were protective factors for children among the poorest households after controlling for wealth score. Also, urbanisation has both a direct and an inverse association with child mortality among sub-Saharan African countries, and the DRC, in particular, has experienced the highest reduction in child mortality as a result of urbanisation(Reference Anyamele51). This finding is consistent with the reduction in child malnutrition in our study. The benefits of residing in urban areas include the availability of various food products, better infrastructure and more accessible healthcare resources due to the concentration of health workers(48). Besides, the mother’s education has shown to be an independent protective factor for the nutrition status of the children living in the poorest households. Moreover, previous literature emphasised the importance of a mother’s education on children’s health and nutrition(Reference Makoka52,Reference Fadare, Amare and Mavrotas53) . The various pathways through which a mother’s education promotes a child’s nutrition status include the acquisition of health knowledge, adherence to recommended feeding practices for children and increased command over resources.
There are some limitations to this study. Firstly, although we found significant associations between child malnutrition with geographical and socio-economic inequalities in this study, causal inference cannot be drawn as this was a cross-sectional study. Secondly, healthcare access is surrogated by maternal healthcare coverage in this study. This was due to the lack of available data to measure a household’s access to healthcare, such as distance to the closest clinic and affordability of medical visits. The study also assumed a linear additive relationship between the explanatory and dependent variables. The possibility of a non-linear relationship was not explored in our study. Finally, the household’s wealth status was measured based on asset endowments only.
Conclusion
This study revealed considerable socio-economic inequalities in nutritional status among children in the DRC and the prevalence of malnutrition is higher in underdeveloped regions.
It calls for an urgent need for nutrition promotion in integrated services of maternal and child healthcare. Policy implementation of better healthcare should particularly prioritise central provinces and improve nutrition education for less-educated mothers.
Acknowledgements
Acknowledgements: None. Financial support: This work was supported by the National Natural Science Foundation of China (grant number 72074130) and the Spring Breeze Foundation of Tsinghua University (grant number 20203080035). Kun Tang received these two grants. Conflict of interest: There are no conflicts of interest. Authorship: K.T., X.Q. and Y.F. contributed to the study concept and design, results interpretation, drafting, and revision of the manuscript and approved the final version of the manuscript. X.Q., Y.F. and Q.H. did the statistical analysis. X.Q. and Y.W. contributed to the introduction drafting and results interpretation. W.C. contributed to the statistical analysis and results interpretation. X.Q., Q.H., J.H. and R.T. contributed to the revision of the manuscript. K.T. is the guarantor of this work and, as such, had full access to all the data used in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. X.Q. and Y.F. contributed to the study equally, listed as co-first authors. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving research study participants were approved by the Ministry of Plan of the DRC. Written informed consent was obtained from all subjects/patients. The data used in the study consisted of a publicly available de-identified dataset, which was retrieved from the UNICEF MICS website with permission.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980021004249









