Introduction
It is generally accepted that the relationship between a therapist and a client is important in the delivery of psychological treatments for achieving favourable client outcomes (Horvath & Simmons, Reference Horvath and Simmons1991; Martin et al. Reference Martin, Garske and Davis2000; Zuroff & Blatt, Reference Zuroff and Blatt2006). Various aspects of the therapeutic relationship have been identified as important in addition to characteristics of both the therapist and the client. Typically, this work is descriptive with little theoretical contribution to suggest why specific aspects of the relationship are important. Furthermore, while the relationship has traditionally been considered to be largely determined by the therapist with the client fulfilling the role of responder (Keijsers et al. Reference Keijsers, Schaap and Hoogduin2000), that conceptualization has changed in recent years, with recognition of the role of the client as an active agent in the formation and development of the relationship (Bohart & Tallman, Reference Bohart and Tallman1996; Stiles, Reference Stiles2009). This refocus of the literature guides our approach which places clients’ willingness to freely peruse their problems at the heart of change. To do so, we utilize a theoretical framework to understand the contribution of both the therapist and the client, to clarify the important elements of the therapeutic relationship, and to inform the resolution of problems in the relationship when they occur. A theoretical framework that accomplished this would enable therapists to provide treatment efficiently and effectively for the benefit of the clients.
Our intention in this paper is to provide one possible framework for practitioners within which the therapeutic relationship can be understood and utilized for good therapeutic effect. A comprehensive review of the therapeutic relationship literature, therefore, is beyond the scope of this paper. We do, however, describe the relevant literature that contextualizes our proposal. Excellent reviews of the therapeutic relationship in cognitive-behaviour therapy (CBT) are already available (e.g. Waddington, Reference Waddington2002) as well as reviews of specific functions of the relationship such as collaborative empiricism (e.g. Tee & Kazantis, Reference Tee and Kazantis2011). After defining key terms and contextualizing our proposal within the existing literature, we lead to a conceptualization of the therapeutic relationship based on Perceptual Control Theory (PCT; Powers et al. Reference Powers, Clark and McFarland1960; Powers, Reference Powers1973). PCT proposes that all actions are goal-serving attempts to control one's own experiences. This leads us to a dynamic model that illustrates how matches and mismatches in client and therapist goals can impact on the therapeutic relationship. We conclude with key recommendations for practising therapy based on this model.
Definitions and clarifications
In this paper, when we refer to a ‘therapeutic relationship’ we are referring to the situation where someone designated a ‘client’ arranges to meet with someone designated a ‘therapist’ for the purpose of resolving some psychological distress the client is experiencing. The resolution of psychological distress is an internal experience which we have conceptualized diagrammatically in Figure 1.

Fig. 1. Conceptual diagram of the internal process facilitated during effective psychotherapy. Any activity that facilitates or promotes this internal process could be considered to be therapeutic.
We consider that activities, people, and events that promote the change process from psychological distress to psychological contentment (see Fig. 1) will be experienced as therapeutic by the client. By ‘therapeutic’, we mean facilitation of a reduction in the experience of psychological distress. We suggest that this reduction can be achieved through the client's candid and persistent exploration of their problem and the problem's impact on important areas of their life.
Clearly, the therapeutic relationship is not the only way a therapeutic effect can be achieved. Computer self-help programs can be therapeutic (i.e. assist in the reduction of psychological distress) and so can activities such as behavioural experiments, activity schedules, and thought diaries. Thus, we are not suggesting that the therapeutic relationship is necessary to achieve the therapeutic effect depicted in Figure 1. We do suggest, however, that the therapeutic relationship may be sufficient to achieve that effect. It is the instance of explicitly using the client–therapist relationship to achieve a therapeutic effect that is our interest in this paper. While we appreciate, therefore, that there are many things that can be therapeutic for a client (behavioural experiments, exercise, thought diaries, etc.), we hypothesize that therapy can be provided effectively and efficiently by using the therapeutic relationship as the main therapeutic instrument.
Contextualizing our hypothesis: goal- and expectation-based models of the therapeutic relationship
In a key article, Leahy (Reference Leahy2008) highlights the importance of the therapeutic relationship in the delivery of CBT and outlines how elements of CBT such as case conceptualization may be useful for promoting a productive relationship. Leahy suggests that problems can occur in the relationship if clients have particular types of beliefs and also when there is a mismatch, or an ‘over-match’, between therapist and client schemas. The idea of a mismatch between client and therapist expectations has also been suggested by Keijsers et al. (Reference Keijsers, Schaap and Hoogduin2000). They propose that problems will occur when the therapist's behaviour deviates too much from what is expected by the client. Similarly, Reis & Brown (Reference Reis and Brown1999) reviewed the literature with regard to the characteristics of clients who ‘drop out’ of therapy and found that the degree of convergence between therapist and client perspectives was an important factor in whether or not a client continued with treatment.
Stiles (Reference Stiles2009, p. 88) extends the idea of expectations and deviations by suggesting that ‘both therapists and clients are trying to be helpful’ within the relationship.
They monitor expected outcome, and when they see deviations they act to make corrections [cf. Powers, Reference Powers2005]. They watch what happens and use what they notice. If they discover a productive approach, they tend to continue it. If they try something that doesn't work, they tend to stop doing it or modify it.
One of the areas in which this constant adjusting can occur is in the way clients discuss their problems. Keijsers et al. (Reference Keijsers, Schaap and Hoogduin2000), for example, suggest that therapists might use more closed questions if clients hesitate over answering open questions. Similarly, clients who are reluctant to talk about their problem may give very brief answers to exploratory types of questions. A large part of treatment, therefore, might involve a subtle kind of unspoken negotiation as therapists continually adjust their verbal and non-verbal behaviour to promote or increase clients’ discussions of their problems. Keijsers et al. (Reference Keijsers, Schaap and Hoogduin2000) report results from a review of the literature which suggests that it is not the amount of time spent speaking about a problem but the way the problem is discussed which is important in terms of outcomes. Reis & Brown (Reference Reis and Brown1999) report research that suggests that therapists who were ‘high engaging’ with regard to clients returning for more sessions tended to spend time elaborating on what the client had said rather than contradicting it or invalidating it.
In psychiatry, the importance of good communication within the context of a therapeutic relationship is also acknowledged. In particular, problems can arise when clients and therapists try to control the conversation in different ways (McCabe & Priebe, Reference McCabe and Priebe2008). McCabe & Priebe report the results of a study which suggested that clients frequently wanted to discuss their hallucinations and delusions but the psychiatrist therapists were reluctant to do so and frequently avoided these concerns. This avoidance often led to confrontation and disagreement with the possibility of the client disengaging from treatment, providing another example, therefore, of the importance of the congruence between therapist and client expectations.
Perceptual Control Theory
While there are many theories about concepts such as goals, expectations, and self-regulation, very few theories are expressed in functional terms in the sense of how an expectation actually works to influence behaviour. PCT (Powers, Reference Powers1973, Reference Powers2005) is one such theory. Interestingly, it is based on a ‘control systems’ approach that is also utilized in both attachment theory (Bowlby, Reference Bowlby1969) and contemporary CBT (Mansell, Reference Mansell2005; Watkins, Reference Watkins2011). PCT provides the foundation for our proposal as it offers an explanation of how the therapeutic relationship might facilitate therapeutic outcomes. PCT describes the way in which behaviour is constantly adjusted through negative feedback to keep perceived deviations from an internal benchmark (reference, belief, goal, expectation, etc.) at a minimum.
Based on PCT principles, an interaction between two people can be conceptualized as the linking of two control systems through a shared environment (see Fig. 2). Both people in the interaction have their own goals about the interaction (and about many other things as well) and make constant alterations to their behaviour so that what they perceive (see, hear, feel) remains close to what they want to experience (internal reference or goal). When treatment proceeds satisfactorily both the therapist and the client are able to keep any deviation they sense to a minimum.

Fig. 2. Generic model of the interaction of two people conceptualized as control systems. * Sensors can be thought of things such as eyes, ears, and skin in which environmental input is converted into neuronal signals. † Muscles and glands are those parts of the system that allow individuals to affect their environments.
To illustrate this process, suppose that a therapist has a goal of understanding the situations in which a client's panic attacks occur. The therapist will ask questions about when, where, how often, for how long, and so on, until they have the amount of information they think is necessary. Perhaps the client has a goal of helping the therapist understand what they are going through so they answer questions and provide details about their panic experiences. This interaction is summarized diagrammatically in Figure 3.

Fig. 3. Model of a therapist seeking to understand a client's panic attacks, and a client wanting to help the therapist understand the attacks.
From time to time, as the client describes their experiences, they might be reminded of various incidents and may even begin to explain these to the therapist. For example, the client might remember how happy they were when they graduated from university. If they start to tell the therapist about this, however, the therapist (who is sticking to their goal of finding out about the panic attacks) will begin to sense that the topic is getting ‘off track’ (a deviation) and will ask more questions about the current panic attacks.
Similarly, there may be times when the therapist spends too much time on one area (from the client's perspective). Perhaps the therapist takes some time at the beginning to ask the client about how their week has been but the client might just want to get straight into the problem [this could be considered to be a divergence of perspectives from Reis & Brown's (Reference Reis and Brown1999) point of view]. The client might give short, brief answers and start talking about their panic attacks in order to reduce the difference between what they are talking about and what they want to talk about. Throughout this conversation there may well be subtle adjustments by both the therapist and the client to keep the conversation happening the way each of them prefers.
McCabe & Priebe (Reference McCabe and Priebe2008), use an example with a potentially different outcome. They describe a situation where ‘One patient asked “Why don't people believe me when I say I'm God?” to which the doctor, after initial avoidance, replied “What should I say now?” ’ (p. 404). In this instance the patient could be considered to be attempting to reduce a discrepancy – perhaps they have attended the session to understand more about their situation. They currently do not understand what is happening and they would like a better understanding (see Fig. 4). When they ask this question, however, it appears to create a deviation for the doctor. Perhaps the doctor has a goal of discussing the patient's medication and also the social engagement activities the patient has enjoyed this week. When the patient asks a question related to their symptoms this creates a mismatch for the doctor between what is expected and what is happening. Initial avoidance occurs and then a request for assistance from the patient.
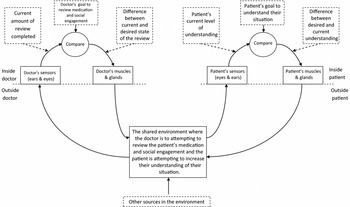
Fig. 4. Model based on an example by McCabe & Priebe (Reference McCabe and Priebe2008) of a doctor seeking to review a patient's medication as well as their level of social engagement for the past week while the patient is seeking to understand some aspect of their interactions with other people.
This example highlights the simplicity of Figure 2. Actually, both the doctor and the patient will have many goals that are important to them when they are interacting. According to PCT, these goals are arranged in parallel and hierarchically in a network of negative feedback control systems. Elsewhere we have discussed the role of multiple goals in the manifestation of psychological distress (e.g. Carey, Reference Carey2008a, b; Mansell, Reference Mansell2005). For this example, however, it can be appreciated that the doctor, as well as the patient, may be experiencing conflicting goals. The doctor might have a goal about discussing particular topics but may also have a goal about keeping the patient engaged. Now, in response to the patient's question, if the doctor does things to keep that patient engaged (by answering their question) that will increase the deviation for the doctor's other goal about what should be discussed in the session (from the doctor's perspective). If the doctor decreases the deviation about what should be discussed by staying on the topics of medication and social engagement, this will increase the deviation away from the doctor's goals about keeping the patient engaged in the session. The doctor's conflict in this situation can be understood as having an important overarching goal and two incompatible goals related to achieving the overarching goal (see Fig. 5). These goals might not always be incompatible but in this context they are.
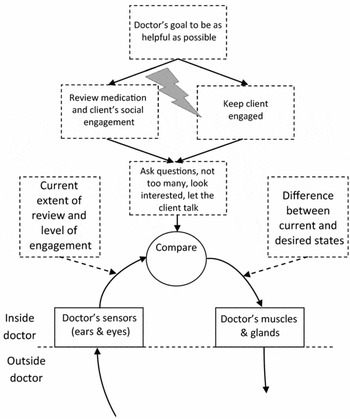
Fig. 5. Possible internal conflict between incompatible goals of the doctor in the example by McCabe & Priebe (Reference McCabe and Priebe2008) resulting in indecision and uncertainty.
The literature provides some clues for therapists about important goals to adopt when providing treatment. Although it seems to be rarely stated explicitly, it does not seem contentious to suggest that a prerequisite for therapy to commence is that the client must consider, talk about, or otherwise express their problem, or at least a problem that is relevant to therapy. So the therapist needs to establish an environment that is conducive to this.
Prior to coming for treatment, however, it is likely that the client has thought about their problem and talked about it with people other than the therapist. Therefore, it is not talking about their problem per se that is important (because they may already have been doing this), but talking in a focused and specific way about the problem. A range of evidence suggests that the manner in which the client thinks about their problem normally can be problematic. For example, ruminative thinking (Watkins, Reference Watkins2011) and avoidance of experiencing emotion (Hayes et al. Reference Hayes, Wilson, Strosahl, Gifford and Folette1996) are associated with the maintenance of distress because they result in avoidance of talking about the problem, but helping clients focus on emotional experience (Johnson, Reference Johnson2002), deeper meanings such as ‘core beliefs’ (Dudley et al. Reference Dudley, Kuyken and Padesky2010), and directly addressing their problems (Nezu & Perri, Reference Nezu and Perri1989) is associated with the long-term relief of distress. We suggest that, mostly in therapy, the way in which this relief is facilitated is through talking to the client in various ways (questioning, reflecting, etc.).
While this kind of directive, focused conversation is an element of many different therapies, it has been distilled as the main element in a transdiagnostic cognitive therapy called the Method of Levels (MOL; Carey, Reference Carey2006) for which there is accumulating evidence collected in naturalistic studies conducted across different time periods, contexts, and therapists (e.g. Carey et al. Reference Carey, Carey, Mullan, Spratt and Spratt2009). It is beyond the scope of this paper to describe MOL in detail; however, it is a focused problem-solving cognitive therapy in which the only activity is to facilitate the client's in-depth exploration of their incongruent attitudes and beliefs in order to find higher-order, more important values and ideals through which this incongruence can be reconciled.
MOL is based on the principles of PCT and maintains that by using questioning to encourage the client to review their problem in detail the client will become aware of aspects of their problem they had previously not attended to. In particular, the therapist is involved in a type of guided discovery to help the client focus on their present moment thoughts and feelings and how they may be related to longer term goals, beliefs, and values. For this process to be effective the client needs to be willing to peruse and express whatever comes into their mind so that they can listen to the idea from outside their head rather than from just inside it. We hypothesize that it is this feature of the therapeutic relationship (providing an opportunity for unrestrained examination by the client) that sets the therapeutic relationship apart from other relationships in the client's life and makes the therapeutic relationship therapeutic.
The therapeutic function of the therapeutic relationship, therefore, arises when an opportunity is created for the client to scrutinize problematic material in a focused, sustained, and uncensored way.
In day-to-day social interactions, people generally filter what they say and phrase things in particular ways in order to achieve certain effects (or goals) during the conversation. For example, they might not want to offend their friend or worry their partner or appear incompetent at work so they portray things accordingly. This process is exaggerated in anxious individuals and has counterproductive effects (Meleshko & Alden, Reference Meleshko and Alden1993). However, in an ideal therapeutic relationship, clients will say whatever comes into their mind and reflect on it after it has been expressed rather than before. In this way clients are able to spend time examining ideas, thoughts, and images that might have otherwise only been in their awareness fleetingly, peripherally, or that which they might not have attended to whatsoever. They might have been thoughts the client was trying to block out and not think about at all. The hierarchical organization of goals can be used to advantage here to help clients become aware of higher-level goals that might be influencing their current state. A simple, brief example of hierarchical goals is illustrated in Figure 5 for the doctor. PCT asserts that the goals of all people are organized hierarchically. A goal to arrive at work on time helps achieve the more essential goal of performing well at work which helps achieve the higher level goal of building a successful career which then helps achieve the goal above that of living the life one wants to live. This hierarchical arrangement is exploited in MOL by directing a client's attention to the higher order but out of focus areas of their life related to the problem that they are currently aware of.
For example, as clients talk about their problems they might say something like ‘That sounds stupid’ or ‘I don't know why I reacted like that’. These statements could be thought of as ‘meta-statements’ in that they are evaluations of what has just been expressed. A therapist with an understanding of PCT would assume that this statement indicates that the client's awareness may have just moved to a more important, more highly valued goal and so, further questioning would be used to direct the client's attention to any background thoughts occurring about this higher level goal. The therapeutic relationship will therefore be therapeutic, when it facilitates a client's detailed exploration of their problem so that attention can be directed to background thoughts that enable awareness of other important goals, thus developing mental flexibility.
The hierarchical arrangement of goals can help therapists prioritize their tasks during treatment delivery. While the establishment of warmth and trust, for example, are important goals, they should be considered a means to an end and not the end in themselves. For example, if one asked ‘Why should warmth and trust be established?’ one could answer with ‘So the client will feel safe to examine all facets of their problem’. Warmth and trust, therefore, are being used to create an environment where the client can freely explore their problem. The reverse, however, does not apply. If one asked ‘Why should I encourage the client to explore freely?’ the answer might be something like ‘So they can become aware of aspects of their problem they previously hadn't considered in much detail and by doing this can find solutions for themselves through cognitive reorganization’. The answer would not be ‘So that warmth and trust will be generated.’ On the other hand, if one asked ‘How can my clients be encouraged to freely examine their problems?’ the answer might be something like ‘By establishing warmth and trust.’ In PCT it is accepted that ‘Why?’ questions tend to move a person's attention up the hierarchy of control systems whereas ‘How?’ questions tend to move attention to lower levels. Encouraging people to investigate their internal experiences, therefore, is one of the most important goals of therapy. ‘Why?’ and ‘How?’ questions can be very useful for therapists as well as clients. Therapists could ask themselves ‘Why?’ about the various strategies they use in order to identify the goals they are seeking to realize in treatment. Moreover, once they have identified important goals they could ask ‘How?’ questions to discover different ways of achieving those goals.
In line with this approach, there is emerging evidence to suggest that the extent to which the client feels ready and able to explore their problem and answer the therapist's questions predicts symptom improvement following a therapy session, over and above the client's perception of the therapeutic alliance. However, both a rating of therapist adherence to the therapy and the client's rating of the working alliance at the end of one session predicted their readiness to talk about their problems at the beginning of the next session (Kelly, Reference Kelly2011). These findings both support the notion of the client's openness and ability to talk freely being important, for therapy, and suggest that a focused form of questioning as part of a structured therapy and the therapeutic relationship facilitate this readiness.
This model can be applied when there appears to be ruptures in therapy. For example, during the conversation, the therapist might get the idea that the client is thinking about what they are going to say next or searching for the right answer (perhaps they have goals about presenting themselves in a particular way to the therapist). This can be addressed quickly and directly by asking questions like ‘Are you thinking of the right way to say what you want to say?’ or ‘Are you wondering what I'm thinking just now?’ Thus, without explicitly focusing on the client's communication, their free expression can be promoted by the questions that are asked. Such questions should focus on experiences in the present moment, increasing the likelihood of clients being able to access the perceptions that are currently occurring in therapy. Reis & Brown (Reference Reis and Brown1999) highlight the importance of ‘preparing’ clients for therapy by the therapist and the client becoming clearer of each other's expectations and, therefore, achieving more convergent perspectives. In the context of this article, treatment preparation could involve the therapist explaining to the client the importance of talking freely and the kind of questions they might ask to help facilitate the client directing their attention to background thoughts.
One client put it succinctly:
Even though I know that words are never sufficient, the effort I put into putting my experiences into words seems to make them clearer, and then they make sense. I could only risk doing that in these sessions at the start, but now it's easier to put my feelings into words, and it makes them all seem so much more . . . normal!
Returning to the start: what is a warm, empathic, and compassionate stance?
We propose that therapists who set and monitor goals for themselves about promoting the client's candid expression, who understand the client's psychological distress as arising from conflicted goals, and who formulate problems within the therapeutic relationship as mismatches between their goals and those of the client, will embody many of the qualities that are known to be involved in a good therapeutic relationship, as described at the start of the article. Therapists will be very careful not to engage in recommendations, advice, and questioning that would impose their own goals upon the client (also known as arbitrary control: Powers, Reference Powers1973; Higginson et al. Reference Higginson, Mansell and Wood2011). These therapists will be attuned to indications of any conflict between their goals and those of the client, such as subtle changes in affect or behaviour. They will be curious about what the client's own goals could be and look to see how their expertise can facilitate those goals. Thus, we propose that by purposefully monitoring goals and their mismatch in the present moment of therapy, a therapist is being non-judgemental, warm, and empathic (Higginson et al. Reference Higginson, Mansell and Wood2011).
It is possible that this not only has the effect of helping the client to talk about their problems candidly in the session but also to later think about their problems more freely and flexibly in their own heads. Part of this process also includes the integration of conflicting cognitions and inconsistencies in personal goals. In early approaches, this process has been termed the development of an ‘internal working model’ (Bowlby, Reference Bowlby1969), or the adoption of a compassionate ‘social mentality’ (Gilbert, Reference Gilbert2005). Our approach echoes the importance of this internal process, and attempts to explain the mechanism through which it develops as an emergent effect of the therapist enabling the free expression of experience in therapy. Although beyond the scope of the current paper, we propose that the imagination mode within PCT (Powers, Reference Powers1973) would be involved. This mode enables an individual to replay memories of past perceptual experience as though they are happening in the moment, and thus could explain how a client could reinstate the helpful stance that their therapist took in therapy, even when outside the therapy.
Conclusion
Our hypothesis in this paper is that a therapeutic relationship will be therapeutic in and of itself when it facilitates the client's uninhibited exploration of their own internal world. This refining of the important element of the therapeutic relationship could give therapists a useful area on which to focus when therapy is not proceeding as they would like. When there seem to be difficulties in therapy, targeting explicitly the extent to which clients feel able to unreservedly explore their distress may provide a tangible way of resolving problems to promote enhanced outcomes for clients.
Summary
• The most therapeutic aspect of the therapeutic relationship is the establishment of an environment that promotes the unfiltered exploration of a client's internal experiences.
• This type of unadulterated yet focused and directed form of reflection allows the client to develop a greater awareness of different aspects of their problem and to generate their own solutions to their difficulties.
• Problems in the therapeutic relationship can be understood through a framework of misaligned goals.
• Seeking to understand the goals of the client in attending treatment sessions can help therapy to proceed more smoothly.
• The goals of the therapist can be considered hierarchically with the higher order goal being to adopt an invitational, curious attitude that encourages clients to freely investigate and report on their current state of mind.
• Discussing the interactional process occurring between the therapist and the client can sometimes assist in progressing treatment.
Declaration of Interest
None.
Learning objectives
After reading this paper people will be able to:
(1) Focus on maximizing a key element of the therapeutic relationship.
(2) Formulate problems in the therapeutic relationship in terms of misaligned goals.
(3) Enhance client outcomes through a more specific understanding of the important element of the therapeutic relationship.







Comments
No Comments have been published for this article.