To the Editor—Doctors, nurses, and other medical staff are greatly concerned about nosocomial outbreaks of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Environmental contamination is a possible source of nosocomial transmission.Reference Wang, Hu and Hu1,Reference van Doremalen, Bushmaker and Morris2 However, how effective environmental cleaning is against SARS-CoV-2 remains unclear.
A 75-year-old man infected with SARS-CoV-2 was diagnosed with COVID-19 during the quarantine period on the Diamond Princess cruise ship. He was transferred directly to our hospital on February 11, 2020. He resided in patient room A for 2 days then was moved to room B, where he stayed for 19 days. After cleaning the rooms thoroughly with disinfectant (Rely+On Virkon, LANXESS, or RUBYSTA in Japan), we tested 15 areas that were in close contact with the patient and medical staff. Swabs were used to transfer 5 environmental samples from room A and 10 samples from room B to universal transport media (Copan, Murrieta, CA). Cleaning was conducted immediately after the patient left the rooms. Environmental sampling was conducted within 5 days and 30 min after the patient left rooms A and B, respectively. Nucleic acids were extracted using MagMAX Viral/Pathogen Nucleic Acid Isolation Kit (ThermoFisher Scientific, Waltham, MA) and were tested using real-time reverse transcription polymerase chain reaction (RT-PCR) targeting the nucleocapsid (N) gene of SARS-CoV-2. Seven sets of primers and probes (CDC-N1, CDC-N2, CDC-N3, YCH-N1, YCH-N2, NIID-N1, and NIID-N2) were used to detect SARS-CoV-2 as previously described (Supplemental Table 1 online).Reference Hirotsu, Mochizuki and Omata3 For the internal positive control, the human ribonuclease P 30 subunit (RPP30) gene was used. The patient’s records, timing of cleaning and sampling, and RT-PCR results were collated.
On admission, the patient had fever (39°C) and a mild cough (Supplemental Table 2 online). The chest X-ray and computed tomography scan on day 1 showed signs of pneumonia in both lungs. He received lopinavir/ritonavir and antibacterial therapy on day 2, but showed respiratory failure. He received supplemental oxygen from day 4 to day 15. After careful clinical management, the patient’s overall status improved. RT-PCR showed that his sputum was positive for SARS-CoV-2 on day 11. Subsequently, nasopharyngeal swabs were negative on days 17, 22, and 29.
The patient stayed in room A for 3 days, during which he had the SARS-CoV-2 infection. After cleaning room A, 5 environmental samples were examined by RT-PCR. All samples were negative for SARS-CoV-2 and were positive or negative for RPP30 (Table 1).
Table 1. Real-Time RT-PCR Analysis of Environmental Samples
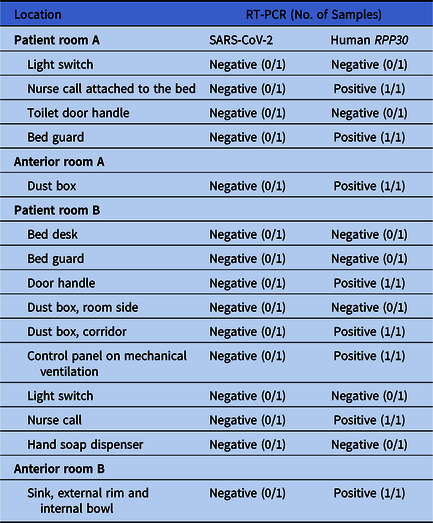
Note. PCR, polymerase chain reaction; RPP30, ribonuclease P 30 subunit; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
After the patient left room A, he resided in room B for 20 days. Ten environmental samples were collected after cleaning. All 10 samples from room B were negative for SARS-CoV-2 and were positive or negative for RPP30 (Table 1).
SARS-CoV-2 is detectable in several types of clinical samples including bronchial lavage fluid, nasopharyngeal swab, pharyngeal swab, sputum, saliva, and feces.Reference Wang, Xu, Gao, Lu, Han, Wu and Tan4,Reference To, Tsang and Chik-Yan Yip5 Transmission of SARS-CoV-2 via surfaces in hospitals is of great concern to medical staff and patients. Blocking the potential routes of transmission is essential for preventing the spread of SARS-CoV-2.Reference Kampf, Todt, Pfaender and Steinmann6 A recent study showed that environmental contamination can occur via contact with patients with SARS-CoV-2 and upper respiratory tract symptoms.Reference Ong, Tan and Chia7 After cleaning, all areas were negative for SARS-CoV-2; therefore, thorough cleaning is sufficient for SARS-CoV-2 decontamination.
This study had several limitations. First, RT-PCR was not performed before cleaning because of the risk of nosocomial transmission. Therefore, a comparison of the viral loads of high-touch areas before and after cleaning is required. Second, this study involved a single patient, and further studies are required to confirm these findings.
In summary, our data indicate the effectiveness of environmental cleaning for SARS-CoV-2 decontamination. This information is useful for infection control strategies and may alleviate the concerns of medical staff.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/ice.2020.144
Acknowledgments
We thank all of the medical and ancillary hospital staff and the patients for consenting to participate. We thank Suzanne Leech, PhD, from the Edanz Group for editing a draft of this manuscript.
Financial support
This study was supported by a Grant-in-Aid for the Genome Research Project from Yamanashi Prefecture (to M.O. and Y.H.), the Japan Society for the Promotion of Science (JSPS) KAKENHI Early-Career Scientists (grant no. JP18K16292 to Y.H.), a Research Grant for Young Scholars (to Y.H.), the YASUDA Medical Foundation (to Y.H.), the Uehara Memorial Foundation (to Y.H.), and Medical Research Grants from the Takeda Science Foundation (to Y.H.).
Conflicts of interest
All authors report no conflicts of interest relevant to this article.




