A growing body of evidence indicates that the incidence of psychosis varies widely across countries, with an over fivefold variation in rate distributions.Reference McGrath, Saha, Chant and Welham1-Reference Saha, Chant, Welham and McGrath4 Research findings to date indicate a prominent age and gender variation.Reference Faraone, Chen, Goldstein and Tsuang5-Reference Kennedy, Boydell, Kalidindi, Fearon, Jones and van Os13 A substantial variation in incidence has also been reported relating to immigration statusReference Cantor-Graae and Selten14,Reference Bourque, van der Ven and Malla15 and ethnicity.Reference Selten, Veen, Feller, Blom, Khan and Schols16-Reference Fearon, Kirkbride, Morgan, Dazzan, Morgan and Lloyd20 Considerable variations in urban-rural distribution have also been observed, with schizophrenia and other non-affective psychoses incidence rates being higher in urban v. rural areas.Reference van Os21-Reference McGrath and Scott23 Several factors have been hypothesised as potential mediators of this urbanicity effect,Reference Allardyce and Boydell24 one of the most robust being intra-city social deprivation.Reference Croudace, Kayne, Jones and Harrison25-Reference Zammit, Lewis, Rasbash, Dalman, Gustafsson and Allebeck28 Most estimates published to date, however, have come from studies conducted in northern-central Europe or in North America,Reference McGrath, Saha, Chant and Welham1,Reference Saha, Chant, Welham and McGrath3 and very little reliable information is available from research carried out in southern Europe.Reference Pelayo-Terán, Pérez-Iglesias, Ramírez-Bonilla, González-Blanch, Martínez-García and Pardo-García29 In particular, Italy has produced scarce reliable data on the incidence of psychotic disorders, and the information that is available was drawn from case register studies conducted in the 1990s on small-scale geographically delimited areas,Reference De Salvia, Barbato, Salvo and Zadro30,Reference Balestrieri, Rucci and Nicolaou31 or from first-admission studies.Reference Preti and Miotto32 A recent epidemiologically based Italian studyReference Tarricone, Mimmi, Paparelli, Rossi, Mori and Panigada33 covered an exclusively metropolitan area and did not address the issues of urban-rural differences or the influence of socioeconomic deprivation on first-episode psychosis incidence. It is also important to note, however, that the heterogeneity reported in the literature may be justified by variations in methodological approaches.Reference Kirkbride, Errazuriz, Croudace, Morgan, Jackson and Boydell34 Thus, to reliably estimate incidence rates, research in this field should meet a series of requirements, such as: a well-defined sociodemographic catchment area; the recruitment of all individuals with a first episode from the general population or at least from any available health service; assessment and diagnostic process that show adequate levels of validity and reliability; and control for any confounding factor.Reference Jablensky, Hirsch and Weinberger35 Therefore, the present study was undertaken to estimate incidence rates for both schizophrenia spectrum disorders and affective psychoses, in a large-scale, epidemiologically defined catchment area of the Veneto region, north-eastern Italy. We also aimed to explore the role of the above-described putative risk factors of age, gender, immigration status, degree of urbanicity and socioeconomic deprivation on incidence rates of psychoses.
Method
Design
This is an epidemiologically based survey conducted within the framework of the Psychosis Incident Cohort Outcome Study (PICOS), a multisite naturalistic study aiming to examine the relative role of clinical, social, genetic and morphofunctional factors in predicting clinical and social outcomes in a large cohort of people with first-episode psychosis, treated by public mental health services located in the Veneto region.Reference Bertani, Lasalvia, Bonetto, Tosato, Cristofalo and Bissoli36,Reference Lasalvia, Tosato, Brambilla, Bertani, Bonetto and Cristofalo37
The care context and the participating sites
Mental healthcare in Veneto is delivered by the National Health Service (NHS) through its Departments of Mental Health (DMHs), which are responsible for the provision of comprehensive and integrated care to the adult population living in a geographically defined catchment area (approximately 250 000-300 000 inhabitants). Within each DMH’s catchment area, two or three community mental health centres (CMHCs) provide out-patient care, day care and rehabilitation to a target population of nearly 100 000 inhabitants living in a geographically defined subsector. The DMHs located in rural contexts usually encompass a number of different municipalities (small towns and villages) within their catchment areas, whereas for the DMHs located in urban contexts their catchment areas usually correspond to one or more neighbourhoods.
Overall, 25 collaborating sites took part in PICOS; they were homogeneously distributed across the regional territory and included either whole DMHs (n = 9) or single CMHCs (n = 16). For the specific purposes of the present study, the PICOS area examined was restricted to an area covered by the 13 sites (4 DMHs and 9 CMHCs) that had ensured reliable coverage of their respective catchment areas during the index period (1 January 2005 to 31 December 2007). These sites were selected on the basis of recruitment procedure accuracy, as shown by a ‘leakage’ study conducted within each participating site and aimed at identifying any cases missed through routine recruitment procedures (see below). Although leading to a restriction of the overall PICOS catchment area, this criterion guaranteed the inclusion of all potentially eligible cases.
Case ascertainment
All psychiatric facilities located in the regional area covered by PICOS were asked to refer to the research team all potential individuals with psychosis at first-service contact during the index period. No categorical diagnostic criteria for entry into the study were adopted. Based on the methodology adopted in the World Health Organization ten-country study,Reference Jablensky, Sartorius, Ernberg, Anker, Korten and Cooper38 the inclusion criteria were: (a) age 15-54 years; (b) residence in the Veneto Region; (c) presence of (i) at least one of the following symptoms: hallucinations, delusions, qualitative speech disorder, qualitative psychomotor disorder, bizarre or grossly inappropriate behaviour, or (ii) at least two of the following symptoms: loss of interest, initiative and drive, social withdrawal, episodic severe excitement, purposeless destructiveness, overwhelming fear, marked self-neglect; and (d) first lifetime contact with any mental health service located in the PICOS area during the study period occasioned by symptoms enumerated in (c). The exclusion criteria were: (a) prior treatment with an antipsychotic agent for more than 3 months; (b) mental disorders as a result of a general medical condition; and (c) moderate to severe intellectual disability. The screening instrument was administered to all potentially eligible individuals as soon as possible after their first-service contact (and in all cases within 30 days from first contact). The instrument was completed by face-to-face interview with the patient and for those who declined on the basis of case notes and information from clinical staff.
Routine case ascertainment was conducted through ongoing liaison between the PICOS research team at each participating mental health service. Local clinical staff were encouraged to refer all people who met the initial screening criteria to the study offices, using a variety of agreed routes including telephone, 24-hour answering services, postal pro-forma and dedicated fax returns. There was regular telephone or face-to-face contact between study teams and both the in-patient and community mental health teams serving the population at risk. Regular training events for clinical teams ensured that all staff knew about PICOS, regardless of staff turnover. Promotional materials were made available in all clinical settings to ensure awareness and continuation of referrals, and presentations were made to user and carer groups within the relevant areas. A ‘leakage study’, based on the method adopted in the Aetiology and Ethnicity in Schizophrenia and Other Psychoses (ÆSOP) study,Reference Fearon, Kirkbride, Morgan, Dazzan, Morgan and Lloyd20 was also undertaken to identify any cases missed through the routine procedures. All electronic and paper information systems were carefully scrutinised for any individuals aged 15-54 years, presenting to the services for the first time during the index period with a clinical diagnosis of psychosis. This information was compared with case records to confirm eligibility.
Immigration status was ascribed using all available information, including self-ascription (i.e. declared nationality). All non-Italian participants (including White non-Italians, predominantly from Eastern Europe) were classified as ‘immigrant’ and Italians as ‘native Italian’. Internal immigration from south to north Italy was not considered here (all Italian participants were included in the native Italian category), nor the generation of immigrants (all non-Italian participants were classified as immigrant regardless of whether they were first- or second-generation).
Diagnostic procedure
The formal best-estimate research diagnosis was made 6 months after inception We completed the Item Group Checklist (IGC) of the Schedule for Clinical Assessment in Neuropsychiatry (SCAN)39 for all patients recruited in the study, based on case notes and information from clinical staff. The ICD-10 diagnoses40 were made by consensus agreement from a panel of clinicians, including a principal investigator and the clinical researcher who conducted the individual assessments. Only patients with a confirmed ICD-10 diagnosis of psychosis (F1x.4; F1x.5, F1x.7, F20-29, F30.2, F31.2, F31.5, F31.6, F32.3, F33.3) were finally included in the study. For the purposes of analysis, the specific ICD-10 codes were categorised as follows: all psychoses (F1x.4, F1x.5, F1x.7, F20-29, F30.2, F31.2, F31.5, F31.6, F32.3, F33.3), non-affective psychosis (F1x.4, F1x.5, F1x.7, F20-29), and affective psychosis (F30.2, F31.2, F31.6, F31.5, F32.3, F33.3). Consistent with previous research,Reference Kirkbride, Fearon, Morgan, Dazzan, Morgan and Tarrant8,Reference Tarricone, Mimmi, Paparelli, Rossi, Mori and Panigada33 separate analyses were also conducted for schizophrenia (F20 and F25), bipolar disorder/psychotic mania (F30.2, F31.2, F31.6, F31.5) and psychotic depression (F32.3, F33.3).
Population at risk
The data on population-at-risk for each site were obtained from the Regional Statistical System of the Veneto Region, which gives the official annual estimates every 1 January.41 The length of recruitment (1 January 2005 to 31 December 2007) was not homogeneous across sites: specifically, the majority of sites (n = 9) recruited participants during the whole 36-month period, but one site recruited for 12 months, one for 20, one for 40 and one for 42. To take into account these different lengths, the mid-period population living in the catchment area of each site was multiplied by the number of months/12. The total population at-risk was obtained by summing up these 13 subpopulations, thus giving a total number of person-years of 3 077 555.
Neighbourhood-level variables
The 198 municipalities located within the PICOS catchment area (4 cities - Verona, Padua, Vicenza, Treviso, with respectively 260 000, 210 000, 114 000 and 82 000 inhabitants - and a series of smaller towns with an average of 7800 inhabitants (s.d. = 6700))41 were classified according to the Italian degree of urbanisation: high level (population density >500 per km2 and more than 50 000 inhabitants), medium level (population density between 100 and 500 per km2 and more than 50 000 inhabitants or being next to a high level area) and low level (population density <100 per km2 and not being completely surrounded by medium or high level areas).42
Level of community socioeconomic deprivation was described using an ecological socioeconomic deprivation index developed and validated by our group (see Tello et al Reference Tello, Mazzi, Tansella, Bonizzato, Jones and Amaddeo43 and Donisi et al Reference Donisi, Jones, Pertile, Salazzari, Grigoletti and Tansella44 for further details). In brief, this index includes nine census variables: married individuals; separated or divorced or widowed; single-parent families; elementary school-level education; university qualification; living in rented accommodation; employment in the industrial sector; civil servants or people employed in the tertiary sector; and unemployed. All these variables were calculated as proportions in the census blocks (for example percentage of people in a census block who were legally married, etc.). The resulting score distribution (i.e. continuous socioeconomic deprivation index) was then divided into four groups (from I - affluent, to IV - deprived), identified at the 20th, 50th and the 80th percentiles (i.e. discrete socioeconomic deprivation index). Patients’ addresses were geocoded using The Google Geocoding API (V3). The geocoded address of each participant was linked to a specific socioeconomic deprivation score through their own census block of residence.
Statistical analysis
Overall and gender- and age-specific incidence rates per 100 000 person-years for all psychoses, non-affective psychosis, affective psychosis and schizophrenia were calculated with their 95% confidence intervals for total population, together with urbanicity- and socioeconomic deprivation-specific incidence rates (and 95% confidence intervals). The different population structure of native Italians and immigrants was taken into account by direct standardisation to the total population of Italy in 2011 (Italian Census population), thus obtaining age- and/or gender-adjusted incidence rates. Unadjusted and adjusted for age, gender and immigration incidence rate ratios (IRRs) with 95% confidence intervals were calculated by using Poisson regression (’xi: poisson’ Stata 11.2 command on Windows). Interaction term was fitted between age and gender where appropriate and tested by likelihood ratio test.
Results
Over the study period, a total of 558 patients were diagnosed as having any ICD-10 psychotic disorder. Table 1 shows the study sample’s demographic characteristics and information on the denominator population. Participants were significantly younger, more likely to come from the immigrant population and more likely to come from a socioeconomically deprived area than the denominator population; no gender differences were found. Regarding the distribution of cases by gender and diagnosis (Table 2), men were overrepresented among patients with schizophrenia (F20 and F25) (64.3% males v. 35.7% females), whereas women were overrepresented within the affective psychosis group (65.8% females v. 34.2% males).
Table 1 Basic demographic characteristics of numerator and denominator populations
| Psychosis n (%) (n = 558) | Mid-period person-yearsFootnote a n (%) (n = 3 077 555) | χ2 test, P | |
|---|---|---|---|
| Gender | |||
| Male | 286 (51.3) | 1 579 168 (51.3) | NS |
| Female | 272 (48.7) | 1 498 387 (48.7) | |
| Age group,Footnote b years | |||
| 15-19 | 30 (5.4) | 251 948 (8.2) | <0.001 |
| 20-29 | 187 (33.6) | 617 352 (20.1) | |
| 30-39 | 203 (36.4) | 947 514 (30.8) | |
| 40-49 | 111 (19.9) | 902 174 (29.3) | |
| 50-54 | 26 (4.7) | 358 557 (11.6) | |
| Immigration | |||
| Native Italian | 431 (77.2) | 2 721 675 (88.4) | <0.001 |
| Immigrant | 127Footnote c (22.8) | 355 880 (11.6) | |
| UrbanicityFootnote b, Footnote d | |||
| Low/medium | 285 (51.4) | 1 557 072 (50.6) | NS |
| High | 269 (48.6) | 1 520 483 (49.4) | |
| Socioeconomic deprivation | |||
| I (affluent) | 59 (10.6) | 363 250 (11.8) | <0.001 |
| II | 151 (27.0) | 994 458 (32.3) | |
| III | 214 (38.4) | 1 326 134 (43.1) | |
| IV (deprived) | 134 (24.0) | 393 713 (12.8) |
NS, not significant.
a. Data from January 1 for the years 2005, 2006, 2007 and 2008.41
b. One missing for age group and four missing for urbanicity.
c. Eastern Europe 46.5%; Central Africa 25.2%; North Africa 9.4%; South America 7.1%; Sri Lanka-India 6.3%; China 5.5%.
d. Data from Istituto Nazionale di Statistica.42 The Psychosis Incident Cohort Outcome Study includes 198 municipalities (4.5% low degree, 79.3% medium degree and 16.2% high degree of urbanisation).
Table 2 Distribution of cases by diagnosis (ICD-10) and gender (n = 558)
| n (%) | ||
|---|---|---|
| Diagnosis (ICD-10 codes) | Male | Female |
| Non-affective psychosis | 246 (55.8) | 195 (44.2) |
| Drug-related psychosis (F11-19) | 5 (83.3) | 1 (16.7) |
| Schizophrenia (F20) | 79 (65.3) | 42 (34.7) |
| Schizotypal disorder (F21) | 6 (60.0) | 4 (40.0) |
| Delusional disorder (F22) | 39 (48.1) | 42 (51.9) |
| Brief psychotic disorder (F23) | 48 (48.0) | 52 (52.0) |
| Schizoaffective disorder (F25) | 31 (62.0) | 19 (38.0) |
| Psychosis not otherwise specified (F28-29) | 38 (52.0) | 35 (48.0) |
| Affective psychosis | 40 (34.2) | 77 (65.8) |
| Bipolar disorder/mania with psychotic features (F30-31) | 16 (33.3) | 32 (66.7) |
| Depression with psychotic features (F32.3-33.3) | 24 (34.8) | 45 (65.2) |
| Total | 286 (51.3) | 272 (48.7) |
Incidence by diagnosis, gender and age
Table 3 (bottom row) shows the incidence rates for all psychoses and for the various diagnostic groups. Table 3 (upper part) also shows age- and gender-specific incidence rates. Although no significant male-female differences emerged for all psychoses, incidence rates were significantly higher for females in the 40-49 year age range (IRR = 2.11, 95% CI 1.40-3.21) and for males in the youngest age range 15-19 years (IRR = 2.58, 95% CI 1.11-6.70). In terms of distribution by diagnosis and gender, the non-affective psychosis group showed a similar incidence rate for men and women, but the incidence rate was higher for men (IRR = 1.71, 95% CI 1.25-2.34) with schizophrenia. Conversely, in the affective psychosis group, women showed a higher incidence rate than men (IRR = 2.04, 95% CI 1.39-2.94).
Table 3 Incidence rates per 100 000 person-years (95% CI) for gender, age, urbanicity and socioeconomic deprivation by diagnosis in the total populationFootnote a
| Incident rates per 100 000 person years (95% CI) | ||||||
|---|---|---|---|---|---|---|
| All psychosis | Non-affective psychosis | Schizophrenia | Affective psychosis | Bipolar disorder/ mania | Depression | |
| Gender | ||||||
| Male | 18.1 (16.1-20.3) | 15.6 (13.7-17.6) | 7.0 (5.7-8.4) | 2.5 (1.8-3.4) | 1.0 (0.6-1.6) | 1.5 (1.0-2.3) |
| Female | 18.1 (16.1-20.4) | 13.0 (11.2-15.0) | 4.1 (3.1-5.2) | 5.1 (4.1-6.4) | 2.1 (1.5-3.0) | 3.0 (2.2-4.0) |
| Age at first contact, years | ||||||
| 15-19 | 11.9 (8.0-17.0) | 10.3 (6.7-15.1) | 5.9 (3.3-9.8) | 1.6 (0.4-4.1) | 1.2 (0.2-3.5) | 0.4 (0.0-2.2) |
| 20-29 | 30.3 (26.1-35.0) | 25.1 (21.3-29.4) | 10.8 (8.4-13.8) | 5.2 (3.5-7.3) | 2.6 (1.5-4.2) | 2.6 (1.5-4.2) |
| 30-39 | 21.4 (18.6-24.6) | 16.8 (14.3-19.6) | 6.0 (4.6-7.8) | 4.6 (3.4-6.2) | 1.7 (1.0-2.7) | 3.0 (2.0-4.3) |
| 40-49 | 12.3 (10.1-14.8) | 9.1 (7.2-11.3) | 2.8 (1.8-4.1) | 3.2 (2.1-4.6) | 1.1 (0.5-2.0) | 2.1 (1.3-3.3) |
| 50-54 | 7.2 (4.7-10.6) | 5.0 (3.0-7.9) | 1.9 (0.8-4.0) | 2.2 (1.0-4.4) | 0.8 (0.2-2.4) | 1.4 (0.4-3.2) |
| Urbanicity | ||||||
| Low/medium | 18.3 (16.2-20.6) | 14.6 (12.7-16.6) | 5.1 (4.0-6.3) | 3.7 (2.8-4.8) | 1.3 (0.8-2.0) | 2.4 (1.7-3.3) |
| High | 17.7 (15.6-19.9) | 13.5 (11.8-15.5) | 6.0 (4.9-7.4) | 4.2 (3.2-5.3) | 2.0 (1.4-2.9) | 2.2 (1.5-3.0) |
| Socioeconomic deprivation | ||||||
| I (affluent) | 16.2 (12.4-20.9) | 12.9 (9.5-17.2) | 5.5 (3.4-8.5) | 3.3 (1.7-5.8) | 1.4 (0.4-3.2) | 1.9 (0.8-4.0) |
| II | 15.2 (12.9-17.8) | 11.4 (9.4-13.7) | 5.5 (4.2-7.2) | 3.8 (2.7-5.2) | 1.9 (1.1-3.0) | 1.9 (1.1-3.0) |
| III | 16.1 (14.0-18.4) | 13.0 (11.1-15.1) | 5.3 (4.1-6.7) | 3.2 (2.3-4.3) | 1.1 (0.6-1.8) | 2.1 (1.4-3.0) |
| IV (deprived) | 34.0 (28.0-40.3) | 27.7 (22.7-33.4) | 6.6 (4.3-9.7) | 6.3 (4.1-9.4) | 2.5 (1.2-4.7) | 3.8 (2.1-6.9) |
| Total | 18.1 (16.7-19.7) | 14.3 (13.0-15.7) | 5.6 (4.7-6.4) | 3.8 (3.1-4.6) | 1.6 (1.1-2.1) | 2.2 (1.7-2.8) |
a. Gender-, age-, urbanicity- and socioeconomic deprivation-specific numbers of person-years at risk were used.
Figure 1 shows the incidence rates by diagnosis, gender and age. The incidence peak in schizophrenia (Fig. 1(c)) occurred in the 20-29 age range for both men (14.0, 95% CI 10.1-18.7) and women (6.9, 95% CI 4.3-10.6), with men showing an incidence rate that was 3.75 times higher (95% CI 1.10-20.72) than that of women in the youngest age range (15-19 years). Affective psychosis incidence (Fig. 1(d)) peaked at the 30-39 year age range for men (3.5, 95% CI 2.0-5.6) and at 20-29 years for women (7.3, 95% CI 4.6-11.0).
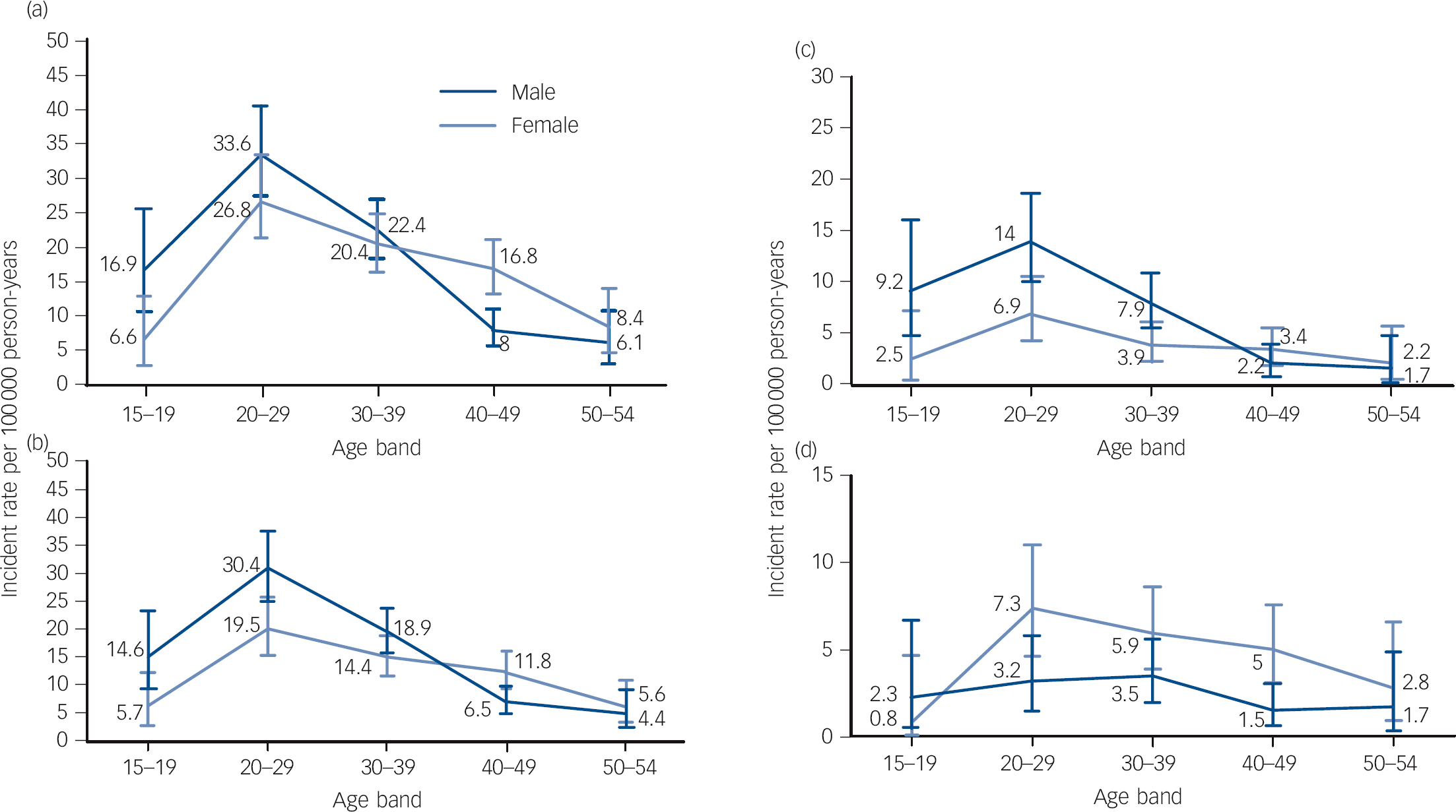
Fig. 1 Incidence rates by diagnosis, gender and age: (a) all psychoses, (b) non-affective psychoses, (c) schizophrenia, (d) affective psychoses.
Incidence by urbanicity and socioeconomic deprivation
As shown in the lower part of Table 3, no distribution diagnosis differences were observed for degree of urbanicity (low/medium v. high level). Yet, a comparison of incidence rates for socioeconomic deprivation yielded significant differences: the incidence rates for all psychoses in the most deprived areas was found to be two times higher than those observed in the other areas (IRR = 2.09, 95% CI 1.54-2.85). The non-affective psychosis category exclusively accounted for this difference, whereas the other diagnostic groups yielded no differences.
Incidence by immigration status
Age- and gender-specific incidence rates by immigration status are shown in Table 4.
Table 4 Age- and/or gender-adjusted incidence rates per 100 000 person-years (95% CI) for gender and age by diagnosis in the native Italian and the immigrant subpopulations
| Incidence rates per 100 000 person-years (95% CI) | ||||||||
|---|---|---|---|---|---|---|---|---|
| All psychoses | Non-affective psychosis | Schizophrenia | Affective psychosis | |||||
| Native Italians | Immigrants | Native Italians | Immigrants | Native Italians | Immigrants | Native Italians | Immigrants | |
| GenderFootnote a | ||||||||
| Male 16.6 (14.5-18.9) | 23.4 (20.8-26.1) | 14.0 (12.1-16.1) | 20.9 (18.5-23.5) | 6.7 (5.4-8.2) | 6.6 (5.2-8.1) | 2.6 (1.8-3.6) | 2.5 (1.8-3.6) | |
| Female | 15.0 (13.0-17.3) | 39.1 (35.7-42.7) | 10.9 (9.2-12.9) | 28.9 (26.0-32.0) | 3.0 (2.1-4.1) | 12.8 (10.9-14.9) | 4.1 (3.1-5.4) | 11.3 (9.6-13.4) |
| Age at first contact,Footnote b years | ||||||||
| 15-19 | 11.9 (7.9-17.4) | 12.0 (8.0-17.7) | 10.2 (6.4-15.2) | 16.1 (11.4-22.5) | 5.7 (3.1-9.8) | 8.3 (4.8-12.8) | 1.8 (0.5-4.5) | 0.0 (0.0-0.0) |
| 20-29 | 25.6 (21.4-30.4) | 54.9 (48.5-62.0) | 21.6 (17.8-26.0) | 43.9 (38.2-50.3) | 10.2 (7.6-13.3) | 14.2 (11.0-17.9) | 4.0 (2.5-6.2) | 11.0 (8.3-14.4) |
| 30-39 | 18.9 (16.0-22.1) | 36.9 (32.6-41.8) | 14.7 (12.2-17.6) | 29.9 (26.0-34.3) | 5.1 (3.6-6.9) | 11.7 (9.3-14.5) | 4.2 (2.9-5.9) | 7.9 (5.9-10.2) |
| 40-49 | 11.3 (9.1-13.8) | 26.0 (22.5-29.6) | 8.2 (6.4-10.4) | 19.8 (16.9-23.1) | 2.4 (1.5-3.7) | 7.2 (5.6-9.4) | 3.0 (2.0-4.5) | 6.1 (4.5-8.0) |
| 50-54 | 7.0 (4.5-10.5) | 11.3 (8.0-15.4) | 5.0 (2.9-8.0) | 5.9 (3.8-9.3) | 1.8 (0.6-3.8) | 5.9 (3.8-9.3) | 2.0 (0.8-4.2) | 5.3 (3.1-8.2) |
| OverallFootnote c | 15.8 (14.4-17.4) | 31.1 (29.0-33.4) | 12.5 (11.2-13.9) | 24.9 (23.0-26.9) | 4.9 (4.1-5.8) | 9.7 (8.5-11.0) | 3.3 (2.7-4.1) | 6.9 (5.9-8.0) |
a. The gender-specific incidence rates are age-adjusted to the 2011 Census Italian population.
b. The age-specific incidence rates are gender-adjusted to the 2011 Census Italian population.
c. Age and gender adjusted to the 2011 Census Italian population.
Immigrants had markedly high incidence rates compared with the Italian population for all psychoses (IRR = 2.26, 95% CI 1.85-2.75) and for all the diagnostic groups. Specifically, the IRR for non-affective psychosis was 2.28 (95% CI 1.82-2.84), the IRR for schizophrenia was 2.18 (95% CI 1.52-3.13), and the IRR for affective psychosis was 2.18 (95% CI 1.41-3.38).
Raised immigrant incidence rates (as compared with those of the native Italian population) were present in both men and women for overall psychoses, non-affective psychosis and schizophrenia. The affective psychosis category showed a higher incidence rate (as compared with native Italians) for immigrant women only, and no differences for men. It is interesting to note that the immigrant population’s incidence rate for overall psychoses was higher in women than in men (IRR = 1.67, 95% CI 1.45-1.94), whereas no gender differences were detected in the Italian population. The higher immigrant female-male rate ratio for all psychoses was substantially accounted for the affective psychosis category’s six-times higher female incidence rate (IRR = 6.52, 95% CI 2.21-26.04), whereas similar incidence rates by gender were observed in both non-affective psychosis and schizophrenia.
Incidence rate ratios adjusted for gender, age and immigration status
Table 5 presents unadjusted and adjusted IRRs for males v. females, age bands v. 50-54 years and immigrants v. native Italians. The risk pattern found with the unadjusted analyses was maintained controlling for the possible confounders of gender, age and immigration. We observed some evidence of heterogeneity of risk across age and gender groups (likelihood ratio test for age gender interaction) for all psychoses (P = 0.01), non-affective psychosis (P = 0.01) and schizophrenia (P = 0.04) but not for affective psychosis (P = 0.33).
Table 5 Incidence rate ratios (IRRs) for gender, age and immigration status by diagnosis
| Unadjusted IRR (95% CI) | Adjusted IRR (95% CI) | |
|---|---|---|
| GenderFootnote a | ||
| All psychoses | 1.00 (0.85-1.18) | 0.99 (0.84-1.17) |
| Non-affective psychosis | 1.20 (1.00-1.45) | 1.19 (0.99-1.44) |
| Schizophrenia | 1.71 (1.25-2.34) | 1.70 (1.24-2.32) |
| Affective psychosis | 0.49 (0.34-0.72) | 0.49 (0.33-0.71) |
| Age at first contact,Footnote b years | ||
| 15-19 | ||
| All psychoses | 1.64 (0.97-2.78) | 1.57 (0.93-2.65) |
| Non-affective psychosis | 2.06 (1.13-3.75) | 1.96 (1.07-3.57) |
| Schizophrenia | 3.05 (1.24-7.48) | 2.90 (1.18-7.13) |
| Affective psychosis | 0.71 (0.21-2.36) | 0.68 (0.21-2.27) |
| 20-29 | ||
| All psychoses | 4.18 (2.77-6.30) | 3.79 (2.51-5.72) |
| Non-affective psychosis | 5.00 (3.07-8.15) | 4.54 (2.78-7.41) |
| Schizophrenia | 5.56 (2.55-12.11) | 5.09 (2.33-11.12) |
| Affective psychosis | 2.32 (1.07-5.04) | 2.10 (0.96-4.58) |
| 30-39 | ||
| All psychoses | 2.95 (1.96-4.44) | 2.71 (1.80-4.09) |
| Non-affective psychosis | 3.34 (2.05-5.44) | 3.06 (1.88-4.99) |
| Schizophrenia | 3.08 (1.41-6.76) | 2.83 (1.29-6.23) |
| Affective psychosis | 2.08 (0.98-4.42) | 1.93 (0.90-4.11) |
| 40-49 | ||
| All psychoses | 1.70 (1.11-2.60) | 1.64 (1.07-2.52) |
| Non-affective psychosis | 1.81 (1.09-3.02) | 1.75 (1.05-2.91) |
| Schizophrenia | 1.42 (0.61-3.28) | 1.37 (0.59-3.17) |
| Affective psychosis | 1.44 (0.66-3.15) | 1.40 (0.64-3.07) |
| ImmigrationFootnote c | ||
| All psychoses | 2.26 (1.85-2.75) | 1.98 (1.62-2.41) |
| Non-affective psychosis | 2.28 (1.82-2.84) | 1.96 (1.57-2.45) |
| Schizophrenia | 2.18 (1.52-3.13) | 1.84 (1.28-2.65) |
| Affective psychosis | 2.18 (1.41-3.38) | 2.04 (1.32-3.18) |
a. Reference group: females. Adjusted for age and immigration.
b. Reference group: 50-54 years. Adjusted for gender and immigration.
c. Reference group: native Italian. Adjusted for gender and age.
Discussion
Main findings
We found that in the area covered by PICOS the incidence rates for all psychoses (18.1 per 100 000 population per year) and for schizophrenia-spectrum psychoses (14.3 per 100 000 per year) are at the lower end of the range of those reported in the literature.Reference McGrath, Saha, Chant and Welham1,Reference McGrath, Saha, Welham, El Saadi, MacCauley and Chant45 We also found that the incidence rates for all psychoses was higher in young people (20-29 years), immigrants and people living in the most socioeconomically deprived areas; these results are consistent with findings in the literature findings.Reference McGrath, Saha, Chant and Welham1,Reference Kirkbride, Errazuriz, Croudace, Morgan, Jackson and Boydell34 The incidence rates for affective psychoses (3.8 per 100 000 per year) is within the range of those reported in the literature.Reference Sherazi, McKeon, McDonough, Daly and Kennedy46-Reference Lloyd, Kennedy, Fearon, Kirkbride, Mallett and Leff50
Methodological considerations
This study has a number of strengths. First, it was conducted on the largest epidemiologically defined geographical area and on the largest at-risk population ever reported in the literature. Second, the study examined a large epidemiologically based cohort of individuals with first-episode psychosis, including both non-affective and affective psychoses, so as to reduce the probability of selection bias because of diagnostic sampling (thus, separate incidence rates were calculated for schizophrenia, bipolar psychotic mania and psychotic depression). Third, we included people from a wide range of mental health services, recruited using broad inclusion criteria. Finally, unlike some previous studies relying on case register dataReference Harrison, Cooper and Gancarczyk51-Reference Bamrah, Freeman and Goldberg53 or informal case referrals only,Reference Harrison, Glazebrook, Brewin, Cantwell, Dalkin and Fox19 the present study conducted leakage studies to confirm the accuracy of case identification.
This study has also some limitations. First, it provides service-based rates rather than community rates. We may assume, however, that the treated incidence rates observed in the PICOS area could be considered to be an accurate reflection of ‘true’ incidence rates, because the vast majority of patients with psychosis in this area contact public mental health services. Previous research has in fact shown that only a negligible fraction of patients with psychosis in the Veneto region are treated in private hospitals or in private practice alone, and that it is standard practice for general practitioners to refer all individuals with psychosis to public mental health services.Reference Amaddeo, Zambello, Tansella and Thornicroft54 A second limitation is that we did not address all of the potentially important factors that could confound or account for the associations observed (for example cannabis use). We therefore cannot exclude the possibility that our study’s observed associations are as a result of residual confounding. Third, we did not verify whether individuals developing psychosis had actually been ‘exposed’ to the degree of deprivation observed at the neighbourhood level. It is theoretically possible that the role in incidence attributed to neighbourhood-level factors could have been because of other exposure levels.Reference Zammit, Lewis, Rasbash, Dalman, Gustafsson and Allebeck28,Reference Kirkbride, Jones, Ullrich and Coid55 We also did not know whether residential neighbourhoods constituted the relevant exposure neighbourhood for risk; thus, future studies will be required to investigate the impact of time spent in different environments on psychosis risk. Finally, regarding the lack of effect of urbanicity, it is possible that we might not have had sufficient resolution to truly examine this construct in our population, since the measure of urbanicity adopted in this study had very little variation (i.e. most of the municipalities were in the ‘medium’ category). The limitations just described should therefore be considered when interpreting the present findings and making comparisons with the results from other studies.
Comparison with other studies
The incidence rates observed in our study for all psychoses overlaps with that reported by a recent Italian study conducted with a similar methodology.Reference Tarricone, Mimmi, Paparelli, Rossi, Mori and Panigada33 These findings, together with those of earlier research using different methodologiesReference De Salvia, Barbato, Salvo and Zadro30,Reference Tansella, Balestrieri, Meneghelli, Micciolo and Tansella56 consistently indicate that the Italian incidence rates for psychosis are somewhat lower than those found in first-episode studies conducted in other European countries such as the UK,Reference Kirkbride, Fearon, Morgan, Dazzan, Morgan and Tarrant8,Reference Coid, Kirkbride, Barker, Cowden, Stamps and Yang10 Ireland,Reference Scully, Quinn, Morgan, Kinsella, O'Callaghan and Owens49 The Netherlands,Reference Veling, Susser, van Os, Mackenbach, Selten and Hoek18 DenmarkReference Cantor-Graae and Pedersen17 and Sweden.Reference Leão, Sundquist, Frank, Johansson, Johansson and Sundquist57 The ÆSOP studyReference Kirkbride, Fearon, Morgan, Dazzan, Morgan and Tarrant8 (multisite research conducted in London, Nottingham and Bristol) showed the greatest discrepancy with Italian rates; reporting an incidence rate for all psychoses of 34.8 per 100 000 person-years. This discrepancy, however, was mostly as a result of twofold higher rates in London, and the Nottingham and Bristol incidence rates were similar to the Italian ones. The higher London incidence rate may be because of the British capital’s specific socioeconomic metropolitan environment. Italy’s Veneto region, conversely, is a somewhat homogeneously affluent and mixed urban-rural region, with a high degree of social cohesion and low population mobility. This situation renders the present study’s catchment area as less deprived and more ethnically homogeneous than inner London or other European metropolitan neighbourhoods, where the other studies’ incidence rates were estimated. Our incidence rate for all psychoses was also far lower than the rates reported by recent UK studies conducted in early intervention service areas;Reference Cheng, Kirkbride, Lennox, Perez, Masson and Lawrence58,Reference Kirkbride, Stubbins and Jones59 this discrepancy is to be expected, however, given the lower age limit (35 years) of the above-mentioned studies as compared with first-episode studies examining the entire adult age range, such as our own, and the relative age-related decline in risk.
The influence of gender and age
We observed similar incidence rates for all psychoses in men and women. This finding is in contrast with those from some studiesReference Kirkbride, Fearon, Morgan, Dazzan, Morgan and Tarrant8,Reference Tarricone, Mimmi, Paparelli, Rossi, Mori and Panigada33,Reference Scully, Quinn, Morgan, Kinsella, O'Callaghan and Owens49 that reported a higher incidence rate for all psychoses in men. We found a high incidence rate for men only in schizophrenia, and the finding of high incidence rates for schizophrenia in males is a robust one.Reference Aleman, Kahn and Selten7,Reference McGrath, Saha, Welham, El Saadi, MacCauley and Chant45 It is therefore possible that this male-female ratio inconsistency for all psychoses may be as a result of different sample composition in terms of diagnostic categories: in fact, 37% of the sample in Kirkbride et al Reference Kirkbride, Fearon, Morgan, Dazzan, Morgan and Tarrant8 and 48% in Tarricone et al Reference Tarricone, Mimmi, Paparelli, Rossi, Mori and Panigada33 were composed of participants with schizophrenia (which yield a greater male-female ratio), whereas individuals with schizophrenia represented only 30% of our sample. With respect to gender distribution by age, we observed that nearly 80% of all the participants developed the disorder before the age of 39 years, confirming that psychosis is more frequent in young adults.Reference Kirkbride, Fearon, Morgan, Dazzan, Morgan and Tarrant8,Reference Allardyce and Boydell24,Reference Scully, Quinn, Morgan, Kinsella, O'Callaghan and Owens49,Reference Svedberg, Mesterton and Cullberg60,Reference Welham, Thomis and McGrath61 The finding that most (but certainly not all) cases of psychosis tend to manifest by the age of 39 years has direct relevance to the early intervention services that are being implemented in a number of Western nations. In fact, many early intervention services tend to adopt a 39-year upper age limit,Reference Edwards, Harris and Bapat62 which inevitably excludes nearly 20% of people from treatment, most of whom will be only slightly older than this limit, and most of these are women.
The influence of immigration status
We found that patients who were immigrants had a significantly greater incidence rate for all psychoses than their Italian counter-parts. Compared with the native population, immigrant incidence rates were twice as high for all diagnostic groups. Moreover, higher psychosis risk among immigrant groups have been consistently observed in the literature. For example, a meta-analysis of population-based incidence studies of schizophrenia in immigrant populationsReference Cantor-Graae and Selten14 demonstrated that ethnic minorities had an overall increased/higher relative risk of 2.9, as compared with that of the indigenous population. This finding was confirmed by a systematic review,Reference McGrath, Saha, Welham, El Saadi, MacCauley and Chant45 which yielded an overall median rate ratio of 4.6. Our study’s immigrant incidence rate was similar to that reported in previous research in other European countries: it should be noted that most immigrants included in our study came from Eastern Europe (Romania, Albania, Moldova, Serbia, 46.5%), Central Africa (Nigeria, Ghana, 25.2%) and North Africa (Morocco, Tunisia, 9.4%). Our findings should therefore be compared with results drawn from homogeneous ethnic groups.Reference Coid, Kirkbride, Barker, Cowden, Stamps and Yang10,Reference Selten, Veen, Feller, Blom, Khan and Schols16,Reference Cantor-Graae and Pedersen17,Reference Fearon, Kirkbride, Morgan, Dazzan, Morgan and Lloyd20 High rates of schizophrenia and other non-affective psychosis among patients from ethnic minority groups, such as African-Caribbean people,Reference Harrison, Glazebrook, Brewin, Cantwell, Dalkin and Fox19,Reference Bhugra, Leff, Mallett, Der, Corridan and Rudge63 in contrast to those of groups living in their homelandReference Mahy, Mallett, Leff and Bhugra64 highlight the role of societal-level effects, such as discrimination or greater levels of social adversity, as a psychosis risk factor. Immigration is an important life event, and assimilation difficulties may remain ‘chronic’, as conceptualised within the stress-vulnerability model of risk for psychosis, although individual risk is still considered to be mediated through genetic susceptibility.Reference Selten, Cantor-Graae and Kahn65 Socioenvironmental characteristics, which are frequently correlated with socioeconomic deprivation, may be more aetiologically relevant to the risk of psychoses for immigrants. Both protective and risk factors are likely to be involved, perhaps differentially among ethnic groups and at multiple levels of organisation (for example individual and neighbourhood).Reference Coid, Kirkbride, Barker, Cowden, Stamps and Yang10
The influence of urbanicity and socioeconomic deprivation
Urban settings have been previously associated with higher rates of schizophrenia and related psychoses,Reference Krabbendam and van Os22 although evidence of their effect on affective psychoses has been less clear.Reference Kaymaz, Krabbendam, de Graaf, Nolen, Ten Have and van Os66 Our study showed that the incidence of both non-affective psychosis and affective psychosis is not significantly higher in individuals living in urban areas at the time of illness onset. This finding is not surprising and confirms the results of a previous case register study comparing urban-rural differences in Italy’s Veneto region,Reference Thornicroft, Bisoffi, De Salvia and Tansella67 which showed no significant differences. Factors thought to be associated with a higher urban risk for psychosis include not only stresses related to urban life or early viral exposure, but also social factors such as social fragmentation, isolation and inequality, and their relationship to genetic liability.Reference van Os21 The specific characteristics of the Veneto region, which presents few urban-rural differences in key social variables, such as social disintegration, emigration and level of social network, might account for the observed lack of an association between incidence of psychosis and urbanicity. On the other hand, level of socioeconomic deprivation appears to more strongly influence incidence of psychosis. In fact, our findings indicate that individuals living in the most deprived areas had a higher risk of non-affective psychosis, whereas no differences were found for affective psychosis. This result is consistent with previous observations that the incidence of non-affective psychosis varies with respect to the environment, but that affective psychosis does not.Reference Kirkbride, Jones, Ullrich and Coid55,Reference Pedersen and Mortensen68 It is possible that, despite some shared genetic liability, the trajectories underlying each type of disorder differ in various ways.Reference Lichtenstein, Yip, Björk, Pawitan, Cannon, Sullivan and Hultman69 Continued efforts to integrate social neuroscience with social epidemiology should help reveal the ways in which environmental exposures over the life course have critical effects on the brain processes that increase psychosis risk.
Further research
This study confirms that the incidence of psychosis varies across countries and in terms of age, gender, immigration status and socioeconomic deprivation. If we are to disentangle the complex puzzle of the aetiopathogenesis of psychosis, a new generation of large-scale, multination, first-inception studies are urgently needed; these, such as the ongoing European Network of Schizophrenia Networks for the Study of Gene-Environment Interactions (EU-GEI) project,70 should be designed with multilevel modelling and should aim to account for both individual-level and environmental-level factors. It is expected that implementation of this type of research, looking at the interplay among environmental, biological and clinical factors, will increase our knowledge about the aetiology of psychoses and, in the near future, will help identify biological markers for use in clinical practice.
Funding
This study was supported by the Ricerca Sanitaria Finalizzata 2004, Giunta Regionale del Veneto with a grant to M.R.; by the Ricerca Sanitaria Finalizzata 2005, Giunta Regionale del Veneto with a grant to A.L.; and by the Fondazione Cariverona with a 3-year grant (Promoting research to improve quality of care. The Verona WHO Centre for mental health research) to the WHO Collaborating Centre for Research and Training in Mental Health and Service Organization at the University of Verona (M.T.).
Acknowledgements
The PICOS-VENETO Group - coordinating staff: M. Tansella M. Ruggeri, A. Lasalvia, M. Bertani, C. Bonetto, P. Brambilla, S. Tosato, D. Cristofalo, G. Marrella, S. Bissoli, C. Perlini. Collaborating sites - Bassano del Grappa: P. Tito, M. Lunardon, F. Gava, E. Borso, L. Grandina, M. Paliotto, L. Roggia. Thiene: A. Danieli, C. Poloni, M. R. Altiero, F. Piazza. Monteccchio M.: E. Ceccato, C. Busana, A. Campi, A. Zanconato. Vicenza 1 UO: P. Zamorani, R. Binotto, A. Caneva, E. Lazzarin, G. Zordan. Vicenza 2 UO: C. Dolce, G. B. Fanchin, C. Negro. Vicenza 3 UO: F. Gardellin, M. Crestale, L. Paiola, A. Sale. Pieve di Soligo: I. Morandin, E. Biondi, A. Cordella G. Favaretto, S. Geatti, P. Urbani. Treviso: M. De Rossi, G. Zanatta, J. Spessotto, R. Penelope, L. Grando, M. Sgnaolin, C. Tozzini, G. Visentin, L. Schiavon. Portogruaro: B. Gentile, M. G. Bolacchi, L. Marzotto, F. Moni, L. Rossi. San Donà di Piave: I. Amalric, C. Miceli, M. R. De Zordo, L. Ramon, S. Russo. Venezia: R. Rossi, G. Casagrande, V. De Nardo, A. Facchetti, F. Ramaciotti. Mirano: V. Marangon, G. Coppola, A. Marcolin, P. Meneghini, F. Sbraccia, C. Segato. Camposampiero: R. Riolo, L. Cappellari, M. Cutugno, L. Meneghetti, L. Longhin, B. Paoleschi. Cittadella: D. Scalabrin, L. Antonello, A. Purgato, G. Santucci, C. Tosin, R. Volpato, R. Zurlo. Padova 2 Serv.: M. Zucchetto, M. Pedron, S. Pinton, M. Benetazzo. Padova 3 Serv.: C. Cremonese, L. Pavan, M. Semenzin, L. Sifari, F. Zorzi. Rovigo: M. M. Martucci, N. Magno, G. Meloni, E. Toniolo. Adria: M. Pavanati, E. Destro, L. Finotti. Verona 1 Serv.: R. Fiorio, A. Marsilio, N. Pedrocco, P. Pollola. Verona 2 Serv.: L. Lazzarotto, F. Nosè, P. Rossin, V. Vivenza. Verona 3 Serv.: A. Lasalvia, M. Bertani, S. Bissoli, K. De Santi, G. Marrella, R. Mazzoncini, M. Ruggeri. Verona 4 Serv.: A. Urbani, L. Bianchi, G. Carcereri, L. Lunardi, G. Migliorini, G. Perdonà, C. Piazza. Legnago: D. La Monaca, G. D’Agostini, I. Boggian, G. Piccione, E. Saladini. Domegliara: F. Gomez, S. Frazzingaro. Isola della Scala: S. Nicolaou, L. Cordioli, G. Bertolazzi, V. Pagliuca. Villa Santa Chiara: M. Abate, M. Bortolomasi, M. Giacopuzzi, M. Segala. Villa Santa Giuliana: F. De Nardi, F. Basetto, C. Bernardis, A. Bezzetto, M. Santi.









eLetters
No eLetters have been published for this article.