Book contents
- Essentials of Pediatric Neuroanesthesia
- Essentials of Pediatric Neuroanesthesia
- Copyright page
- Dedication
- Contents
- Contributors
- Preface
- Chapter 1 Developmental Approach to the Pediatric Neurosurgical Patient
- Chapter 2 Developmental Cerebrovascular Physiology
- Chapter 3 Neuroprotective Strategies in the Pediatric Patient
- Chapter 4 Neuropharmacology
- Chapter 5 Blood Sparing Techniques
- Chapter 6 Regional Anesthesia for Pediatric Neurosurgery
- Chapter 7 Anesthesia for Posterior Fossa Craniotomy
- Chapter 8 Congenital Neurosurgical Lesions
- Chapter 9 Anesthetic Considerations for Deep Brain Stimulator Placement
- Chapter 10 Anesthesia for Fetal Neurosurgery
- Chapter 11 Anesthesia for Craniofacial Surgery
- Chapter 12 Anesthesia for Cerebrovascular Disease in Children
- Chapter 13 Epilepsy Surgery
- Chapter 14 Traumatic Brain Injury
- Chapter 15 Anesthesia for Minimally Invasive Neurosurgery
- Chapter 16 Intraoperative Neuromonitoring in Pediatric Neurosurgery
- Chapter 17 Anesthesia for Neurointerventional Radiology
- Chapter 18 Radiation Therapy
- Chapter 19 Anesthetic-Induced Neurotoxicity
- Chapter 20 Perioperative Salt and Water in Pediatric Neurocritical Care
- Chapter 21 Intensive Care Considerations of Pediatric Neurosurgery
- Index
- References
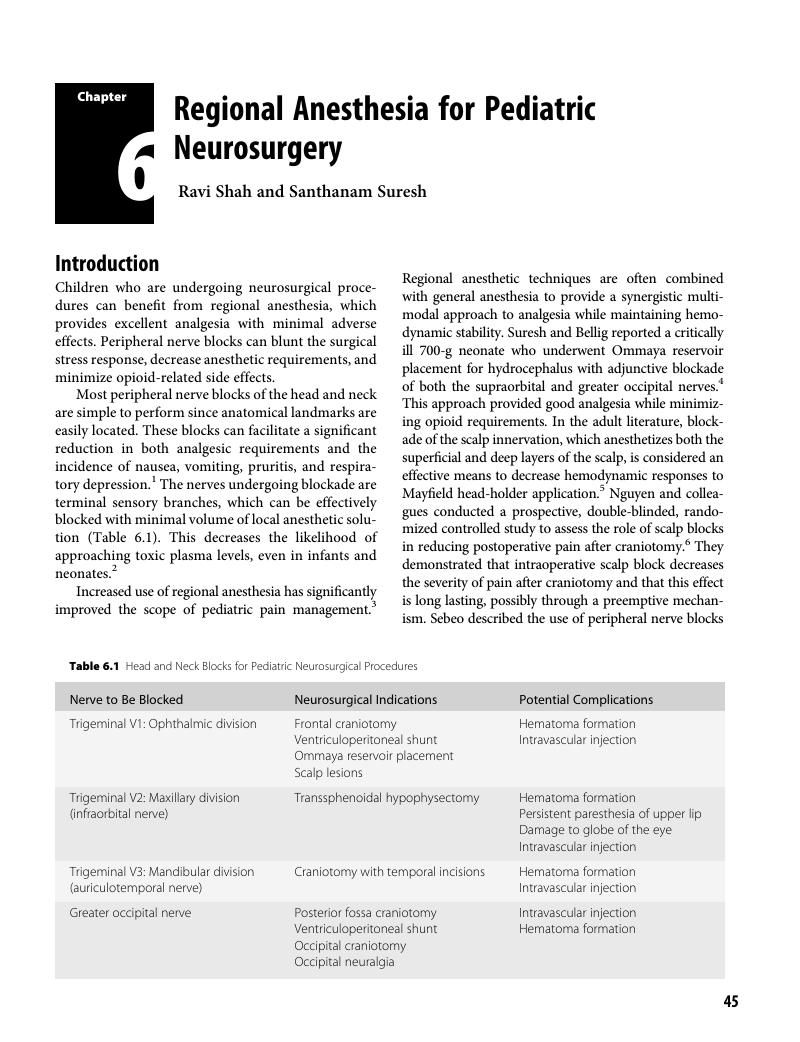
Chapter 6 - Regional Anesthesia for Pediatric Neurosurgery
Published online by Cambridge University Press: 02 November 2018
- Essentials of Pediatric Neuroanesthesia
- Essentials of Pediatric Neuroanesthesia
- Copyright page
- Dedication
- Contents
- Contributors
- Preface
- Chapter 1 Developmental Approach to the Pediatric Neurosurgical Patient
- Chapter 2 Developmental Cerebrovascular Physiology
- Chapter 3 Neuroprotective Strategies in the Pediatric Patient
- Chapter 4 Neuropharmacology
- Chapter 5 Blood Sparing Techniques
- Chapter 6 Regional Anesthesia for Pediatric Neurosurgery
- Chapter 7 Anesthesia for Posterior Fossa Craniotomy
- Chapter 8 Congenital Neurosurgical Lesions
- Chapter 9 Anesthetic Considerations for Deep Brain Stimulator Placement
- Chapter 10 Anesthesia for Fetal Neurosurgery
- Chapter 11 Anesthesia for Craniofacial Surgery
- Chapter 12 Anesthesia for Cerebrovascular Disease in Children
- Chapter 13 Epilepsy Surgery
- Chapter 14 Traumatic Brain Injury
- Chapter 15 Anesthesia for Minimally Invasive Neurosurgery
- Chapter 16 Intraoperative Neuromonitoring in Pediatric Neurosurgery
- Chapter 17 Anesthesia for Neurointerventional Radiology
- Chapter 18 Radiation Therapy
- Chapter 19 Anesthetic-Induced Neurotoxicity
- Chapter 20 Perioperative Salt and Water in Pediatric Neurocritical Care
- Chapter 21 Intensive Care Considerations of Pediatric Neurosurgery
- Index
- References
Summary
- Type
- Chapter
- Information
- Essentials of Pediatric Neuroanesthesia , pp. 45 - 51Publisher: Cambridge University PressPrint publication year: 2018