Introduction
Falls and fall-induced injuries are extremely common among older adults and result in a considerable increase in morbidity and mortality in this age group (Davis et al., Reference Davis, Robertson, Ashe, Liu-Ambrose, Khan and Marra2010; World Health Organization, 2021). Multiple fall-prevention strategies for older people include monitoring contributing factors. These factors may be either intrinsic (changes in the body with aging), extrinsic (environmental conditions, surfaces), or a combination of both (Bleijlevens et al., Reference Bleijlevens, Diederiks, Hendriks, van Haastregt, Crebolder and van Eijk2010; Huang, Reference Huang2005; Mortazavi, Tabatabaeichehr, Taherpour, & Masoumi, Reference Mortazavi, Tabatabaeichehr, Taherpour and Masoumi2018; Unguryanu, Grjibovski, Trovik, Ytterstad, & Kudryavtsev, Reference Unguryanu, Grjibovski, Trovik, Ytterstad and Kudryavtsev2020; Vondracek & Linnebur, Reference Vondracek and Linnebur2009). One of the most deleterious outcomes of aging is musculoskeletal disorders mainly due to significant loss of muscle strength (atrophy, weakness) and flexibility (Phillips & Haskell, Reference Phillips and Haskell1995; Raad, Agre, McAdam, & Smith, Reference Raad, Agre, McAdam and Smith1988; Stathokostas, Little, Vandervoort, & Paterson, Reference Stathokostas, Little, Vandervoort and Paterson2012), reduction of postural control (loss of balance) (Nuzzo, Reference Nuzzo2020; Robertson, Collins, Elliott, & Starks, Reference Robertson, Collins, Elliott and Starks1994), impaired vestibular function (Lin & Bhattacharrya, Reference Lin and Bhattacharrya2012), musculoskeletal efficacy and functional ability (Bruce, Reference Bruce1989; Lord, Murray, Chapman, Munro, & Tiedemann, Reference Lord, Murray, Chapman, Munro and Tiedemann2002).
Physical activity programs can improve older adults’ physical well-being (Eduardo, Ronei, Martim, & Mikel, Reference Eduardo, Ronei, Martim and Mikel2014; Evan, Xiaoyang, & Mahdi, Reference Evan, Xiaoyang and Mahdi2017). Results from a variety of studies have shown that physical therapy intervention can have a positive impact on functional mobility, improve balance in neurological and musculoskeletal disorders, and reduce the levels of pain and the frequency of heart diseases in nursing home residents (Barnett, Smith, Lord, Williams, & Baumand, Reference Barnett, Smith, Lord, Williams and Baumand2003; Lazowski et al., Reference Lazowski, Ecclestone, Myers, Paterson, Tudor-Locke and Fitzgerald1999; Littbrand, Lundin‐Olsson, Gustafson, & Rosendahl, Reference Littbrand, Lundin‐Olsson, Gustafson and Rosendahl2009; Mimi, Tang, Wan, & Vong, Reference Mimi, Tang, Wan and Vong2014; Papathanasiou, Reference Papathanasiou2020; Pepera, Mpea, Krinta, Peristeropoulos, & Antoniou, Reference Pepera, Mpea, Krinta, Peristeropoulos and Antoniou2021). A systematic review by Valenzuela (Reference Valenzuela2012) has demonstrated that progressive resistance training can significantly improve the overall functional status in nursing home older adults.
Exercise interventions may also potentially have an effect on reducing fall risks, though only a small number of randomized controlled trials have evaluated this factor, with no overall benefit identified on falls outcomes. A recent randomized controlled trial (Hewitt, Goodall, Clemson, Henwood, & Refshauge, Reference Hewitt, Goodall, Clemson, Henwood and Refshauge2018) demonstrated a significant reduction in falls in a large sample, including residents with cognitive impairment, in residential care facilities. On the other hand, there is evidence referring that exercise intervention overall makes small or no effect on falls in nursing home residents (Arrieta, Rezola-Pardo, Gil, Irazusta, & Rodriguez-Larrad, Reference Arrieta, Rezola-Pardo, Gil, Irazusta and Rodriguez-Larrad2018; Cameron et al., Reference Cameron, Dyer, Panagoda, Murray, Hill and Cumming2018).
Similarly, there is a lack of well-controlled studies to capture a complete picture of the multidimensional exercise training program effectiveness, based on strength and flexibility, in residents of nursing homes. Only a few of them included different types of exercise in their program (Gomez-Cabello, Ara, Gonzalez-Aguero, Casajus, & Vicente-Rodriguez, Reference Gomez-Cabello, Ara, Gonzalez-Aguero, Casajus and Vicente-Rodriguez2004; Langoni et al., Reference Langoni, Resende, Barcellos, Cecchele, Knob and Silva2019; Rezola-Pardo et al., Reference Rezola-Pardo, Arrieta, Gil, Yanguas, Iturburu and Irazusta2019), whereas the minimum period of intervention, which could be necessary to record changes in physical function in older adults, remains unclear. Despite evidence suggesting that multidimensional exercise training may affect hemodynamic, gait, and balance parameters (Pepera et al., Reference Pepera, Mpea, Krinta, Peristeropoulos and Antoniou2021), little is known of the impact of such training intervention in the overall strength and flexibility status of the older population.
The purpose of the study was to prospectively explore the effectiveness of a short-term, eight-week multidimensional training program in overall strength and flexibility in nursing home residents and one that could be used by physical therapists in clinical practice. The hypothesis of this study was that a short-term, eight-week multidimensional training program can improve strength and flexibility in nursing home residents.
Methods
Research Design
A single-blind, randomized, parallel-group, multi-centre design with pretest and posttest study (NCT04358653, ClinicalTrials.gov) was used. All participants signed an informed consent prior to participation to the study. This study was conducted in five phases: (a) Recruitment, (b) Randomization, (c) Baseline assessment, (d) Intervention (eight weeks), and (e) Second assessment (eight weeks from the start of the intervention). The flow chart of the study design is shown in Figure 1.

Figure 1. Flow chart of the study.
The randomization into groups significantly reduced the bias and aimed to distribute evenly different participants’ characteristics to the groups. The incorporation of a control intervention is helping reduce the internal validity threats (i.e., history effects, maturation effects) and more clearly understand the real effects of the experimental intervention. This study was a part of a bigger study that was approved by the ethics committee of the University of Thessaly (Pepera et al., Reference Pepera, Mpea, Krinta, Peristeropoulos and Antoniou2021).
Sample
The current study is part of a bigger study and the sample has been additionally described in a previous publication (Pepera et al., Reference Pepera, Mpea, Krinta, Peristeropoulos and Antoniou2021). Eligibility criteria were (a) residents of long-term care facilities and (b) 65 years of age or above (World Health Organization, 2021). Exclusion criteria were (a) severe neurological diseases (e.g., multiple sclerosis, cerebrovascular disorders, stroke); (b) dementia; (c) severe heart failure (New York Heart Association class III, IV); (d) severe musculoskeletal diseases (e.g., severe rheumatoid arthritis); and (e) recent surgeries.
A diagnosis of dementia was reported in the participants’ medical files kept in the nursing home files together with their prescribed medication treatment (psychotherapeutic drugs). The absence of dementia and other severe neurological diseases as exclusion criteria was based on the rationale to focus this research on the musculoskeletal disorders related to aging and their responses to an exercise program implementation. Moreover, the population of older adults with dementia is heterogeneous regarding the severity of dementia and number of comorbidities. In this case, more subgroup analyses would be required to detect clinical effects and enhance statistical power (Jongsma, van Bruchem-Visser, van de Vathorst, & Mattace Raso, Reference Jongsma, van Bruchem-Visser, van de Vathorst and Mattace Raso2016).
Participant recruitment
Participant recruitment occurred in three steps. Initially, 48 nursing home residents, both men and women, were recruited from three nursing homes, where they were provided nutritional, medical, and quality-of-life supplies and services. Potential participants were checked for eligibility based on their medical records. Finally, out of the 40 older adults meeting the previously mentioned criteria, 20 were randomly assigned (using random numbers generated by a computer) to the control group and 20 to the rehabilitation group. In both groups, half of the participants reported at least one incidence of falling during the past year. A sample size calculation was performed with the software G*Power 3.1.9.4, and it was described in a previous publication (Pepera et al., Reference Pepera, Mpea, Krinta, Peristeropoulos and Antoniou2021).
Data Collection and Blinding
All assessments and interventions were carried out by the same researchers (qualified physiotherapists). Before testing and training, researchers were trained in using tests and instruments. After each assessment, the data were stored and the researchers had no further access to them. Data were encoded in a spreadsheet and sent to another researcher to perform the data analysis. Lastly, the results were shared among the authors.
Intervention
The intervention program has been described in a previous publication (Pepera et al., Reference Pepera, Mpea, Krinta, Peristeropoulos and Antoniou2021) (Table 1). The experimental group was designed to undergo a supervised exercise training program two days a week for eight consecutive weeks for 45–50 minutes per session. The intervention program was implemented at the nursing homes. The control group did not receive any intervention during that period, and the participants were instructed to pursue their habitual daily life activities.
Table 1. Exercise training program
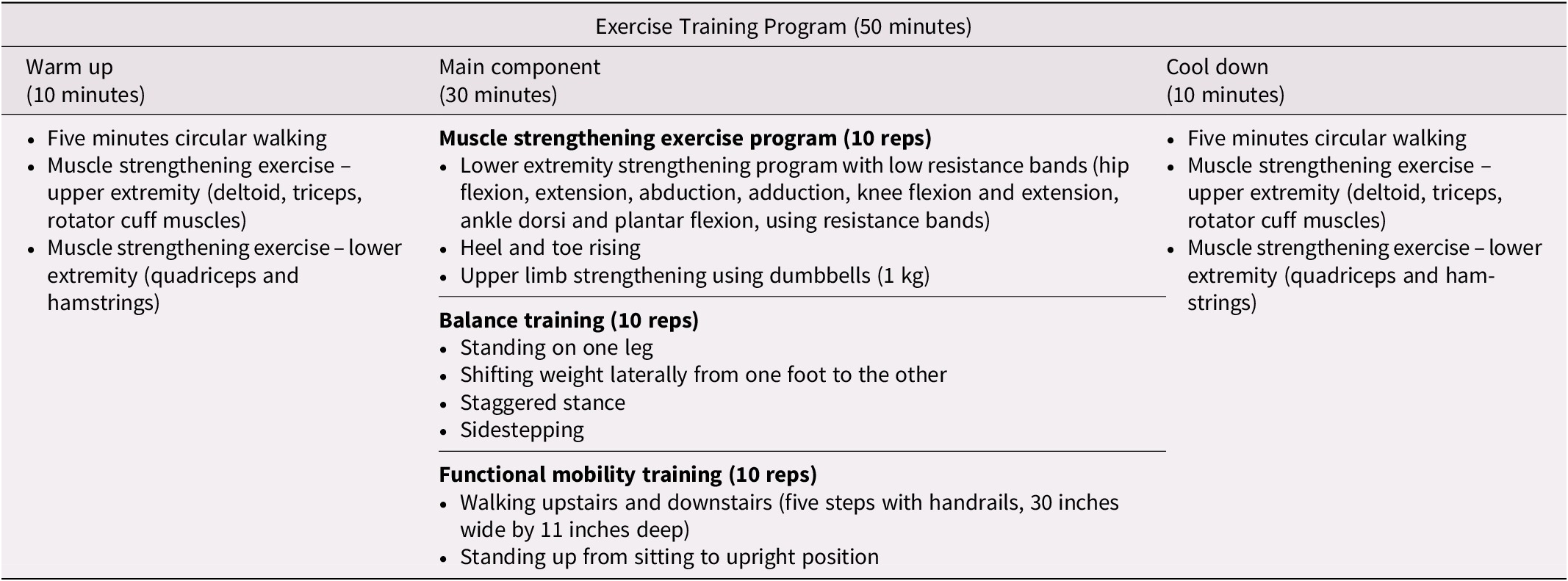
Exercise intensity was monitored using the Borg CR10 scale (Foster et al., Reference Foster, Florhaug, Franklin, Gottschall, Hrovatin and Parker2001). During the exercise intervention, participants were advised to keep up the exercise intensity between 3 (moderate exercise), 4 (somewhat hard exercise), and 5 (hard exercise) of the Borg scale. The Rating of Perceived Exertion (RPE) scale was positioned on the wall in the training room. The exercise intervention was designed to follow the exercise activity guidelines for older adults demonstrated by the American College of Sports Medicine (Garber et al., Reference Garber, Blissmer, Deschenes, Franklin, Lamonte and Lee2011) and American Heart Association (Nelson et al., Reference Nelson, Rejeski, Blair, Duncan, Judge and King2007).
Participants were instructed to refrain from drinking alcohol and caffeine beverages 24 hours before testing and training. Dietary intake wasn’t controlled; however, it was recommended they stay with their usual diet during the period of the study. They were advised to avoid participation in any other exercise program. All evaluations and intervention sessions occurred at the same time each day, between 8:00 a.m. and 10:00 a.m.
Throughout the duration of the study, the participants, as a whole, were supervised and assessed by a qualified physiotherapist and two final-year physical therapy students (20:3, participants to staff ratio). As an exception was the balance training. Participants were divided into five groups of four participants in each, so the participant to staff/supervision ratio was 3:4 each time. Chairs were positioned nearby the participants (not in front of them), and they were allowed to sit on them only while their awaiting the balance training exercises.
Assessments and Outcome Measures
Assessment was based on physical functional measurements that have been shown to be related to falls. Participants were assessed at baseline and after the eight-week exercise program intervention. The following six primary outcome measures were assessed to evaluate the effectiveness of the multidimensional exercise program.
Outcome measures
Apart from the primary outcome measures, other baseline characteristics were measured: (a) anthropometric and demographic data (age, weight, height); (b) comorbid medical conditions; and (c) prior history of falls and fall-related injuries during the past year (World Health Organization, 2008).
Upper extremity strength. This was measured through hand grip strength (HGS) testing, using the SAEHAN hand grip dynamometer (Model SH5001; SAEHAN Corporation, Yangdeok-Dong, Masan, South Korea). The participants were seated on a standard chair with the elbow flexed at 90o. When the participants were ready, they would begin to strain the device in a maximal isometric effort, maintaining, at the same time, high concentration, as this was a required condition for maximal results. No other body movement was allowed during testing (Romero, Bishop, Velozo, & Light, Reference Romero, Bishop, Velozo and Light2011). Test–retest reliability of HGS has been proven to be excellent (intraclass correlation coefficient [ICC] > 0.95, 95% CI), and minimum detectable change (MDC) scores for the hand was 5.0 kg in nursing home residents (Bohannon, Reference Bohannon1998).
Lower extremity strength. This was assessed through the Sit-to-Stand test (STS). Participants were asked to sit on a chair, stand up, and return to the sitting position for five consecutive times at full speed, with no intervals between. The normal time expected for the successful completion of the trial was estimated at 24–27 seconds (Lin & Bhattacharrya, Reference Lin and Bhattacharrya2012; Oliveira Gonçalves et al., Reference Oliveira Gonçalves, Bandeira, Coelho-Júnior, Silva Aguiar, Minucci Camargo and Yukio Asano2019). Reliability of the STS test has been found to be highly significant (ICC > 0.90), and the MDC has been estimated at 2.5 seconds (Bobos, Nazari, Lu, & MacDermid, Reference Bobos, Nazari, Lu and MacDermid2020).
Upper body flexibility. This was assessed through the Back Scratch test (BST). Participants were instructed to bring their hand back as high as possible to reach the seventh cervical vertebra (C7) with the thumb. The distance between the thumb and the seventh cervical vertebra (C7) was measured (Oliveira Gonçalves et al., Reference Oliveira Gonçalves, Bandeira, Coelho-Júnior, Silva Aguiar, Minucci Camargo and Yukio Asano2019). Reliability of the BST has been found to be excellent (ICC > 0.95, 95% CI), whereas the MDC has been estimated at 1.42 cm (Whitney et al., Reference Whitney, Wrisley, Marchetti, Gee, Redfern and Furman2005).
Lower body flexibility. This was assessed using a modified Sit and Reach test (SRT). This test was performed in a standard chair with one leg fully extended and the other in a flexed position. Participants reached forward with one hand as far as possible and held this position for three seconds. The distance between fingers and toes was measured (Rikli & Jones, Reference Rikli and Jones2001). The test–retest reliability of RST has been found to be excellent (ICC > 0.95, 95% CI), whereas the MDC has been estimated at 1.56 cm (Goldberg, Chavis, Watkins, & Wilson, Reference Goldberg, Chavis, Watkins and Wilson2012).
Statistical Analysis
Data analysis
The normality of data was examined using Kolmogorov-Smirnov tests. The comparison of baseline characteristics of participants between study groups was examined with independent t-tests when the data were parametric and with an χ2 when the data were from a nominal scale. The baseline characteristics were described by using means, SDs, number of observations, percentages, and p values.
Multivariate Analysis of Variance (MANOVA) was used to examine the main effects (group effects, time effects) and group*time interactions, considering that a degree of correlation exists between the four dependent variables (HGS, STS, BST, and SRT). MANOVA was performed on a design including two independent variables: one factorial (group: intervention, control) and one repeated measure (time: before, after). Univariate analysis followed multivariate analysis. The effects were expressed by using means, SDs, mean differences, 95 per cent CIs, F statistics, degrees of freedom (dfs), effect size η2, observed power, and p values.
The effectiveness of the control and experimental intervention was also examined by using dependent t-test for each group and by comparing the pre- with the post-scores. The effects were expressed by using means, SDs, mean differences, 95 per cent CIs, per cent change, t statistics, dfs, pre-post correlations (r), and p values.
The significance level was set at p = 0.05. Statistical Package for Social Sciences (SPSS), version 25, was used for all data analyses.
Results
Data were normally distributed (Kolmogorov–Smirnov, p > 0.05). At baseline, the only significant difference between groups was found for SRT (higher in the control group, Mdiff = 1.5 cm; p < 0.05). All the other characteristics were not significantly different between the groups (p > 0.05) (Table 2). None out of the 40 participants (20 for the intervention group and 20 for the control group) dropped out of the study (Pepera et al., Reference Pepera, Mpea, Krinta, Peristeropoulos and Antoniou2021).
Table 2. Baseline characteristics and differences between the groups

Notes. HGS = Hand Grip Strength; STS = Sit-to-Stand Test; BST = Back Scratch Test; SRT = Sit and Reach Test.
Using MANOVA, Box’s Test was found to be non-significant (p = 0.09). Based on Pillai’s Trace, MANOVA revealed a significant between-subjects (group) effect, V = 0.599, F(6, 33) = 8.22, p < 0.001, partial η2 = 0.599, observed power = 1; a significant within-subjects (time) effect, V = 0.336, F(6, 33) = 2.78, p = 0.027, partial η2 = 0.336, observed power = 0.808; and a significant group*time interaction, V = 0.908, F(6, 33) = 54.52, p < 0.001, partial η2 = 0.908, observed power = 1.
Univariate analysis of variance did not reveal a significant time main effect on any variable (p > 0.05). Significant group main effects were observed for SRT (p < 0.05) but not for the other dependent variables (p > 0.05). Significant group*time interactions were observed for all the dependent variables (HGS, STS, BST, SRT) (p < 0.05). The results of univariate analysis and the corresponding pairwise comparisons are analytically presented in Table 3.
Table 3. Results from the univariate analysis of variance

Notes. HGS = Hand Grip Strength; STS = Sit-to-Stand Test; BST = Back Scratch Test; SRT = Sit and Reach Test.
Dependent t-tests showed that all the variables significantly changed from baseline to the end of intervention in both groups (p < 0.05). The only exception was the change of the SRT for the control group, which was found to be non-significant (p > 0.05). Each variable, however, changed in a different direction for the experimental and control group. The effect sizes of the changes for all the variables were found to be small to medium (0.07–0.30) for both groups. The only exception was the effect sizes for the SRT, which were medium to high (0.46–0.93). The results of this pre-post analysis are analytically presented in Table 4.
Table 4. Pre–post differences for each examined variable

Notes. HGS = Hand Grip Strength; STS = Sit-to-Stand Test; BST = Back Scratch Test; SRT = Sit and Reach Test.
No musculoskeletal (muscle strain or joint pain), suicide, cardiovascular, or respiratory adverse-related events to the intervention were reported.
Discussion
A multidimensional exercise program can improve hemodynamic function (blood pressure and heart rate resting), balance, and gait ability in nursing home residents (Pepera et al., Reference Pepera, Mpea, Krinta, Peristeropoulos and Antoniou2021). The present study aimed to assess the effectiveness of a group exercise program in the reduction of important fall risk factors (such as overall strength and flexibility) in care-home residents and to develop a therapeutic exercise program for this population. All fall risk factors showed statistically significant improvement after an eight-week, short-term multidimensional exercise program. Specifically, both strength and flexibility in the lower and upper body were improved in the exercise group, whereas the same rates worsened in the control group.
Functional fitness level is shown to be lower among institutionalized older adults compared with those living independently (Bhattacharya, Deka, & Roy, Reference Bhattacharya, Deka and Roy2016). Thus, there is no surprise that an exercise program will enhance their physical abilities. According to the World Health Organization, 28–34 per cent of people ages 65 years and older will experience at least one incidence of falling every year, a rate that is increased with age and frailty level. With an annual cost of €25 billion EUR in the European Union, falls create a significant negative impact in the society as a whole (Carande-Kulis, Stevens, Florence, Beattie, & Arias, Reference Carande-Kulis, Stevens, Florence, Beattie and Arias2015; Davis et al., Reference Davis, Robertson, Ashe, Liu-Ambrose, Khan and Marra2010; World Health Organization, 2021). Understanding ways to reduce the risk of falling and frailty, especially in the older population, is vital since it can significantly reduce their morbidity and mortality (World Health Organization, 2021).
Many studies have shown that both individual and group programs can similarly reduce the intrinsic risk factors of falling, such as strength, balance, range of motion, and functional mobility in both nursing home settings (Arrieta et al., Reference Arrieta, Rezola-Pardo, Gil, Irazusta and Rodriguez-Larrad2018; Hewitt et al., Reference Hewitt, Goodall, Clemson, Henwood and Refshauge2018; Rezola-Pardo et al., Reference Rezola-Pardo, Arrieta, Gil, Yanguas, Iturburu and Irazusta2019; Sherrington et al., Reference Sherrington, Michaleff, Fairhall, Paul, Tiedemann and Whitney2017) and community settings (Cameron et al., Reference Cameron, Dyer, Panagoda, Murray, Hill and Cumming2018; Carter, Campbell, Sanson-Fisher, Redman, & Gillespie, Reference Carter, Campbell, Sanson-Fisher, Redman and Gillespie1997; De Vries et al., Reference De Vries, Ravensberg, Hobbelen, OldeRikkert and Staal2012; Furtado, Sousa, Simao, Pereira, & Vilaca-Alves, Reference Furtado, Sousa, Simao, Pereira and Vilaca-Alves2015; Gillespie et al., Reference Gillespie, Rodertson, Gillespie, Sherrington, Gates and Clemson2012; Hill & Schwarz, Reference Hill and Schwarz2004; Patel & Pachpute, Reference Patel and Pachpute2015). Taking into consideration that in most cases of falling there is a combination of factors that lead to the fall accident, it is logical that the more factors coexist, the more the risk increases (Gomez-Cabello et al., Reference Gomez-Cabello, Ara, Gonzalez-Aguero, Casajus and Vicente-Rodriguez2004). A prevention program that addresses more risk factors is more effective than one that focuses on just one factor alone (Eduardo et al., Reference Eduardo, Ronei, Martim and Mikel2014). Since exercise can have many positive results on physical, cognitive, and social elements, it is highly surprising that these programs are not commonly used as a standard practice in nursing home residents.
In our study, we found that an eight-week, multidimensional exercise program was capable enough to improve fall risk factors and enhance overall strength and flexibility. In comparison with another study, with a similar sample size, equivalent results in strength, balance, and functional mobility were observed, although in that study the exercise program was far more frequent (Zhuang, Huang, Wu, & Zhang, Reference Zhuang, Huang, Wu and Zhang2014).
The intervention of this study demonstrated that the magnitude of changes was lower in upper extremity strength (0.8 than 5 kg), lower extremity strength (2.2 than 2.5 kg) than the reported MCD values. In contrast, the same intervention exercise program showed higher magnitude of changes in upper body flexibility (1.8 than 1.42 cm) and lower body flexibility (2.4 than 1.56 cm) than the reported MCD values. It was concluded that clinically meaningful changes were observed in flexibility components only.
Α systematic review by Arietta et al. (Reference Arrieta, Rezola-Pardo, Gil, Irazusta and Rodriguez-Larrad2018) suggested that, although there was considerable heterogeneity among studies (seven finally included), multidimensional physical exercise programs are effective on improving physical functioning mobility in nursing home residents. It is also worth mentioning that, based on the results of this study and the similar ones from the study of Hewitt et al. (Reference Hewitt, Goodall, Clemson, Henwood and Refshauge2018), the need to intergrade such multidimensional exercise programs as fall prevention strategies in nursing home residents is highly recommendable.
A systematic review showed that exercise programs based on functional exercises were correlated to an improvement of physical function. However, the impact of the coexistence of visual impairments on fall frequency isn’t clearly defined (Gleeson, Sherrington, & Keay, Reference Gleeson, Sherrington and Keay2014). Similarly, another meta-analysis of 12 studies with 1,292 participants living in nursing homes concluded that exercise programs can prevent falls but not fractures, in this population (Silva, Eslick, & Duque, Reference Silva, Eslick and Duque2013).
Contrary to the results in nursing homes, exercise intervention seems to have a positive impact on fall reduction in community-dwelling older individuals. Specifically, a meta-analysis of 19 studies including 649 participants living in the community, published recently, showed significant improvements in strength and flexibility after exercise programs using elastic bands (Yeun, Reference Yeun2017). In another study in 56 community-dwelling people ages 60–80 years, statistical significant improvement in the timed up and go test (TUG) and the chair stand test of this population was reported (Zhuang et al., Reference Zhuang, Huang, Wu and Zhang2014). Similarly, a recent randomized longitudinal clinical trial study demonstrated that a home-based balance and strength exercise training program significantly reduced the rate of falls in community-dwelling older people with a history of falling (Liu-Ambrose et al., Reference Liu-Ambrose, Davis, Best, Dian, Madden and Cook2019). This, however, was a single-centre study and such bias can limit ability for generalization.
Okubo et al. (Reference Okubo, Osuka, Jung, Figueroa, Tsujimoto and Aiba2014) compared two exercise groups, one of a walking and one of a balance training. They found small but significant changes in lower extremity strength and dynamic balance levels in both groups; however, walking alone managed to increase the number of daily steps and the fall self-efficacy score (Okubo et al., Reference Okubo, Osuka, Jung, Figueroa, Tsujimoto and Aiba2014). The majority of the studies related with small effect sizes in community-dwelling settings (Crocker et al., Reference Crocker, Young, Forster, Brown, Ozer and Greenwood2013). Similarly, our study showed small to medium effect size changes in physical function components.
There are a few randomized controlled trials that have shown that exercise can improve mobility, but it can be unsuccessful in reducing falls (Cameron et al., Reference Cameron, Dyer, Panagoda, Murray, Hill and Cumming2018; Gardner, Robertson, & Campbell, Reference Gardner, Robertson and Campbell2000). Moreover, some recent systematic reviews in the nursing home setting have not provided strong evidence of the benefits of exercise on the older residents’ physical performance or falls outcomes. Nevertheless, physical and functional gains of exercise are not to be doubted, but it is suggested that further research is needed to take the next step in order to determine whether a multidimensional exercise program actually does reduce risk of falls.
Limitations of the Study
Among the limitations of this study are the (a) small duration of the study, which was completed in eight weeks; (b) possibility of research bias, since the investigators had a role in the study design; (c) data collection and analysis; and (d) small sample size. Despite the initial sample randomization, substantial baseline differences in the groups were recorded, negatively affecting the homogeneity of the sample. Additionally, by setting the presence of cognitive impairment as an exclusion sample criteria, a significant number of home care residents, also at a high risk of falls, were left out. Furthermore, it needs to be determined whether the positive outcomes observed on physical performance measures, as a result of exercise implementation, can translate to a reduction of falls in the older residents. Additionally, the fact that the control group did not receive any exercise intervention may have affected the results of the study. Lastly, the population was exclusively nursing home residents, and their results cannot be generalized to other settings.
Conclusion
Despite the beneficial effects of an exercise program on the older population’s strength and flexibility status demonstrated in this study, further evidence is needed in a larger sample, by using stratified normative outcomes for age and gender, so as to make safe conclusions. Additional studies are also needed to examine the long-term benefits of this exercise intervention program and to identify the time-dependent effects of a longitudinal exercise program on fall risk factor reduction. In addition to the assessment of the upper and lower extremities’ strength and flexibility, a comprehensive assessment of the trunk function, including the lumbar extensor muscles, should be incorporated in future studies (Vlažná et al., Reference Vlažná, Krkoška, Kuhn, Dosbaba, Batalik and Vlčková2021). Within the exercise group, the study should resume comparing the reduction of risks between the older adults who actually had previous falls and those who had not. Furthermore, the role of Information and Communication Technologies (ICT) through telephone communication, telemonitoring, and tele-exercise programs, in a home fall prevention program, could be beneficial in improving patients’ compliance, as well as adopting a more personally prescribed exercise prevention program based on each patient’s risk profile (Bernocchi et al., Reference Bernocchi, Giordano, Pintavalle, Galli, Ballini Spoglia and Baratti2019; Giordano et al., Reference Giordano, Bonometti, Vanoglio, Paneroni, Bernocchi and Comini2016). Especially nowadays, with the current COVID-19 pandemic affecting the entire world, the use and integration of mobile technologies as fall prevention strategies are highly recommended for future research. Lastly, the safe implementation of fall prevention exercise programs in older residents with dementia should be considered and examined in future research.
The findings of the present thesis are important with regard to clinical practice in physiotherapy. Small but significant improvements were demonstrated in strength and flexibility among nursing home residents following a low intensity and short-duration multidimensional group exercise training program. The program described in this study has been proven to be efficient, easy to be implemented, and inexpensive, as it requires only simple equipment and thus it appears to be an ideal choice for the training of older people in nursing homes on clinical physiotherapy practice. It would be of value to extend the exercise program to a long-term investigation with follow-up, before trying to generalize the findings.
Acknowledgements
The study is part of a bigger study, where the same sample and intervention were used in a previous published study on July 2021: Pepera, G., Krinta, K., Mpea, C., Peristeropoulos, A., & Antoniou, V. (Reference Pepera, Mpea, Krinta, Peristeropoulos and Antoniou2021). Effects of multicomponent exercise training intervention on hemodynamic and physical function in older residents of long-term care facilities: a multicenter randomized clinical controlled trial. Journal of Bodywork and Movement Therapies, 28, 231–237. https://doi.org/10.1016/j.jbmt.2021.07.009. It was presented at the World Confederation for Physical Therapy (WCPT) Congress (2021) (e-poster).
Funding
None declared.










