No CrossRef data available.
Article contents
Diagnostic stability of 346 patients with borderline personality disorder based on retrospective clinical records
Published online by Cambridge University Press: 19 July 2023
Abstract
State-of-the-art research highlights that borderline personality disorder have high rates of comorbid Axis I disorders, which imply uncertainty in establishing an accurate diagnosis and can be some of the most challenging patients for clinicians and researchers.
This study seeks to observe the diagnostic stability in borderline personality disorder patients, in order to increase empirical knowledge through a retrospective look at the historical line of diagnoses.
A twenty-year retrospective study at a psychiatric hospital, searching at the electronic clinical records for all patients with borderline personality disorder diagnosis, under the code 301.83 from World Health Organization’s International Classification of Diseases, 9th Revision (WHO ICD9). A 346 patients’ sample was identified aged between 18 and 83 years (Mage=44.14 years, SD=11.18; predominantly female 73.70%; Mschooling=9.31years; Madmissions=4.72times, SD=9.21; 2nd-5th comorbid diagnosis, a 75.72% sample with three diagnosis); excluding organic cerebral syndrome and no comorbidity besides drug abuse, or no comorbidity at all.
As a general observation, the following diagnoses are indicated: 44.09% major depressive disorder, 33.16% affective disorder, 13.05% schizophrenia, and 9.70% mania. As a spectrums disorders analysis (Figure 1), differential percentage occurrences are identified in patients with borderline personality disorder.
Image:
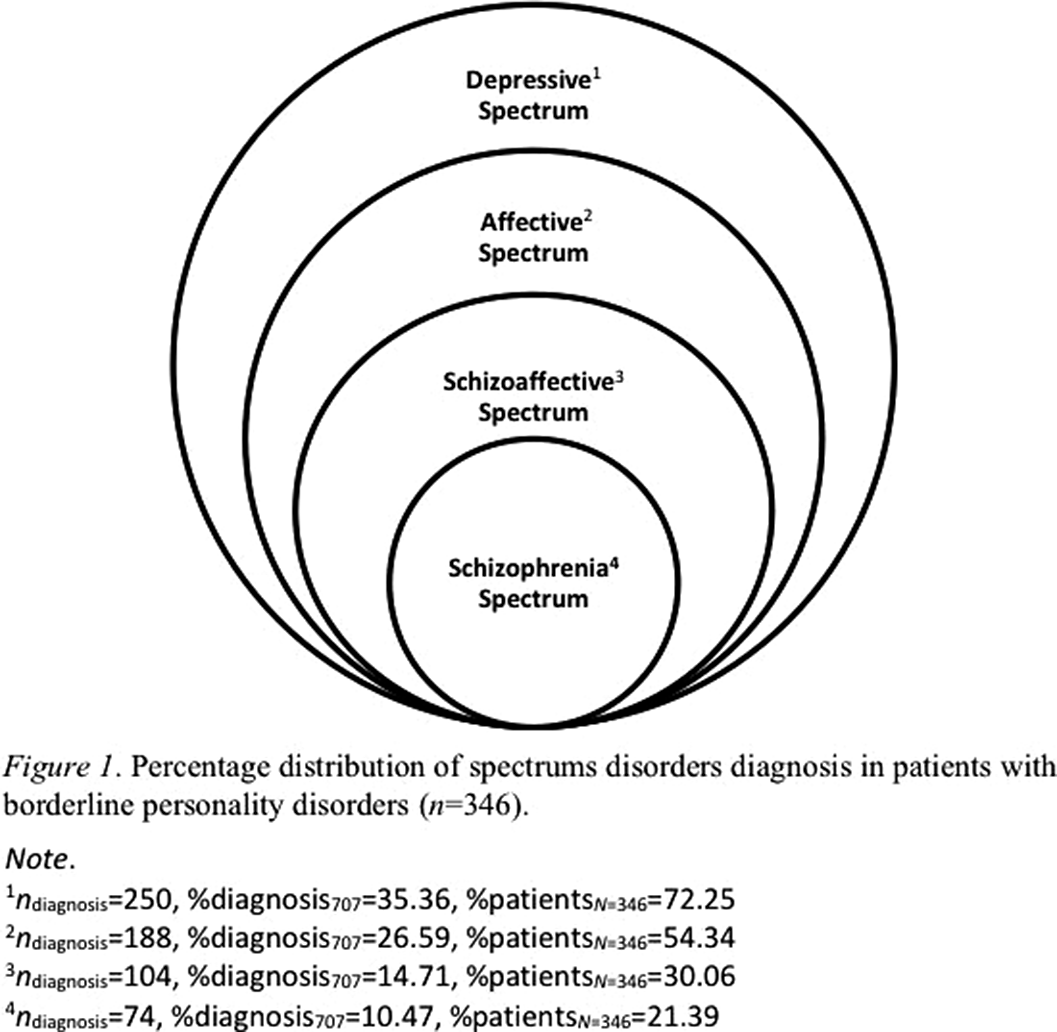
Based on clinical diagnoses records of borderline personality disorder patients, some spectrums disorders are highlighted, to be reported in descending order of incidence: depressive, affective, schizoaffective and schizophrenia spectrums.
None Declared
- Type
- Abstract
- Information
- European Psychiatry , Volume 66 , Special Issue S1: Abstracts of the 31st European Congress of Psychiatry , March 2023 , pp. S625 - S626
- Creative Commons
- This is an Open Access article, distributed under the terms of the Creative Commons Attribution licence (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted re-use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Copyright
- © The Author(s), 2023. Published by Cambridge University Press on behalf of the European Psychiatric Association





Comments
No Comments have been published for this article.