No CrossRef data available.
Article contents
Drug attitude inventory is relevant to LAI treatment persistence in schizophrenia: Preliminary results
Published online by Cambridge University Press: 13 August 2021
Abstract
Patients’ attitudes and subjective experience are crucial in the management of severe mental illness, but their practical value is overlooked.
To identify predictors of future adherence to LAI antipsychotic maintenance treatment of schizophrenia among socio-demographic, clinical, and psychometric characteristics – including Drug Attitude Inventory-10 (DAI-10) and Subjective Well-being under Neuroleptics short form (SWN-K) scores.
Retrospective baseline data from 53 clinically stable outpatients with schizophrenia switched from oral to LAI therapy were collected. Patients continuing treatment at the time of analysis (n=29) were compared to those who had discontinued it (n=24). Selected variables were further evaluated in survival analyses.
Between-group differences are presented in Table 1 (**: p<0.01; *: p<0.05).
| Continued treatment | Discontinued treatment | χ2 or t | |
| Treatment persistence (months) | 63.79±21.01 | 23.88±25.80 | 6.21** |
| Age (years) | 39.17±10.11 | 35.58±13.39 | 1.11 |
| Male | 15 (51.7%) | 13 (54.1%) | 0.03 |
| Single | 20 (69.0%) | 15 (62.5%) | 0.25 |
| Instruction (years) | 13.28±3.31 | 11.83±3.56 | 1.53 |
| Employed | 20 (69.0%) | 7 (29.2%) | 8.32** |
| Illness duration (years) | 17.69±10.53 | 13.42±11.36 | 1.42 |
| Previous hospitalisations | 2.10±1.32 | 2.67±1.86 | -1.29 |
| MADRS | 13.59±9.06 | 14.67±8.99 | -0.43 |
| YMRS | 5.52±5.57 | 6.00±9.94 | -0.22 |
| p-PANSS | 12.17±5.20 | 14.38±6.13 | -1.41 |
| n-PANSS | 10.90±5.39 | 15.63±7.93 | -2.48* |
| g-PANSS | 29.38±10.33 | 33.63±10.26 | -1.49 |
| PANSS | 52.66±17.57 | 63.96±20.61 | -2.15* |
| DAI-10 | 3.86±4.96 | -1.13±5.80 | 3.38** |
| SWN-K | 74.93±23.07 | 81.00±15.60 | -1.09 |
Cox regression analysis included instruction, employment, hospitalisations, PANSS subscales and DAI-10 scores: a protective role against treatment discontinuation was outlined only for employment (HR 0.16; 95%CI 0.05-0.50) and higher DAI-10 scores (HR 0.85; 95%CI 0.78-0.94). DAI-10 scores delineated distinct adherence trajectories (Figure 1).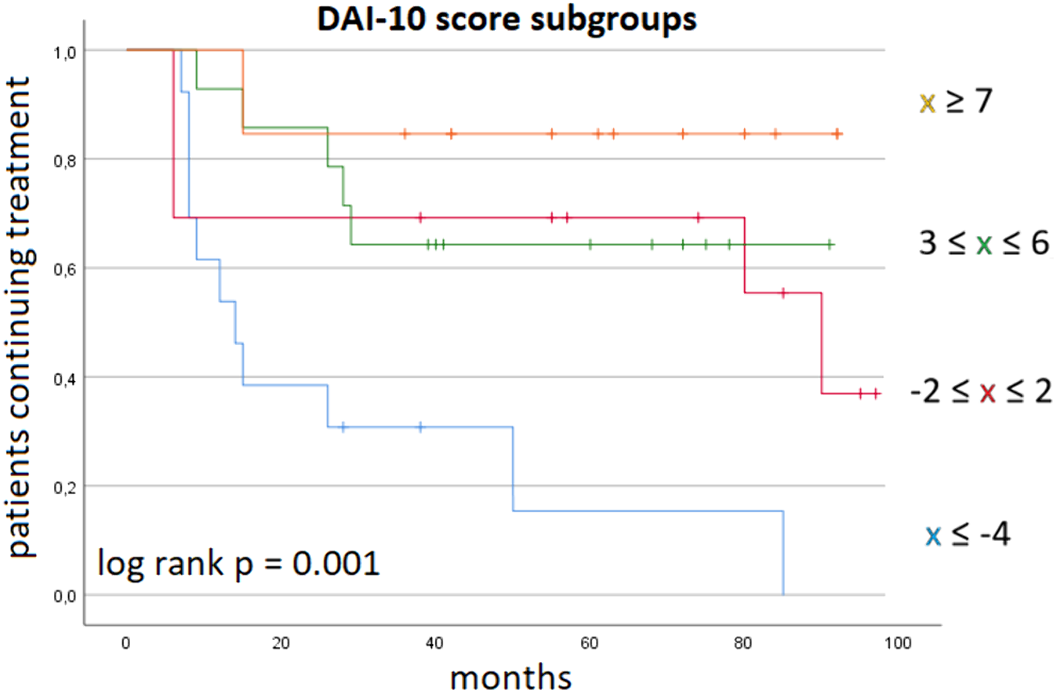
Baseline DAI-10 scores may identify patients at risk of dropout after switching to LAI.
No significant relationships.
- Type
- Abstract
- Information
- European Psychiatry , Volume 64 , Special Issue S1: Abstracts of the 29th European Congress of Psychiatry , April 2021 , pp. S156
- Creative Commons
- This is an Open Access article, distributed under the terms of the Creative Commons Attribution licence (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted re-use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Copyright
- © The Author(s), 2021. Published by Cambridge University Press on behalf of the European Psychiatric Association





Comments
No Comments have been published for this article.