Healthcare-associated infections (HAIs) are common inpatient adverse events and result in significant morbidity, mortality, and cost. Reference Klevens, Edwards and Richards1,Reference Scott2 From 2011 to 2014, hospitals reported 85,994 central-line–associated bloodstream infections (CLABSIs), 138,283 catheter-associated urinary tract infections (CAUTIs), and 133,080 surgical site infections (SSIs). Reference Weiner, Webb and Limbago3 Costs attributable to HAI vary widely. Reference Scott2,Reference Olsen, Tian and Wallace4–Reference Al-Rawajfah, Hewitt, Stetzer and Cheema7 Adult inpatient CLABSIs have been associated with attributable costs of $7,288 per infection; CAUTIs have been associated with attributable costs of $862 to $1,007; and SSIs have been associated with attributable costs of $11,874 to $34,670 (2007 USD). Reference Scott2 Attributable CLABSI costs in adult intensive care units range between $21,400 and $110,800; CAUTI costs range between $1,200 and $4,700; and SSI costs range between $5,600 and $12,900 (2009 USD). Reference Umscheid, Mitchell, Doshi, Agarwal, Williams and Brennan5
Pediatric HAI costs are less well studied. Pediatric inpatient CLABSIs have been associated with mean attributable costs from $55,646 (2011 USD) to $69,332. Reference Wilson, Rafferty, Deeter, Comito and Hollenbeak6,Reference Goudie, Dynan, Brady and Rettiganti8 Pediatric inpatient CAUTIs have been associated with a mean attributable cost of $7,200 (2011 USD). Reference Goudie, Dynan, Brady, Fieldston, Brilli and Walsh9 To our knowledge, no studies have investigated costs associated with inpatient pediatric SSI. Few studies have examined costs associated with pediatric HAI in ambulatory settings, despite many pediatric patients requiring long-term, ambulatory central lines, ambulatory urinary catheterization or outpatient surgery, and suggestions of high ambulatory pediatric HAI incidence. Reference Zingg, Fu and Neves10–Reference Audry, Johanet, Achrafi, Lupold and Gruner20 A single-center study of ambulatory bloodstream infections (BSIs) and CLABSIs in pediatric oncology patients identified attributable charges (not costs) of $36,611. Reference Wong Quiles, Gottsch, Thakrar, Fraile and Billett21 In pediatric and adult patients with SSIs following hernia repair and anterior cruciate ligament reconstruction, 2 surgeries commonly performed as ambulatory, costs ranged from $3,028 to $16,489 and from $3,735 to $19,356 (2014 USD), respectively. Reference Olsen, Tian and Wallace4
The healthcare costs of pediatric ambulatory HAIs across all at-risk populations is unclear. Given the potential harm to children and the lack of data on attributable costs, this study establishes attributable costs for ambulatory pediatric CLABSIs, and CAUTIs, and SSIs following ambulatory surgery in 4 academic centers via retrospective, matched case-control analyses.
Methods
Setting
This retrospective epidemiologic analysis was performed in 4 urban, pediatric, tertiary-care academic medical centers. Data for ambulatory CLABSIs and CAUTIs were obtained from all 4 sites, and data for SSI following ambulatory surgery were obtained from 2 sites due to resource availability. These institutions were brought together as part of the New York City Clinical Data Research Network (NYC-CDRN). Reference Kaushal, Hripcsak and Ascheim22 The NYC-CDRN created the electronic queries described below, although all queries were run at individual sites on site-specific databases. All pediatric patients <22 years old who had ambulatory visits at 1 of these sites from October 1, 2010, through September 30, 2015, were eligible for inclusion.
Ambulatory healthcare-associated infection and control patient identification
To obtain maximal event capture, patients who may have been at risk for ambulatory HAI were identified with 3 increasingly broad electronic medical record queries. The first queries included patients with billing codes for CLABSIs and CAUTIs; the second queries identified patients with positive blood and urine culture respectively, and a concomitant International Statistical Classification of Diseases and Related Health Problems, 9 th edition (ICD-9) code for a diagnosis commonly found in patients who use central lines or urinary catheters (eg, oncology ICD-9 codes for patients with positive blood cultures or urologic ICD-9 codes for patients with positive urine cultures). The third included patients with billing codes for central line and urinary catheter insertion, removal, or use, respectively. The first SSI following ambulatory surgery query identified patients with billing codes for SSI; The second query identified patients with >1 clinic visit or any admission, reoperation, emergency department visit, complete blood count ordered, wound culture ordered, or antibiotic prescription from the day following their initial ambulatory surgery through 30-days following surgery. The third query included all patients with an ambulatory surgery billing code. Complete query parameters are provided in the Appendix (online).
All patients identified by any of the 3 CLABSI or CAUTI queries received manual chart reviews to screen for central lines or urinary catheters and to identify ambulatory HAI (HAI definitions provided below). All patients identified by the first SSI following ambulatory surgery query received manual chart review to confirm ambulatory surgery and identify ambulatory HAI. Due to the large number of patients identified by the 2 broader SSI following ambulatory surgery queries, a random sample of approximately 20% of patients from each query received manual chart review to investigate for SSI following ambulatory surgery. Only 2 SSIs following ambulatory surgery were identified from the second query and none from the third. Trained abstractors entered data into a REDCap database. Reference Harris, Taylor, Thielke, Payne, Gonzalez and Conde23
Once all potential HAIs were adjudicated (see definitions below), the first HAI in the study window for a unique patient was matched up to 1:3 with controls—patients who were at risk for, but did not experience, an HAI. Matching for CLABSI and CAUTI was conducted according to (1) the patient’s primary urinary catheter–related or central-line–related diagnosis ICD-9 diagnostic code group, (2) study site, and (3) presence of a central line or urinary catheter coincident with the case’s CLABSI or CAUTI. Chart abstractors identified a patient’s primary diagnosis that led the patient to need a urinary catheter or central line, and this primary diagnosis was grouped into 1 of 17 top-level ICD-9 diagnostic code groups. 24 Matching for SSI following ambulatory surgery was conducted according to (1) primary surgery organ system, (2) study site, and (3) surgery coincident in time ±60 days with the case’s SSI. This matching scheme accounted for changes in prevention strategies throughout the study period but allowed for broad assessment of potential risk factors in other related research studies on this database. Notably, no control patients were identified that met all 3 matching criteria at 1 site.
Definitions
The 2015 National Healthcare Safety Network (NHSN) definitions for CLABSI, CAUTI, and SSI were used to identify HAI. 25 HAIs were deemed to be ambulatory if the positive blood or urine culture was obtained >48 hours after hospital discharge or ≤48 hours after inpatient admission. In addition, patients performing clean intermittent catheterization (CIC) were included as at risk for CAUTI; CIC patients are at risk for similar infections and have never been included in the NHSN definition despite large numbers of children using CIC in the ambulatory space. Reference Larijani, Moghtaderi, Hajizadeh and Assadi26–Reference Jewes, Gillespie and Leadbetter29
Patients were considered for SSI following ambulatory surgery if they were not admitted to the hospital or not in a hospital bed at midnight on the day of their surgery. The operative procedure definition included any procedure that took place during an operation where at least one incision (including laparoscopic approach) was made through the skin or mucous membrane and in an operating room. 30 These modifications allowed us to study SSI following ambulatory surgery risk among patients undergoing procedures that are not included in the NSHN’s list of inpatient operative procedures. Reference Rinke, Jan, Nassim, Choi and Choi16
Data abstractors were trained to adjudicate HAI by a pediatric hospital epidemiologist on the research team (L.S.), and they frequently shared adjudication questions for discussion and review.
Cost determination
Charges were obtained from site-specific databases 30 days before, on the day of, and 30 days after the HAI for CLABSI and CAUTI cases and controls, and SSI following ambulatory surgery cases. For SSI following ambulatory surgery controls, the number of days between the matched SSI case’s surgery and their SSI following ambulatory surgery was calculated. SSI control charges were then obtained 30 days before, on the day of, and 30 days after that number of days after the control’s surgery date. This allowed for charge windows to be consistent relative to each patient’s individual surgery date. Two sites provided line-item professional and facility charges: 1 provided just facility charge and 1 provided inpatient charges from a connected database. Because cases and controls for all HAIs were matched based on site, this heterogeneity is consistent within specific case–control matched groups.
Charges were converted to costs using the group all-payer inpatient cost-to-charge ratio for urban, nonprofit hospitals with >300 beds, which we obtained from standard cost-to-charge ratio files. 31 Costs were then adjusted to 2015 USD using Bureau of Economic Analysis Personal Consumption Expenditure health component price index (PCE-Health). 32 PCE-Health was chosen because it reflects payments by all payers for medical services, whereas the medical component of the consumer price index (MCPI) excludes expenditures by third-party payers. Reference Dunn, Grosse and Zuvekas33
Statistical analyses
Descriptive statistics were used to analyze differences in costs, comparing the 30 days prior to the infection date and the infection date plus the 30 days following HAI. The primary outcome was additional costs associated with each specific ambulatory HAI. Additional costs for each HAI were estimated using a difference-in-difference analysis with a Wald t test using mixed effects linear regression accounting for matching of cases and controls. The analysis compared the difference in cases’ and controls’ respective differences in costs accrued on the infection date and in the 30 days following the infection date (post-HAI) with cost accrued in the 30 days prior to the infection date (pre-HAI). In the primary model, patients with unrecorded charge data (ie, no charges recorded) were excluded from the analysis. A sensitivity analysis assumed that patients with unrecorded charge data have charges of $0. Statistical analyses were completed using SAS version 9.4 software (SAS Institute, Cary, NC).
This study was approved by the Biomedical Research Alliance of New York (BRANY) institutional review board.
Results
Ambulatory CLABSIs
After manual chart review, 177 unique pediatric patients with an ambulatory CLABSI in the study window were able to be matched with 382 at-risk controls with ambulatory central lines. Overall, 81% of cases were matched with at least 1 control patient. Queries of charge databases yielded charges for 165 cases (93%) and 317 controls (83%).
When patients with unrecorded charge data were excluded from the analysis, the mean difference in costs for ambulatory CLABSI cases comparing before and after CLABSI was $4,336 (95% CI, $529–$8,142). Among control patients, the mean difference in costs comparing before and after the respective case’s CLABSI date was −$1,348 (95% CI, −$4,085–$1,390). Additional costs associated with ambulatory CLABSI via the difference in differences analysis was $5,684, (95% CI, $1,005–$10,362; P < .0174). When patients with unrecorded charge data were assumed to have charges of $0, additional CLABSI costs was $6,502 (95% CI, $2,261–$10,744; P = .0027) (Tables 1 and 2).
Table 1. Costs of Ambulatory Pediatric Healthcare-Associated Infections: Difference-in-Differences Analysis in 2015 US Dollarsa

Note. IQR, interquartile range; CI, confidence interval; CLABSI, central-line–associated bloodstream infection; CAUTI, catheter-associated urinary tract infection; SSI, surgical site infection.
a Unrecorded charges excluded.
Table 2. Costs of Ambulatory Pediatric Healthcare Associated Infections: Difference-in-Differences Analysis in 2015 US Dollarsa
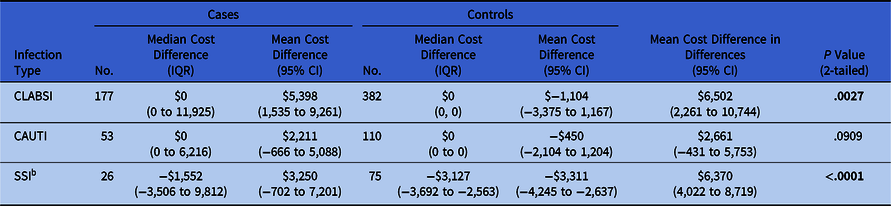
Note. IQR, interquartile range; CI, confidence interval; CLABSI, central-line–associated bloodstream infection; CAUTI, catheter-associated urinary tract infection; SSI, surgical site infection.
a Unrecorded charges treated as $0.
b Analysis is identical to Table 1 because all cases and controls had at least 1 charge.
Ambulatory CAUTIs
After manual chart review, 53 unique patients with a CAUTI in the study window were able to be matched with a total of 110 at-risk controls with ambulatory indwelling urinary catheters or performing CICs. Overall, 85% of cases were matched with at least 1 control patient. Queries of charge databases yielded charges for 30 cases (57%) and 43 controls (39%).
When patients with unrecorded charge data were excluded from the analysis, the mean difference in costs for ambulatory CAUTI cases comparing before and after CAUTI was $4,146 (95% CI, −$630 to $8,923). Among control patients, the mean difference in costs comparing before and after their respective case’s CAUTI was −$2,454 (95% CI, $−5,718 to $811). Additional costs associated with ambulatory CAUTI via the difference in differences analysis was $6,600 (95% CI, $1,055–$12,145; P = .0208). When patients with unrecorded charge data were assumed to have charges of $0, additional CAUTI cost of $2,661 (95% CI, −$431 to $5,753; P = .0909) (Tables 1 and 2).
SSIs following ambulatory surgery
After manual chart review, 26 unique patients with a SSI following ambulatory surgery in the study window were matched with a total of 75 at-risk controls with ambulatory surgery. Overall, 90% of cases were matched with at least 1 control patient. All patients were from a single site, which provided facility and professional charges. Queries of charge databases yielded charges for all cases and controls.
The mean difference in costs for SSI following ambulatory surgery cases comparing before and after SSI was $3,250 (95% CI, −$702 to $7,201). Among control patients, the mean difference in costs comparing before and after the same number of days following their surgery as the days between their respective case’s surgery and SSI was −$3,311 (95% CI, $−4,245 to $−2,637). Additional costs associated with SSI following ambulatory surgery via difference in differences analysis was $6,370 (95% CI, $4,022–$8,719; P < .0001) (Tables 1 and 2).
Discussion
Using a difference-in-differences analysis, this multicenter study identified additional costs associated with ambulatory pediatric CLABSI of $5,684; costs associated with CAUTI of $6,600; and costs associated with SSI following ambulatory surgery of $6,370. To our knowledge, this is the first study reporting additional costs of pediatric ambulatory CLABSI and CAUTI, and SSI following ambulatory surgery in a multisite cohort, inclusive of all patient diagnoses and surgeries.
In comparison, studies found mean attributable costs of pediatric inpatient CLASBI of $55,646 to $69,332 (2011 USD), Reference Wilson, Rafferty, Deeter, Comito and Hollenbeak6,Reference Goudie, Dynan, Brady and Rettiganti8 and pediatric inpatient CAUTI of $7,200 (2011 USD). Reference Goudie, Dynan, Brady, Fieldston, Brilli and Walsh9 Adult SSIs have been associated with attributable costs of $11,874 to $34,670 (2007 USD), Reference Scott2 and SSIs following hernia repair and anterior cruciate ligament reconstruction, which are commonly performed ambulatory, ranged from $3,028 to $16,489 and from $3,735 to $19,356 (2014 USD) respectively. Reference Olsen, Tian and Wallace4 These costs have large variability based on type of surgery.
Overall lower additional costs were associated with pediatric ambulatory HAIs than inpatient HAIs. Reference Wilson, Rafferty, Deeter, Comito and Hollenbeak6,Reference Goudie, Dynan, Brady and Rettiganti8,Reference Goudie, Dynan, Brady, Fieldston, Brilli and Walsh9 Multiple factors may account for this discrepancy. Patients in this study may have had lower disease severity or higher baseline health status than inpatients, suggesting milder disease courses or shorter inpatient stays, which reduce associated HAI cost. Alternatively, lower additional costs may be influenced by differing methodologies; we used a measure of healthcare cost inflation, the PCE-Health, that has not grown as rapidly as the MCPI Reference Dunn, Grosse and Zuvekas33 used in some inpatient HAI studies. Additionally, some sites were unable to provide complete charge data, which may contribute to an underestimation of associated costs.
Pediatric ambulatory HAI were nonetheless associated with significant costs. Ambulatory HAIs likely occur in greater absolute numbers than inpatient HAIs, Reference Rinke, Milstone and Chen17 creating an appreciable cumulative cost. As expected, ambulatory CLABSI costs identified here were lower than identified charges from a single-center study of pediatric hematology-oncology ambulatory BSIs and CLABSIs. That study identified crude charges of $36,611 per infection in patients whose admission was “solely related to their bloodstream infection.” Reference Wong Quiles, Gottsch, Thakrar, Fraile and Billett21 If these charges are roughly converted to costs by a multiple of 0.35 (mean cost-to-charge ratio from 2010 to 2015 31 ), the result is $12,814, closer to the $10,744 upper limit in this study. Differences may also suggest that cost calculations may not be broadly applicable across all patient populations and that diagnosis of specific HAI costing may be needed to understand ambulatory HAI costs.
In addition to using hospital-based charges, some studies on the attributable cost of HAI use a micro-costing approach. Reference Stevens, Geiger, Concannon, Nelson, Brown and Dumyati34,Reference Graves, Weinhold and Tong35 These studies assign a unit cost for every resource used in the treatment of a patient Reference Xu, Grossetta Nardini and Ruger36 then identify which costs are attributable to the HAI. This methodology is important for patients with extensive healthcare interactions coincident with their HAI. This study was unable to employ micro-costing given limitations in site data and the time required to attribute a given resource to an ambulatory HAI. We believe that using a difference-in-difference analysis to compare costs before and after an HAI takes into account the background cost of care and removes the non-HAI costs from our estimation. It also accounts for potential differences in the severity of illness for cases and controls.
Importantly, the additional costs of ambulatory HAIs presented in this study ignores the financial burden placed on the families of children with these infections. Each HAI generates additional health insurance copayments, travel costs, and lost work time. HAIs further compound existing financial strain for caregivers of patients with complex chronic conditions who already experience reduced employment and lost wages due to the long-term needs of providing care for children with chronic conditions. Reference Kish, Newcombe and Haslam37 Previous research found that reducing avoidable healthcare encounters in children with medical complexity covered by Medicaid leads to significant cost savings. Reference Berry, Hall and Neff38 The all-inclusive costs of ambulatory HAI are likely appreciably higher than those calculated here.
This study has several limitations. First, we were unable to capture complete charge information for all patients in our study, which may have artificially lowered our ultimate cost estimates. Some patients had no charge data on their patient account, and we are unable to determine whether these unrecorded values reflected no charges accrued, charges not in the databases we had access to for this study, or charges accrued outside of the primary health system. This gap biases our results toward underestimating the true costs of ambulatory HAI. CLABSI and CAUTI cost data were obtained from 4 urban, tertiary-care, academic medical centers, and information on cost of SSI following ambulatory surgery was obtained from only 1 site. Thus, our results, particularly regarding the cost of SSI, may not be generalizable to all pediatric patients, especially in rural and non–tertiary-care centers. However, we believe that many children at risk for ambulatory CLABSI and CAUTI are treated in tertiary-care centers. Matching was performed with broad categories, which may have created unbalanced groups, suggesting the need for further research with even more specific matching criteria on larger cohorts of patients. In addition, matching based on catheter or central-line type or specific surgery may be a key variable in future cost analyses. The lack of significance in the sensitivity analysis CAUTI model was likely related to the addition of >20 cases and 60 controls with zero costs, biasing the model toward the null hypothesis. Increased nonrecorded CAUTI charges may result from decreased healthcare utilization in patients with CAUTI compared to CLABSI. Data from another study on this cohort suggest that fewer than half of patients with ambulatory CAUTI were hospitalized, whereas 85% of patients with ambulatory CLABSI were hospitalized. Reference Rinke, Oyeku and Heo39,Reference Rinke, Heo and Saiman40 Finally, cost-to-charge ratios, while commonly used in HAI research, Reference Goudie, Dynan, Brady and Rettiganti8,Reference Goudie, Dynan, Brady, Fieldston, Brilli and Walsh9,Reference Graves, Weinhold and Tong35 may misestimate costs for a given institution, and the group all-payer inpatient cost-to-charge ratio for urban, nonprofit hospitals with >300 beds may not apply to all pediatric charges found in our patients, especially ambulatory visits.
Pediatric ambulatory CLABSIs and CAUTIs and SSIs following ambulatory surgery are associated with significant healthcare costs. This article adds to the growing body of literature on the cost of HAIs among pediatric patients. Additional research should be conducted to expand the generalizability of our findings across regions and to include patient and family costs. Future infection prevention initiatives should strive to reduce HAIs among at-risk ambulatory pediatric patients.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/ice.2020.305
Acknowledgments
The authors gratefully acknowledge the contributions of Ms Kelly Ann Balem, RN.
Financial support
The authors were supported by the Agency for Healthcare Research and Quality (grant no. R01HS24432).
Conflicts of interest
No authors report a potential conflict of interest related to this article.





