The term ‘plant-based diets’ has been used for more than 20 years, with discussion of potential benefits and risks(Reference Mann1). There is no universally agreed definition of the term, and although some have used it to refer to omnivorous diets with a low content of animal source foods (e.g. meat and fish), the threshold for this has not been agreed and here we take the pragmatic approach of using it to refer to vegetarian (lacto-ovo-vegetarian: plant-based except for dairy products and or eggs) and vegan diets (100 % plant-based).
Evidence on the health-status of vegetarians and vegans comes from a substantial number of relatively small cross-sectional studies which compare their dietary intakes, nutritional status and physiological characteristics with those of meat-eaters, together with a small number of prospective cohort studies which follow the health of these groups over many years. This review is based largely on results from EPIC-Oxford (the European Prospective Investigation into Cancer and Nutrition Oxford cohort), with some results from the earlier Oxford Vegetarian Study and from the UK Biobank(Reference Davey, Spencer and Appleby2–Reference Allen, Sudlow and Peakman4). EPIC-Oxford is a cohort of 65 000 men and women living throughout the UK and was established in the 1990s with recruitment targeted to identify as many vegetarians as possible, and 50 % of the participants do not eat meat; some analyses of EPIC-Oxford, on cancer and mortality, also include data from the Oxford Vegetarian Study which used similar methods of recruitment and follow-up of 11 000 people recruited in the early 1980s. UK Biobank is a cohort of 500 000 men and women in the UK established between 2006 and 2010; recruitment was not targeted at vegetarians, but due to the large size of the cohort it includes several thousand vegetarians and several hundred vegans. In this review, we describe the relationships of plant-based diets with nutritional intakes, physiological and biochemical characteristics, and long-term health.
Food intakes
Vegetarian and vegan diets are defined by the foods that are excluded, but examination of the composition of such diets shows typical patterns by which they differ from omnivorous diets. In EPIC-Oxford, vegetarians and vegans have much higher intakes compared to regular meat-eaters of soya, legumes, nuts and other moderately high-protein plant foods, substantially higher intakes of relatively unprocessed cereals, and modestly higher intakes of fruit and vegetables(Reference Papier, Tong and Appleby5); this pattern is consistent with the expectation that the energy and other nutrients supplied in omnivorous diets by meat, fish and dairy products will be largely replaced by the types of plant foods which contain substantial amounts of energy and protein, rather than by plant foods such as fruit and vegetables which are generally low in energy and protein. A similar pattern was seen in UK Biobank(Reference Bradbury, Tong and Key6).
Nutrients
As a consequence of the foods consumed, vegetarian and vegan diets typically have a different pattern of nutrient intake from omnivorous diets, with relatively high intakes of carbohydrates, n-6 fatty acids, dietary fibre, carotenoids, folate, vitamin C, vitamin E and magnesium, and relatively low intakes of protein, saturated fat, long-chain n-3 fatty acids, retinol, vitamin B12 and zinc; vegans may have particularly low intakes of vitamin B12, calcium and iodine, and plant-based diets are generally devoid of haem iron. For most of these nutrients, the relevance of these differences in terms of long-term health is not yet clear; here, we focus mainly on intakes of protein, saturated fat, dietary fibre, vitamin B12 and calcium.
Dietary intakes in EPIC-Oxford have been assessed at baseline and, in approximately half the cohort, at re-survey about 14 years later(Reference Davey, Spencer and Appleby2,Reference Sobiecki, Appleby and Bradbury7) . At re-survey, mean protein intakes as percent energy were 17⋅2, 15⋅5, 14⋅0 and 13⋅1 % in meat-eaters, fish-eaters, vegetarians and vegans, respectively; the proportions of participants estimated to have inadequate protein intakes were less than 5 % in meat-eaters and fish-eaters, but were 9⋅8 and 6⋅0 % respectively in male and female vegetarians, and 16⋅5 and 8⋅1 % respectively in male and female vegans. These findings should be interpreted cautiously, for example because the dietary questionnaires may not have included some protein-rich foods consumed by vegetarians and vegans (e.g. vegan cheese), but they raise the possibility that protein intake might be inadequate in some of the vegetarians and vegans in this population. Plasma concentrations of amino acids have been measured in a subsample of male participants: circulating non-fasting concentrations of the essential amino acids lysine, methionine, leucine, valine and tryptophan were 6–13 % lower in vegans (but not in vegetarians) compared to those in meat-eaters(Reference Schmidt, Rinaldi and Scalbert8).
Saturated fat intake is typically lower in vegetarians, and especially in vegans, compared to that in meat-eaters. This is to be expected because meat is a major source of saturated fat; for example, in the UK's National Diet and Nutrition Survey for years 2014–2016, meat and meat products provided 24 % of saturated fat intake in men and women aged 19–64(9). In EPIC-Oxford, saturated fat intakes at follow-up as percent energy were 10⋅4, 9⋅4, 9⋅5 and 6⋅9 % in meat-eaters, fish-eaters, vegetarians and vegans, respectively(Reference Sobiecki, Appleby and Bradbury7). It is likely that the reason that saturated fat intake in vegetarians in EPIC-Oxford is only modestly lower (about 9 %) compared to that in meat-eaters is because the vegetarians eat about 50 % more cheese compared to meat-eaters, partly as a substitute for meat(Reference Papier, Tong and Appleby5).
Unrefined plant foods are rich in dietary fibre(10). In EPIC-Oxford, fibre intakes at follow-up were 21⋅7, 24⋅9, 25⋅6 and 28⋅9 g/d of non-starch polysaccharides in meat-eaters, fish-eaters, vegetarian and vegans, respectively(Reference Sobiecki, Appleby and Bradbury7); these intakes would probably be about 30 % higher if expressed as g/d of AOAC (Association of Analytical Chemists) fibre(10).
Plants cannot synthesise vitamin B12 and generally contain none (there may be some exceptions such as duckweed due to the presence of bacteria inside the plant tissue(Reference Kaplan, Zelicha and Tsaban11)); therefore, vegans would be expected to have zero intake unless they consume foods fortified with vitamin B12 and/or vitamin B12 supplements. Vegetarians obtain vitamin B12 from dairy products and/or eggs, but on average their intakes are lower than those of meat-eaters. It is difficult to obtain accurate estimates of intakes of vitamin B12 in vegetarians and vegans because of the need for detailed information on the use of fortified foods and supplements, but blood measurements can provide information on status. In a sub-sample of male participants in EPIC-Oxford, mean serum vitamin B12 concentrations were 281, 182 and 122 pmol/l in meat-eaters, vegetarians and vegans, respectively, and 52 % of vegans, 7 % of vegetarians and <1 % of meat-eaters had concentrations below 118 pmol/l indicating deficiency(Reference Gilsing, Crowe and Lloyd-Wright12).
Calcium intakes typically differ little between meat-eaters, fish-eaters and vegetarians, but are substantially lower in vegans; in the UK, milk and milk products supply 34 % of dietary calcium in men and women aged 19–64(9). In EPIC-Oxford, average intakes at follow-up in the four dietary groups were 1083, 1131, 1117 and 848 mg/d, respectively; intakes in vegans at recruitment were substantially lower, 582 and 610 mg/d in women and men, respectively, and the higher intakes in vegans at follow-up may be explained by more questions on the questionnaire, and greater availability in shops, for plant-based dairy replacements with calcium fortification.
For several other micronutrients, nutritional status is best assessed by measuring concentrations in the blood. Such analyses have shown that vegetarians and particularly vegans in EPIC-Oxford have lower plasma concentrations compared to meat-eaters of EPA, DHA and vitamin D(Reference Rosell, Lloyd-Wright and Appleby13,Reference Crowe, Steur and Allen14) . Haematological measures have not been made in EPIC-Oxford, but analyses of data for white British premenopausal women in UK Biobank have shown that Hb concentrations were lower in vegetarians compared to that in regular meat-eaters, with 12⋅7 % of vegetarians compared to 8⋅7 % of regular meat-eaters categorised as anaemic; data were available for only seventy-six vegans, among whom six (7⋅9 %) were anaemic(Reference Tong, Key and Gaitskell15).
Anthropometry and physiology
At recruitment, the mean BMIs of both male and female vegetarians and vegans in EPIC-Oxford were approximately 1 and 2 kg/m2 lower than those of meat-eaters, respectively(Reference Davey, Spencer and Appleby2). During the first 5 years of follow–up, meat-eaters gained approximately 400 g per year; weight gain was similar in vegetarians, whereas weight gain in vegans was significantly less at approximately 300 g per year(Reference Rosell, Appleby and Spencer16). The lower BMI of vegetarians, and especially vegans, compared to that of meat-eaters in this population would be expected to lead to a lower risk of several diseases linked to obesity, but also a higher risk of any disorders linked to underweight.
Plasma concentrations of non-HDL cholesterol by diet group were measured in a large sample of men and women in EPIC-Oxford(Reference Bradbury, Crowe and Appleby17); non-HDL-cholesterol was measured as a surrogate for LDL-cholesterol and in the remainder of the present paper, for convenience, we refer to the differences noted in non-HDL-cholesterol as differences in LDL-cholesterol. In men, mean LDL-cholesterol was 0⋅85 mmol/l lower in vegans compared to meat-eaters, the difference reduced to 0⋅68 mmol/l lower after adjusting for BMI; the differences in women were 0⋅49 and 0⋅40 mmol/l, respectively, and mean concentrations in vegetarians were intermediate. Blood pressure was also found to be lower in vegans than that in meat-eaters, partly due to lower BMI; differences in mean systolic blood pressure between vegans and meat-eaters before and after adjusting for BMI were 4⋅2 and 2⋅6 mmHg, respectively, in men and 2⋅4 and 1⋅8 mmHg, respectively, in women, whereas the differences in blood pressure between vegetarians and meat-eaters were very small(Reference Appleby, Davey and Key18).
Bone density has not been assessed in EPIC-Oxford, but heel bone mineral density has been measured in almost all participants in UK Biobank. In white British women, the heel bone density test t-scores were −0⋅54, −0⋅62 and −0⋅80 in regular meat-eaters, vegetarians and vegans, respectively; these measures were −0⋅55, −0⋅61 and −0⋅77, respectively, after adjusting for body weight(Reference Tong, Key and Sobiecki19). The lower bone density test t-scores in vegans after allowance for body weight may be related to their lower intakes of micronutrients such as calcium and vitamin D, but other factors might be involved perhaps including the differences in protein intake.
Major diseases: CVD and diabetes
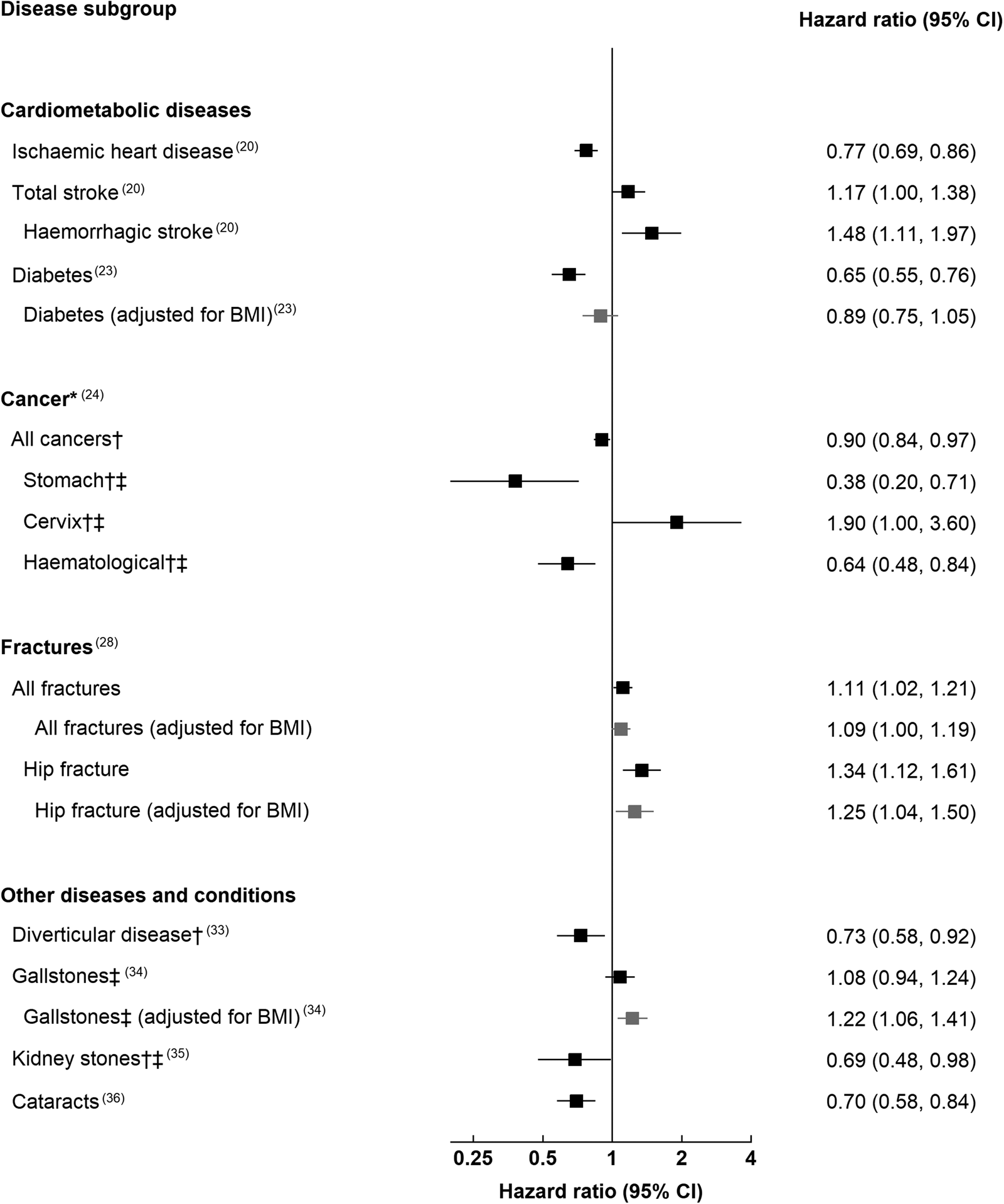
Fig. 1 summarises findings on the associations of vegetarian diets with long-term health in EPIC-Oxford; the results plotted are those for which there was evidence for a difference in risk between meat-eaters and vegetarians (either in the BMI-adjusted or -unadjusted model for outcomes where we showed both models). Fig. 2 shows the equivalent results for which there was evidence for a difference in risk between meat-eaters and vegans. Slight differences in the categorisation of the comparison group in some analyses are given in footnotes to Figs. 1 and 2.
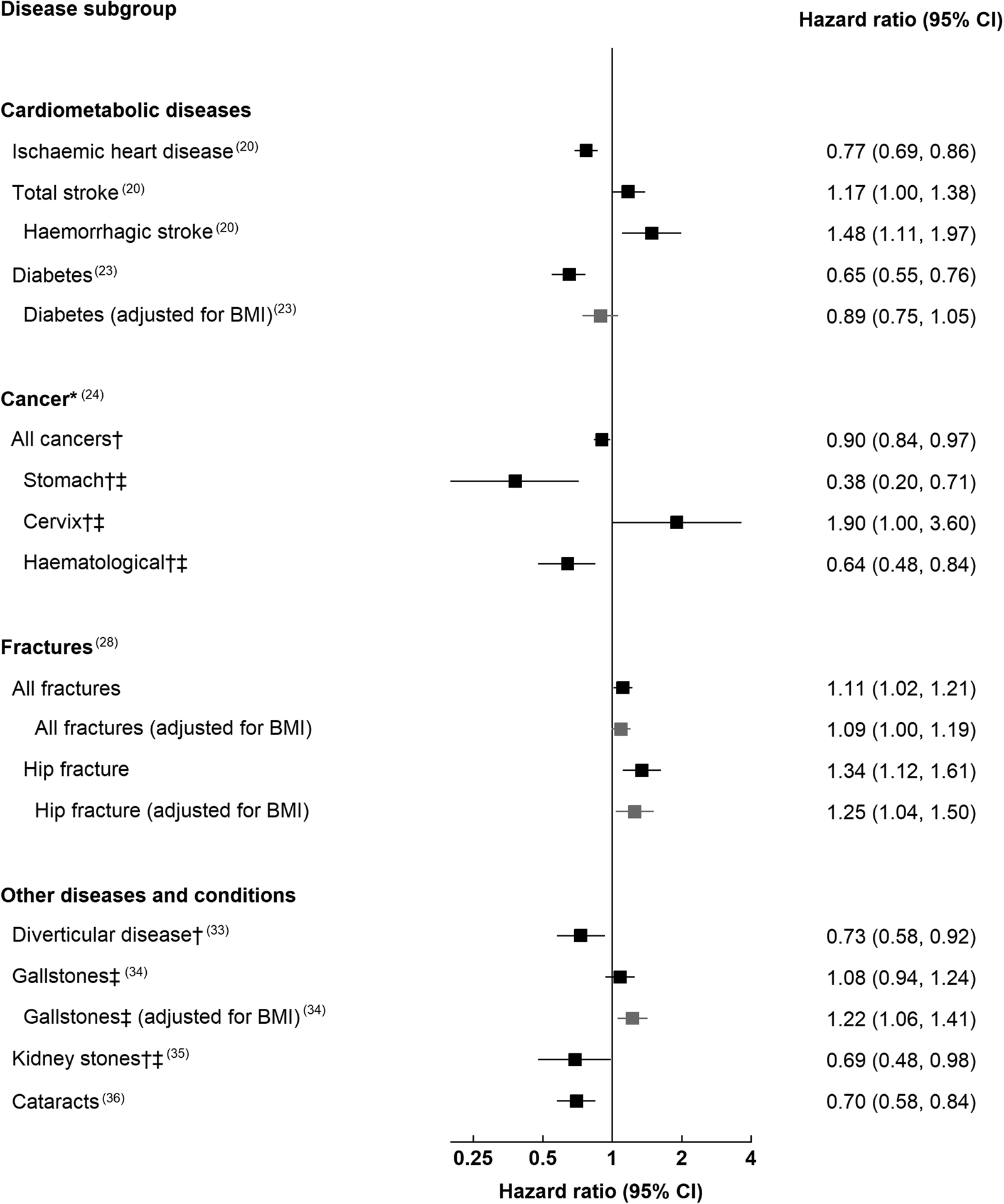
Fig. 1. Risk of various conditions in vegetarians compared with meat-eaters in the EPIC-Oxford study. *Includes data from EPIC-Oxford and the Oxford Vegetarian Study combined. †Adjusted for BMI. ‡Vegetarians and vegans combined. The hazard ratios and 95 % CIs presented are in reference to the following groups: regular meat-eaters who consume 50+ g of meat daily (diabetes); high meat-eaters who consumed 100+ g of meat daily (kidney stones and cataracts); meat-eaters (IHD, total and haemorrhagic stroke, all cancers and subtypes, all fractures and hip fractures, diverticular disease); non-vegetarians who eat meat or fish (gallstones).
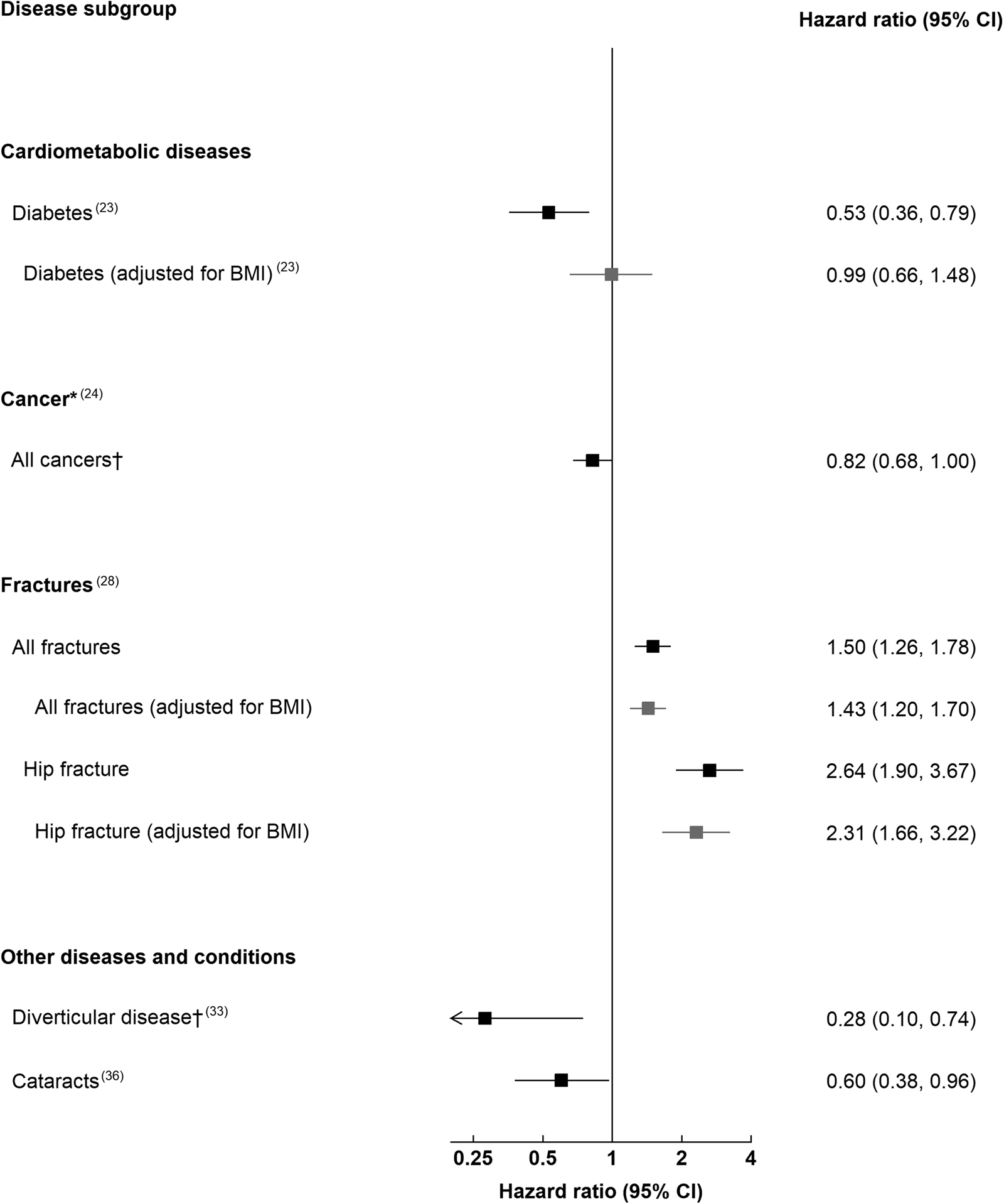
Fig. 2. Risk of various conditions in vegans compared with meat-eaters in the EPIC-Oxford study. *Includes data from EPIC-Oxford and the Oxford Vegetarian Study combined. †Adjusted for BMI. The hazard ratios and 95 % CIs presented are in reference to the following groups: regular meat-eaters who consume 50+ g of meat daily (diabetes); high meat-eaters who consumed 100+ g of meat daily (cataracts); meat-eaters (all cancers, all fractures and hip fractures, diverticular disease).
Compared to meat-eaters, the vegetarians in EPIC-Oxford had a 23 % lower risk of IHD after 18 years of follow-up(Reference Tong, Appleby and Bradbury20). For vegans, the risk estimate was 18 % lower than that in meat-eaters, but due to the relatively small numbers of vegans in the cohort the CI of this estimate were wide and the difference was not statistically significant(Reference Tong, Appleby and Bradbury20). The combined risk of IHD in vegetarians and vegans was 22 % lower than that in meat-eaters, and this was reduced to a 17 % lower risk after adjusting for BMI; data on lipids and blood pressure were not available for the whole cohort, but it is likely that the lower LDL-cholesterol and slightly lower systolic blood pressure of the vegetarians and vegans could explain the remainder of their lower risk.
In contrast to the lower risk of IHD, the risk of stroke was 17 % higher in vegetarians than that in meat-eaters, largely driven by a higher risk of haemorrhagic stroke, which was 48 % higher; the risk for total stroke was not attenuated by adjustment for BMI. The point estimate for haemorrhagic stroke in vegans compared to meat-eaters was 1⋅35, but this was not statistically significant. The cause of the higher risk of haemorrhagic stroke in vegetarians is not known, but it might be explained by the low LDL-cholesterol which has been associated with an increased risk in observational studies, Mendelian randomisation analyses and in lipid lowering trials using statins(Reference Sun, Clarke and Bennett21,Reference Falcone, Kirsch and Acosta22) ; it might also be related to other factors such as high homocysteine due to low vitamin B12, or possibly related to the low intake of animal protein, but further research is needed to examine these hypotheses.
The risk of diabetes in vegetarians in EPIC-Oxford was 35 % lower than that in meat-eaters(Reference Papier, Appleby and Fensom23); this was attenuated to 11 % lower and non-significant after adjusting for BMI at recruitment. The risk of diabetes in vegans was 47 % lower than that in meat-eaters, and this was attenuated to 1 % and non-significant after adjusting for BMI (there were only twenty-six cases among vegans)(Reference Papier, Appleby and Fensom23). The interpretation of these findings is that vegetarians and vegans in this population have a substantially lower risk of diabetes compared to meat-eaters, which appears to be largely or entirely due to their lower BMI.
Cancer
The risk for any type of cancer (all cancers combined) was 10 % lower in vegetarians than that in meat-eaters in EPIC-Oxford (Fig. 1), and 18 % lower in vegans (Fig. 2)(Reference Key, Appleby and Crowe24). For specific cancer sites, the only differences in risk were for stomach cancer and haematological cancers, which were 62 and 36 % lower, respectively, in vegetarians, and cancer of the cervix which was 90 % higher in vegetarians, all with rather wide CI due to the relatively small numbers of cancers at individual sites. The risk for colorectal cancer did not differ between vegetarians and meat-eaters. The reasons for the observed differences are not well understood although there is some limited other evidence suggesting that processed meat may increase the risk for stomach cancer(25). The higher risk of cancer of the cervix in vegetarians was unexpected and of borderline statistical significance; it is unlikely to be due to differences in screening, because reported attendance for cervical cancer screening does not differ between vegetarians and meat-eaters in the same cohort(Reference Tong, Appleby and Bradbury26).
The lower risk for all cancers combined in both vegetarians and vegans than that in meat-eaters in EPIC-Oxford is interesting but needs to be interpreted very carefully because few associations with individual cancer sites have been identified and several common cancers, such as lung cancer, are very strongly associated with smoking and therefore, although the results are adjusted for smoking status, there could well be residual confounding by this or by other non-dietary factors. Further research is needed to clarify whether vegetarian diets may affect the risk for a range of cancers; vegan diets are of particular interest because they are associated with lower circulating concentrations of the growth factor insulin-like growth factor-I, high levels of which probably increases the risks for colorectal, breast and prostate cancer, and also because characteristics such as the amino acid profile of vegan diets may have other metabolic effects which could perhaps reduce cancer risk(Reference Green, Lamming and Fontana27).
Fractures
In EPIC-Oxford, the risk for a bone fracture at all sites combined was 11 % higher in vegetarians compared to meat-eaters, which was reduced to 9 % higher after adjustment for BMI because the vegetarians have a lower BMI and BMI is itself inversely associated with fracture risk at certain sites, particular at the hip(Reference Tong, Appleby and Armstrong28). Larger differences were seen for hip fracture, for which vegetarians had a 34 % higher risk, reduced to 25 % higher after adjustment for BMI. In vegans, the risks for all fractures, before and after adjustment for BMI, were 50 and 43 % higher respectively, while the risks for hip fracture were 164 and 131 % higher, respectively. There was evidence of an interaction with BMI, since in vegans the risk for hip fracture was 3⋅17 (95 % CI 2⋅13, 4⋅71) among people with a BMI of less than 22⋅5 kg/m2 but 0⋅94 (0⋅38, 2⋅29) among people with a BMI of 22⋅5 kg/m2 and above (P for heterogeneity = 0⋅041), although this was based on small numbers in the subgroups.
The reasons for the moderately higher fracture risk in vegetarians, and substantially higher risk in vegans, are not clear. For vegetarians, calcium intakes are adequate and similar to those in meat-eaters, so other explanations are needed. Vegans in EPIC-Oxford have relatively low intakes of calcium and low circulating vitamin D, but adjustment for dietary calcium had only a moderate attenuating impact on the raised risk, and in an earlier analysis in this cohort we saw no relationship of circulating vitamin D with fracture risk(Reference Roddam, Neale and Appleby29). As noted earlier, the elevated risk of hip fractures was largely confined to people with a low BMI at recruitment (<22⋅5 kg m2), and it is possible that greater weight loss into older age may contribute to the higher risk in vegans; there are also other possibilities such as the lower insulin-like growth factor-I we have observed in vegans(Reference Allen, Appleby and Davey30–Reference Yakar, Werner and Rosen32), and the importance of nutrients such as calcium and protein may be underestimated in our analyses due to measurement error, a particular problem for calcium in vegans among whom a substantial amount may come from variably fortified foods.
Other disorders
In EPIC-Oxford, the linkage to hospital episode statistics data has enabled us to examine the risk of a range of other disorders in relation to the diet group. The risk of diverticular disease was observed to be 27 % lower in vegetarians and 72 % lower in vegans than that in meat-eaters, although the number of cases in vegans was only four(Reference Crowe, Appleby and Allen33); the lower risk in vegetarians and vegans (combined) was attenuated but remained statistically significant after adjusting for dietary fibre, suggesting that some of the lower risk is explained by fibre but that other factors such as meat itself may also contribute. The risk of gallstones did not differ between vegetarians and non-vegetarians(Reference McConnell, Appleby and Key34), but obesity causes a large increase in the risk for this condition and, after adjustment for BMI, vegetarians were observed to have a relatively high risk compared to meat-eaters (22 % higher risk), suggesting that some characteristic of the vegetarian diet may have an adverse impact; there was evidence that high starch intake was associated with a higher risk, but this did not appear to explain the relatively higher risk of vegetarians after adjusting for BMI. The risk of kidney stones was 31 % lower in vegetarians than that in high meat-eaters, and the risk of cataracts was lower in both vegetarians and vegans than that in high meat-eaters, but the reasons for these apparent differences are not known(Reference Turney, Appleby and Reynard35,Reference Appleby, Allen and Key36) .
All-cause mortality
In comparison with regular meat-eaters, all-cause mortality did not differ in vegetarians (hazard ratio 1⋅00 (95 % CI 0⋅93, 1⋅08)) or in vegans (hazard ratio 1⋅14 (0⋅97, 1⋅35))(Reference Appleby, Crowe and Bradbury37). Although diet is one determinant of long-term health, there are many other factors including smoking status, alcohol intake and socio-economic factors, so all-cause mortality has to be interpreted carefully because non-dietary differences between groups, although adjusted for as far as possible, may still influence the results through residual confounding. Based on the available data, however, it appears that overall mortality from all causes combined is broadly similar in vegetarians and vegans compared to that in meat-eaters.
Strengths, weaknesses and interpretation of the findings
The strengths of EPIC-Oxford are its moderately large size, extensive exposure data with biological samples for about 30 % of participants and nearly complete follow-up for almost two decades through National Health Service datasets on cancer, hospital episodes and mortality. The main weaknesses are that, while the number of vegetarians is large enough to study the more common endpoints (about 20 000 vegetarians), the number of vegans in the study is too small (about 2500 vegans) to give accurate relative risk estimates, and that as with other epidemiological studies the measurements of dietary and other factors are subject to error.
Interpretation of the results requires care. As with all observational epidemiological studies, the classification of people by diet group is imperfect, and the estimates of relative risks are subject to potential confounding by other factors such as smoking status, alcohol intake and socio-economic factors; all the results reported are adjusted for these factors as far as possible, but this adjustment is never perfect due to errors in the assessment of exposure to these factors, therefore the results can be affected by residual confounding if an exposure such as smoking is strongly related to the disease of interest. Another potential problem in most nutritional epidemiological studies is reverse causation, where people may change their diet because of early effects of a yet undiagnosed condition on their health or appetite; it is not clear if this is an important problem in the results reported, but most of the vegetarians and vegans had followed their diet for several years at the time of recruitment and therefore their choice of diet is unlikely to be due to diseases which were on average diagnosed many years later.
Another important factor to consider when interpreting the findings is the role of BMI. Vegetarians and vegans in EPIC-Oxford have a lower mean BMI compared to meat-eaters, and high BMI is a well-established risk factor for a number of diseases, therefore it would be expected that this difference would cause a moderately lower risk of these conditions in those on plant-based diets; by contrast, for some sites of bone fractures and possibly for some other conditions, risk is higher in people with low BMI. When answering the question ‘what is the association of a plant-based diet with long-term health?’, we have generally taken the view that the plant-based diet itself is a major determinant of the lower BMI, and therefore that the most appropriate relative risks are those which are not adjusted for BMI (this is analogous to our interpretation of the role of LDL-cholesterol, where we do not adjust for this measure because it is almost certain that the differences in LDL-cholesterol between vegetarians, vegans and meat-eaters are caused by the composition of the diet). However, to fully understand the relationship of plant-based diets with health it is helpful to also consider the relative risks after adjustment for BMI, an approach which answers the question ‘for people of the same BMI, does health differ between meat-eaters and those on a plant-based diet?’.
A further point to consider when interpreting the results is that they are from comparisons with the non-vegetarians who joined the study and thus are determined by the healthiness of the comparison group. The participants in EPIC-Oxford were all recruited over the same period with the same methods, and the non-vegetarians have broadly similar characteristics to those of the vegetarians, such as similarly low rates of smoking and obesity. Thus the comparisons can be considered to be quite stringent, and both the vegetarians and the non-vegetarians in the cohort are generally healthier compared to the average for the UK population; during the first 9 years of follow-up the standardised mortality ratios of vegetarians and non-vegetarians were only about 40 % of the average for the UK(Reference Key, Appleby and Davey38).
Conclusions
The plant-based diets of people in EPIC-Oxford who are vegetarians or vegans differ from those of meat-eaters, but for most nutrients the intakes of both groups are nutritionally adequate and meet or are close to meeting other government guidelines for good health, and many of the differences are quite small. Perhaps the most important potentially beneficial difference is the lower intake of saturated fat of those following plant-based diets and consequently their lower plasma LDL-cholesterol, which probably largely explains their lower risk of IHD. The higher intake of dietary fibre may also contribute to the lower risk of some disorders, particularly diverticular disease and possibly other disorders of the gastro-intestinal tract.
Potentially deleterious differences noted in people following plant-based diets are the lower average intakes and plasma concentrations of vitamin B12 and vitamin D, and the lower average intake of calcium in vegans. Vitamin B12 is of particular concern, since half the vegans studied had circulating concentrations indicating deficiency and this would be expected to have adverse effects on long-term health; for example, one possible explanation of the higher risk of stroke in vegetarians and vegans (combined) is that it is due to low vitamin B12 leading to raised homocysteine and increased stroke risk, and more research is needed to investigate this relationship. Although not discussed in detail here, vegans also typically have low plasma concentrations of long-chain n-3 fatty acids, and low intakes of iodine unless they consume seaweed, fortified food, iodised salt or supplements. For all these nutrients, further research is needed to determine whether there are adverse effects on health endpoints and importantly whether any risks can be prevented by adequate food fortification and/or supplementation, for example for vitamin B12. Furthermore, the availability of plant-based foods, particularly substitutes for meat and fish, is expanding and their characteristics are evolving, therefore new studies are needed to examine the impacts of these changes; these should include examination of temporal changes in the consumption of these products, and ascertaining whether the dietary characteristics of people who have recently adopted a plant-based diet differ from those of people such as those in EPIC-Oxford who have followed such diets for a much longer period. Further research is required, and it would be ideal to recruit a large new cohort including tens of thousands of vegans, with the best available methods to measure diet, to eventually provide reliable evidence on their long-term health.
Acknowledgements
We thank all the participants in EPIC-Oxford and colleagues past and present at the Cancer Epidemiology Unit.
Financial Support
This study was supported by Cancer Research UK A29017; Medical Research Council MR/M012190/1; Wellcome Trust Livestock, Environment and People 205212/Z/16/Z.
Conflict of Interest
None.
Authorship
The authors had sole responsibility for all aspects of preparation of this paper.