Maternal and child undernutrition remains one of the significant causes of millions of deaths and disability every year(Reference Black, Victora and Walker1). Low- and middle-income countries (LMIC) in particular face the brunt of this global crisis where pregnant women have a much higher risk of iron deficiency anaemia (IDA)(Reference McLean, Cogswell and Egli2), inadequacy of vital micronutrients, proteins and energy(Reference Beal, Massiot and Arsenault3). This results in a high proportion of adverse pregnancy outcomes such as low birth weight and stunting in infants born in these regions(4).
During pregnancy, the requirements of energy, protein and essential micronutrients (vitamins and minerals) increase not only to maintain the mother’s health but also to support optimal physical and brain development of the foetus(Reference Beal, Massiot and Arsenault3). Public health interventions in many countries target diet, nutritional supplements, multiple micronutrients during pregnancy and have shown beneficial effects on reducing preterm births and low birth weights(Reference Ramakrishnan, Imhoff-Kunsch and Martorell5). In the Indian context, evidence suggests that the top two risk factors causing disability and premature deaths are related to malnutrition and poor diet(Reference Dandona, Dandona and Kumar6). Moreover, despite the considerable reductions in maternal and child mortality in the last decade, nutritional indicators associated with women and children remain deplorable(7).
To address undernutrition among pregnant women, the federal Indian government focused on two national programmes, namely, provisioning of iron and folic acid (IFA) tablets/syrup and supplementary food (SF) to women during pregnancy(Reference Kotwal, Murugkar and Ramaswami8) with the objective of reducing the burden of IDA(Reference Rai, Fawzi and Barik9), and improving the overall nutrition. Under the National Iron+ Initiative, pregnant and lactating women are prescribed a dose of 100 mg elemental Fe and 500 μg folic acid, with a prescribed regime of one tablet daily for 100 d (IFA100), starting after the first trimester, at 14–16 weeks of gestation, and repeated up to 100 d postpartum(Reference Rai, Fawzi and Barik9). On the other hand, the Mid-day Meal Scheme (MMS), the Integrated Child Development Services (ICDS), the Mahatma Gandhi National Rural Employment Guarantee Scheme (MGNREGS) and the Public Distribution System (PDS) were devised to reduce undernutrition by providing supplementary food (SF) directly or by offering economic support to secure food for the household(Reference Kotwal, Murugkar and Ramaswami8). A further step was taken with the introduction of the National Food Security Act (NFSA) 2013, and priority was given to food and nutrition security among women(Reference Kotwal, Murugkar and Ramaswami8). The NFSA outlines that women are to receive supplementary nutrition – which consists of one meal that meets basic nutritional standards, free of charge, during pregnancy and 6 months after childbirth – through the local anganwadi centres. Eligible women are entitled to take home ration, which supplements 2510 kJ (600 kcal) of energy with 18–20 g of protein(Reference Kotwal, Murugkar and Ramaswami8).
Several studies have analysed IFA and micronutrient uptake among pregnant women in Africa(Reference Harika, Faber and Samuel10), Indonesia(Reference Wiradnyani, Khusun and Achadi11), Cambodia(Reference Raut, Reddy and Rahman12) and India(Reference Varghese, Swaminathan and Kurpad13). A few studies from India suggest that the effectiveness of IFA and SF intervention to reduce undernutrition remains far from expected, although both programmes seem to have helped in improving coverage(Reference Rai, Fawzi and Barik9,Reference Drèze and Khera14) .
An often-repeated query is about the access and adequate utilisation of healthcare programmes. In the present context, whether and to what extent the pregnant women, as beneficiaries of public nutritional interventions, are receiving the benefits of these nutritional health programmes remains unclear. Moreover, considering the huge regional differences in culture, healthcare infrastructure and socioeconomic status, it would be useful to explore the links and associations at multiple levels leading to the utilisation of maternal nutrition programmes in India. Existing empirical literature does not provide adequate evidence in this direction, as most of the studies have attempted to capture individual-level factors responsible for public health nutrition interventions, ignoring the role of programme and contextual determinants in such a diverse country(Reference Rai, Fawzi and Barik9,Reference Chakrabarti, Raghunathan and Alderman15) . Building upon the present gaps in scientific literature, this study examines the individual, programmatic and contextual factors associated with the utilisation of two important interventions related to maternal nutrition, including IFA and SF, in India. Moreover, the results of this study could guide the evaluation of such programmes implemented in other LMIC.
Methods
Conceptual framework
This study follows the WHO–Commission on Social Determinants of Health (CSDH) framework(16) to understand the individual, socioeconomic, programmatic and contextual factors responsible for the uptake of IFA100 and SF. The framework illustrates how social, economic and political mechanisms promote socioeconomic positions, whereby populations are stratified according to income, education, gender, race/ethnicity and other factors. These socioeconomic positions, in turn, shape specific determinants of health status or health services, and reflect people’s place within social hierarchies. Following the CSDH framework, the variables constructed to understand the individual, programmatic and contextual factors can be categorised as below.
1. Socioeconomic factors – These include maternal age at birth of the referenced children, women’s education, parity, gender composition of living children, caste/social group, wealth quintile and religion.
2. Programmatic factors – These include the timing of prenatal care in terms of months of pregnancy, total number of prenatal visits, meeting community healthcare providers during pregnancy and the place where antenatal care (ANC) was received.
3. Compositional/contextual factors – These include the proportion of illiterate and poor population in the community, that is, the primary sampling unit (PSU), and the proportion of registered pregnancies in the district along with place and region of residence.
A detailed description of these factors is given in the following sub-section related to explanatory variables.
Data and sample
This study is based on the fourth round of the National Family Health Survey (NFHS) conducted during 2015–16 across all twenty-nine states and seven union territories of India(7). The NFHS is an adaptation of the Demographic and Health Survey of India. A two-stage stratified random sampling was used to draw samples from both urban and rural areas. Villages in rural areas and Census Enumeration Blocks (CEB) in urban areas served as the PSU or clusters. A total of 28 586 PSU were selected across India. The household response rate was 98 %, whereas it was 97 % among women. A detailed description of survey design, sample and stratifications is available online at http://rchiips.org/nfhs/NFHS-4Report.shtml. The study sample includes 190 898 ever-married women aged 15–49 years who had at least one live birth in the 5 years preceding the survey. The sample represents a generalisable characteristic of Indian women as the distribution of the sample across social group/caste, religion and place of residence (rural/urban) followed the Indian Census 2011 statistics (see online supplementary material, Supplemental Table S1).
Outcome variables
The consumption of a recommended dose of IFA (i.e. at least one tablet or equivalent amount of syrup per day for 100 d) and receiving SF during pregnancy are considered the outcome variables of this study. In NFHS-4, women were asked to report the number of days they took IFA tablets during pregnancy. Similarly, women respondents were asked to provide information on whether they received SF during pregnancy if they responded to receiving any benefit from the anganwadi/ICDS centres. The WHO strongly recommends daily oral IFA supplements during pregnancy as part of prenatal care to reduce the risk of low birth weight, maternal anaemia and Fe deficiency(17). Pregnant and lactating mothers are entitled to receive cooked food served at anganwadi centres on a daily basis or take-home food provisions as per the guidelines of the Ministry of Women and Child Development, Government of India. The SF provided to pregnant and lactating women at the centre is supposed to include 2510 kJ (600 kcal) of energy and 18–20 g of protein per day in the form of micronutrient-fortified food and/or energy-dense food as take-home ration(18).
Explanatory variables
Individual/household factors
Women’s characteristics analysed were age, education (categorised based on the highest years of schooling attained) and parity. The gender composition of living children to women was considered a proxy variable to assess the behavioural aspect of women, reflecting their earnestness towards pregnancy care. Women’s affiliation to the social group – documented as caste (categorised as Scheduled Castes (SC), Scheduled Tribes (ST), Other Backward Classes (OBC) and Others (who are not eligible to receive incentives from the government)) and religion (categorised as Hindu, Muslim and Others) – is also considered along with their household economic status (measured in terms of wealth quintiles: poorest, poorer, middle, richer and richest). Previous studies have found that these variables had considerable influence in determining the interventions addressing maternal nutrition during pregnancy(Reference Selvaraj, Arumugasamy and Sarkar19,Reference Warvadekar, Reddy and Sharma20) .
Programme-dependent factors
During early pregnancy, the health system contacts at various platforms are evidenced to influence the utilisation of other health services in continuum. Thus, the utilisation of these services is determined by important programme-dependent factors – contact of women with healthcare providers (at home or at other places) during pregnancy, time of first prenatal care or registration with the health facility (in terms of month of pregnancy: within or in the 3rd month, 4th–5th month, and in the 6th month or later), number of prenatal care visits and place where prenatal care was received. Early pregnancy registration with the health facility or community health workers was significantly associated with the consumption of IFA supplements, and a health worker is more likely to visit those pregnant women who were registered for prenatal care(Reference Varghese, Swaminathan and Kurpad13).
These health system contacts also work as a proxy for nutrition education and counselling (NEC) given during pregnancy. Studies around community-based distribution (CBD) of IFA supplements and NEC have shown these to be effective strategies in increasing the consumption of IFA tablets among pregnant women(Reference Kavle and Landry21). The CBD is a strategy to provide IFA supplements to women directly through community channels, such as private pharmacies, community health centres, village health workers, community health workers, community volunteers or community gatherings for health education sessions(Reference Alam, Rasheed and Khan22).
Compositional/contextual factors
The associations between shared spatial attributes in the neighbourhood and health outcomes/behaviours are well documented in public health literature(Reference Subramanian, Chen and Rehkopf23,Reference Stephenson, Baschieri and Clements24) . The theories of social capital(Reference Coleman25,Reference Das and Teng26) , including social networks and relationships(Reference Coleman25,Reference Das and Teng26) , community awareness and diffusion(Reference Gage and Guirlène Calixte27), provide a framework for understanding the mechanism through which communities may influence the utilisation of healthcare services. The proportion (%) of illiterate persons in a PSU and the proportion (%) of the poor in a PSU, as well as the type of residential place (rural or urban), were included in the study to reflect the impact of shared community/neighbourhood on the use of health nutrition services. In NFHS, one PSU is more often the size of a standard village (with >40–50 households) in rural areas, and Indian villages are still a cohesive unit in terms of socialisation. A close urban neighbourhood would also incur more or less a similar aggregate impact on the utilisation of health services by individuals in that community.
In India, the district serves as the lowest programme implementation unit in the overall administrative hierarchy. Literature suggests that the role of individual, household and community factors differs from one geographic setting to another(Reference Babalola and Fatusi28). A few area-specific contextual factors, such as the proportion (%) of pregnancy cases registered in districts, and state groups, are also included in the study. The Government of India has designated eight states (Bihar, Chhattisgarh, Jharkhand, Madhya Pradesh, Orissa, Rajasthan, Uttarakhand, Uttar Pradesh) into the ‘Empowered Action Group’ (EAG) and Assam under a group of ‘High Focus States’ (HFS), which account for about 48 % of India’s population.
Analytical strategies
Owing to the hierarchical structure of the data and the nature of factors, especially compositional or contextual factors, namely individuals (level 1) grouped in clusters (level 2) and then in districts (level 3), a multilevel framework was adopted to analyse the influence of covariates at individual/household, community and district levels on the utilisation of nutritional interventions during pregnancy. From a statistical perspective, this structure of data (grouped data) implies a violation of the assumption of independence among observations within the same second- and third-level units, that is, individuals living in the same community and district(Reference Agresti and Kateri29). To address the structure of data and the binary nature of outcome variables, we applied a multilevel binary logistic regression model with random intercept specification that includes random intercepts and fixed slopes at specified levels(Reference Goldstein30). A major impetus for examining the role of contexts in explaining health variations comes from the advances in quantitative methods, in particular those related to multilevel statistical methods(Reference Goldstein and Healy31).
Data analysis was performed with Stata (version 14)(32) using the ‘xtmelogit’ command for a logistic linear random intercept model. Bivariate associations between plausible factors and outcome variables were checked using χ 2 tests. Factors found to be significant in the χ 2 test were included in the multivariate analyses. Before applying multivariate analyses, the intercept-only model (referred to as the ‘empty model’) was estimated for both outcomes. Intra-class correlation coefficients (ICC) were estimated to assess heterogeneity at the community and district levels. ICC refers to the proportion of total variance that is accounted for by the group level. The likelihood ratio test was incorporated to see whether the estimated variances were significant. A separate analysis between HFS and non-High Focus States (NHFS) was conducted to examine the differences in the determinants of IFA consumption and receiving SF during pregnancy.
In addition, based on the full model estimated for both outcomes, district-specific (posterior) residuals were estimated and mapped using ArcGIS suite. Residual mapping is an extremely useful application of multilevel models to present the model-based implications for policy and programme implementation, or the observed heterogeneity at the level of administrative decision-making and implementation(Reference Subramanian, Duncan and Jones33).
Results
Differentials in the uptake of iron and folic acid and supplementary food
Table 1 presents the proportion (%) of women consuming IFA and receiving SF by select characteristics. All the listed characteristics had a statistically significant association with both outcome measures. Less than one-third of women (30 %) reported consuming IFA, while slightly more than half (52 %) confirmed receiving SF during pregnancy. The consumption of IFA100 was relatively higher among women who were educated, lived in an urban area and belonged to a socioeconomically advantageous background. Further, the consumption of IFA was higher among women who did early pregnancy registration (38 %) and those who received ANC services at least once by any doctor (40 %) or at higher-level facilities. On the other hand, women who were in contact with community health workers or received prenatal services at least once from community health workers or at ICDS centres or sub-centres received SF in higher proportions.
Table 1 Proportion (%) of women consuming iron and folic acid for at least 100 d (IFA100) and receiving supplementary food (SF) during pregnancy in the 5 years preceding the survey by selected background characteristics, National Family Health Survey, 2015–16

ICDS, Integrated Child Development Services; SC, sub-centre; ANC, Antenatal Care; ANM, Auxilliary Nurse Midwife; LHV, Lady Health Visitor; CHW, Community Health Worker; ICDS, Integrated Child Development Services; ASHA, Accredited Social Health Activist; CHC, Community Health Centre; PHC, Primary Health Centre.
District-wise pattern in the utilisation of IFA (Fig. 1(a)) and SF (Fig. 1(c)) shows considerable variations. Out of 640 districts, 156 and 44 had <15 % coverage of IFA and SF, respectively. Moreover, only eighty-seven districts had >55 % coverage of IFA, while the number of corresponding districts receiving SF was 333. Districts with a lower coverage of both services were largely concentrated in the north, east and western states of India.
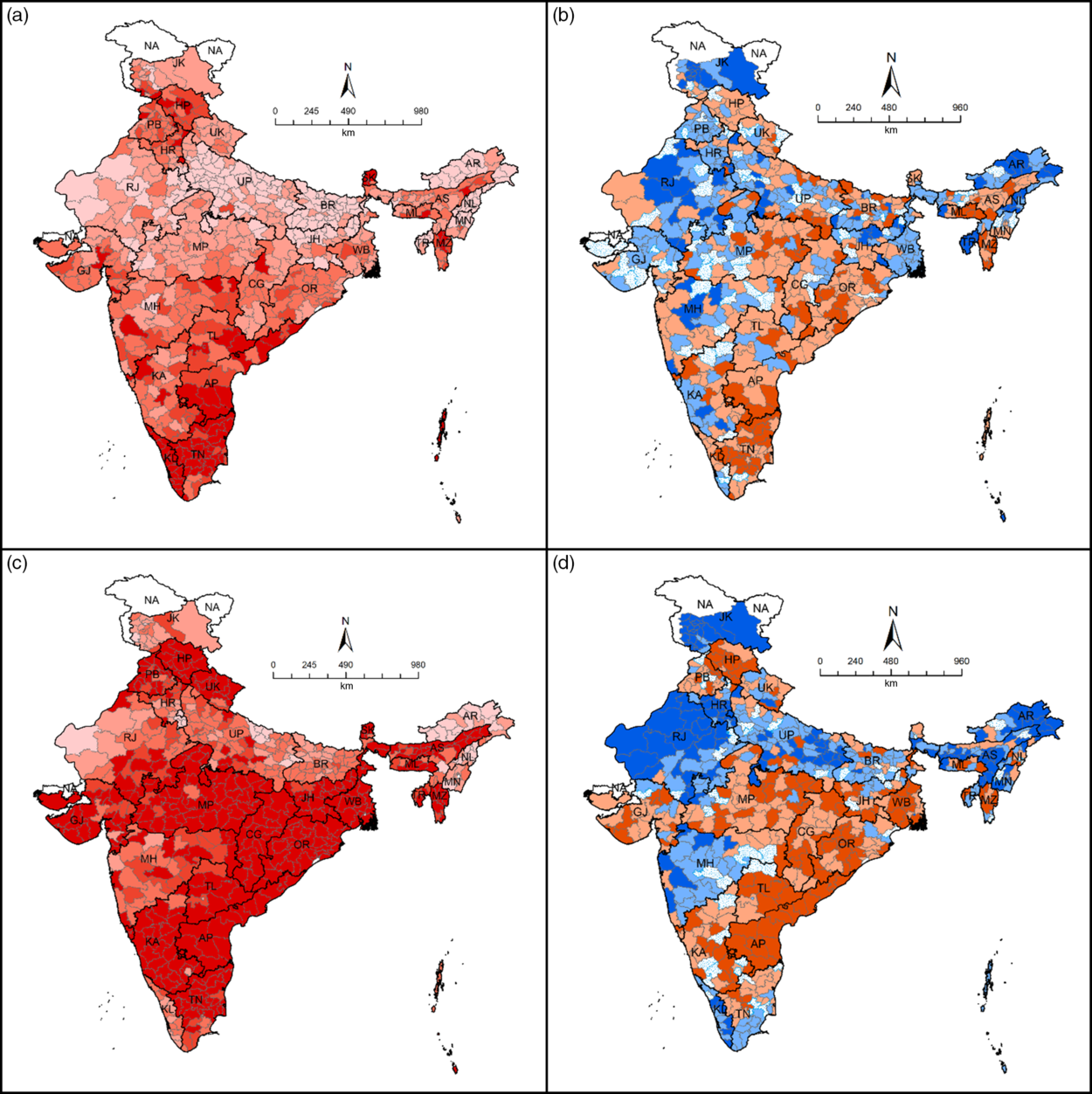
Fig. 1 Iron and folic acid tablets/syrup consumption (%) for at least 100 d (IFA100), supplementary food (SF) received (%) and their model-based heterogeneity across districts of India, National Family Health Survey-4 (2015–16). (a) Proportion of women (15–49) (%) consuming IFA100 during pregnancy. (b) District-level residuals (variances) map for IFA100. (c) Proportion of mothers (%) receiving supplementary food from an anganwadi/Integrated Child Development Services centre during pregnancy. (d) District-level residuals (variances) map for SF. (a and c) ![]() , < 15·0;
, < 15·0; ![]() , 15·0–30·0;
, 15·0–30·0; ![]() , 30·1–45·0;
, 30·1–45·0; ![]() , 45·1–55·0;
, 45·1–55·0; ![]() , > 55·0;
, > 55·0; ![]() , data not available. (b and d)
, data not available. (b and d) ![]() , < –0·70;
, < –0·70; ![]() , –0·70 to –0·11;
, –0·70 to –0·11; ![]() , –0·1 to 0·10;
, –0·1 to 0·10; ![]() , 0·11–0·70;
, 0·11–0·70; ![]() , < 0·70;
, < 0·70; ![]() , data not available
, data not available
Factors associated with the use of iron and folic acid tablets/syrup for at least 100 d and supplementary food
The results of the random intercept-only model (Table 2) infer that there were considerable variations in the utilisation of IFA (26 % at district level and 44 % at PSU level) and receipt of SF (31 % at district level and 53 % at PSU level). Findings of a multivariate logistic regression analysis suggest that the use of IFA during pregnancy was significantly determined by the women’s age at childbirth (positively associated), education (positively associated), parity (negatively associated), economic status (positively associated), caste and religious affiliation (Table 3).
Table 2 Parameter coefficients for the multilevel model (random intercept-only model, without covariates) for iron and folic acid tablets/syrup for at least 100 d (IFA100) and supplementary food (SF), National Family Health Survey (2015–16)

s 2, variance; PSU, primary sampling unit.
Table 3 Multilevel binary regression analysis for iron and folic acid tablets/syrup for at least 100 d, India, 2015–16

ANC, antenatal care; ICDS, Integrated Child Development Services; SC, sub-centre; PSU, primary sampling unit; ANM, Auxilliary Nurse Midwife; LHV, Lady Health Visitor; CHW, Community Health Worker; ICDS, Integrated Child Development Services; ASHA, Accredited Social Health Activist; CHC, Community Health Centre; PHC, Primary Health Centre; AIC, Akaike's Information Criteria; BIC, Bayesian Information Criteria.
As far as programme-level factors are concerned, women who registered their pregnancy in the first trimester (OR 1·33, 95 % CI 1·09, 1·62), who were contacted by healthcare providers both at home and outside (OR 1·29, 95 % CI 1·23, 1·35), who had four or more ANC visits (OR 1·74, 95 % CI 1·68, 1·79) or who had at least one ANC visit at a higher-level facility showed higher odds of IFA consumption compared to women who received no ANC, who did not meet any healthcare provider during pregnancy or who received ANC at home. Women in the HFS had nearly 30 % less probability of using IFA100 compared to those from the NHFS. Similarly, women from the community with more female illiteracy had 14 % less probability of using IFA100. Similarly, the likelihood of IFA100 use was higher among those districts with a higher rate of pregnancy registration (OR 12·30. 95 % CI 7·94, 19·06).
In the case of women receiving SF (Table 4), findings suggest that women’s age at childbirth, educational status, parity, economic status, caste and religious affiliation were significantly associated factors. Those who registered their pregnancy in the first trimester (OR 1·41, 95 % CI 1·16, 1·72), who had four or more ANC visits (OR 1·08, 95 % CI 1·05, 1·12) and who had at least one ANC visit at an ICDS centre or sub-centre (OR 1·97, 95 % CI 1·85, 2·10) showed higher odds of receiving SF compared to women receiving no ANC and who received ANC at home. Similarly, women’s contact with healthcare providers during pregnancy increased their chance of receiving SF by nearly five times compared to those not meeting healthcare providers. The likelihood of women receiving SF was nearly 87 % higher in the HFS than in the NHFS. Further, in communities where more than three-fourths of women were illiterate, there was an 18 % less probability of their receiving SF. In addition, a higher proportion of pregnancies registered in a district confirmed a higher probability of women in that district receiving SF.
Table 4 Multilevel binary regression analysis for supplementary food, India, 2015–16

ANC, antenatal care; ICDS, Integrated Child Development Services; SC, sub-centre; PSU, primary sampling unit; ANM, Auxilliary Nurse Midwife; LHV, Lady Health Visitor; CHW, Community Health Worker; ICDS, Integrated Child Development Services; ASHA, Accredited Social Health Activist; CHC, Community Health Centre; PHC, Primary Health Centre; SC, Sub Centre; AIC, Akaike's Information Criteria; BIC, Bayesian Information Criteria.
Comparison between High Focus States and non-High Focus States
Findings suggest that caste affiliation significantly determined the consumption of IFA100 in HFS but not in the case of NHFS (see online supplementary material, Supplemental Table S2). Further, women from NHFS who visited government healthcare facilities for ANC were more likely to consume IFA than those who received ANC at home. For districts with >75 % coverage of pregnancy registration, IFA use was nearly 29 and 5·6 times higher in NHFS and HFS, respectively, compared to districts with <25 % pregnancy registration.
On the other hand, women who received ANC at any government health facility in NHFS had higher odds of receiving SF compared to those who received ANC at home (see online supplementary material, Supplemental Table S3). However, in the case of HFS, there was no significant difference in SF receipt between women who used a government health facility for ANC and those who did not. Further, in the case of HFS, the association between women residing in a poor community and receiving SF was statistically significant, which was not true in the context of NHFS.
Administrative area-specific (district) contextual effects
The random intercept-only model (Table 2) applied for IFA consumption illustrated that there were nearly 26 and 44 % variances (out of total variances) in the use of IFA at district and community levels, respectively, which could be due to some unobserved factors at these levels. However, the full IFA model (Table 3) explains around 62 % of district-level variances, illustrating the observed differences in the proportion of pregnancies registered across the districts. The final IFA model suggests that there were about 10 and 30 % of variances in the use of IFA, which could be explained through the differences in elements at the district and community levels, respectively.
A district-level residual map for IFA (Fig. 1(b)) clearly shows the clusters of districts in western Rajasthan, parts of Jharkhand, Maharashtra, Arunachal Pradesh, Nagaland and Tripura, which had relatively higher negative variances, suggesting that, due to some unobserved district-level factors, the use of IFA was at a suboptimal level in these clusters of districts. Similarly, around 20 and 38 % of variances in SF receipt could be explained through the differences in elements at the district and community levels, respectively (Table 4). A district-level residual map for SF use (Fig. 1(d)) shows clusters of districts in Rajasthan, Haryana, eastern Uttar Pradesh, parts of Maharashtra, Kerala, Assam, Arunachal Pradesh, Manipur, and Jammu and Kashmir having relatively higher negative variances, suggesting that, due to some unobserved district-level factors, the use of SF was at a suboptimal level in these clusters of districts.
Discussion
The findings of this study demonstrate that the determinants of utilisation of two most essential interventions of maternal nutrition during pregnancy include a few important components of prenatal healthcare programmes and aggregated (community-level) compositional or contextual factors.
Socioeconomic factors
The findings indicated an increasing trend of utilisation of IFA with increasing age and level of education, which is well supported by other studies(Reference Chourasia, Pandey and Awasthi34,Reference Wendt, Stephenson and Young35) . However, older women were found to be less likely to receive SF. Education status of women has been recorded in recent literature to factor in the overall awareness about relevant reproductive health programmes and beneficial policies at their disposal(Reference Sharma, Sharma and Choudhary36), including the utilisation of supplementary nutrition(Reference Vishnu, Nirgude and Rajarathnam37). Women’s parity was observed to influence the consumption of IFA and SF in opposite directions, where higher parity women were less likely to consume IFA and more likely to receive SF in contrast to primiparous women. Similar patterns of IFA consumption have been noted in other studies(Reference Alam, Rasheed and Khan22), which reflects the higher prevalence of anaemia among multiparous women(Reference Viveki, Halappanavar and Viveki38).
Concurrent to the results of other similar studies(Reference Chourasia, Pandey and Awasthi34,Reference Begum39) , the consumption of IFA was observed to be higher among economically well-off women, although they were less likely to receive SF. Further, women classified under the caste affiliation of OBC, SC and ST were found to be less likely to consume IFA but more likely to receive SF. The low consumption of IFA among women belonging to disadvantaged social classes could be due to lack of awareness regarding IFA’s beneficial effects on mother and baby, myths surrounding IFA use, low-risk perception of anaemia, limited availability of resources(Reference Nisar, Dibley and Mir40), lower use of ANC services(Reference Balarajan, Selvaraj and Subramanian41) and lesser autonomy at home(Reference Diamond-Smith, Gupta and Kaur42). This highlights the need to increase the outreach of counselling on IFA supplements to pregnant women from targeted social groups. Muslim women were less likely to consume IFA and receive SF, which is supported by similar studies(Reference Wendt, Stephenson and Young35) identifying that Muslim women often showed restricted utilisation of MCH services(Reference Singh, Rai and Alagarajan43).
Programme factors
Availing ANC during early pregnancy (within the first trimester) is a key to better utilisation of reproductive health services in continuum. This was observed to have a positive influence on IFA consumption and SF receipt. Similarly, making four or more prenatal visits as recommended had a positive influence on the utilisation of both IFA and SF. Parallel studies have found prenatal visits to be associated with improved awareness and consequent utilisation of IFA(Reference Roy, Mohan and Singh44).
When examining the place of prenatal care, women who received ANC at any government healthcare institution were more likely to consume IFA and receive SF than those who received ANC at home, which is supported by other studies(Reference Kumar and Singh45). The highest odds of consuming IFA and receiving SF was recorded among women who met with healthcare providers at home or elsewhere compared to those who did not meet at all.
Contextual factors
The influence of aggregated literacy among women in the community (e.g. village) was considerable in the utilisation of both maternal nutritional interventions. Education has been underlined by multiple studies to define health behaviour(Reference Conner and Norman46) and is considered one of the most influential factors in the utilisation of maternal healthcare services in developing countries(Reference Sridharan, Dey and Seth47). Therefore, without formal education, there is a higher chance of women in the community not being aware of the services, or developing misinformed perceptions about the same. On the other hand, the aggregated poverty of the community (at the PSU level) did not show a significant influence on the consumption of IFA, but this was influential in terms of the utilisation of SF. Socioeconomic status could influence the utilisation of ICDS services; for instance, it has been observed that the participation of upper- and middle-income households remains lower in availing SF-alike services(Reference Rao and Kaul48).
Concurrent to the findings relating to pregnancy registration and utilisation of supplements(Reference Warvadekar, Reddy and Sharma20,Reference Roy, Mohan and Singh44,Reference Khan and Raza49) , we found that as the percentage of pregnancy registrations increased in the district, IFA and SF utilisation increased, too. The utilisation of SF was likely to be higher among women belonging to rural households than their urban counterparts. As the distribution of SF was planned through an anganwadi, which is primarily a rural functional centre for women and childcare, proximity to the centre might possibly influence the utilisation of this particular ICDS service.
Women in the HFS were less likely to consume IFA and more likely to receive SF compared to those in the NHFS, while the opposite behaviour was observed in terms of the utilisation of SF. However, a further analysis revealed that women residing in NHFS, compared to those residing in HFS, had higher odds of consuming IFA100 if they had gone for their first prenatal check-up within 3 months of pregnancy and subsequently made four or more prenatal visits. The odds of consuming IFA100 increased almost thirty times among women in NHFS and about six times in HFS if the coverage of pregnancy registration exceeded three-fourth (compared to under one-fourth) in the district. Adherence to mandated IFA dosage has been found to be poor among women in HFS(Reference Chourasia, Pandey and Awasthi34), which could be understood in terms of infrastructural and evaluative lacunae faced by healthcare institutions(Reference Wendt, Stephenson and Young50) in these states.
This study found a better utilisation of SF in NHFS among women of higher parity, women who made an early prenatal care visit, women who went for four or more prenatal care visits and women who visited ICDS centres or sub-centres at least once in order to receive ANC. A higher proportion of illiterate women in the community in both HFS and NHFS showed a less likelihood of receiving SF. Similar to IFA uptake, a higher proportion of pregnancy registration in the district favoured women receiving SF, especially in HFS. Results also suggested that women from a community in HFS with a higher proportion of poverty were more likely to receive SF. Despite the infrastructural deficits observed by several studies(Reference Gupta, Gupta and Nongkynrih51),the increasing likelihood of women receiving SF indicated the popularity of free meals provided by anganwadis in HFS. However, the lower likelihood of women receiving SF in urban areas calls for a further exploration and implementation of relevant focussed interventions in both HFS and NHFS.
Study limitations
This study is based on an analysis of a large-scale multi-aspect cross-sectional data, which was not specifically designed to explore the utilisation of nutritional health programmes. Owing to its cross-sectional design, the possibility of exploring causation among variables is limited, while the use of self-reported data poses a possibility of over- or underestimation of outcomes attributable to recall errors. Although the variables were selected based on a thorough literature review and expert consultations, the amount of unobserved heterogeneity still left unexplained provides scope for future studies to incorporate more salient variables not captured by the NFHS. Moreover, based on the information given in the NFHS, it is not known whether the women received IFA tablets or syrup under the public health programmes or purchased by themselves. However, the objective of appraising the utilisation patterns of IFA and SF as maternal nutrition interventions is fulfilled to a large extent by this study.
Conclusion
This comprehensive cross-sectional study appraising the two pertinent public health interventions to improve maternal nutrition in India is of significant interest in terms of accounting for the observed potential socioeconomic, programmatic and contextual factors. The application of multilevel analysis also provided an opportunity to identify the administrative units where district-level contextual factors such as supply-side system-level functionaries could be responsible for undermining the utilisation of nutrition interventions. The study showed that the consumption of a recommended dosage of IFA improved with a better utilisation of prenatal health services, especially in communities where pregnancies were registered in higher proportions, when women regularly interacted with community health workers or healthcare providers during pregnancy, when women received their first prenatal check-up early in their pregnancy followed by more (at least four) such check-ups. Women’s education and their economic status were obvious favourable factors for IFA consumption. Similarly, the likelihood of receiving SF from an anganwadi/ICDS centre was higher among women having a regular contact with healthcare providers and making more number of prenatal visits, at least once at an ICDS centre or sub-centre. Women living in rural areas accounting for a higher registration of pregnancies and a higher proportion of households with poor economic status were more likely to receive SF. Stark differences in the utilisation of both maternal nutrition interventions within and between districts and between HFS and NHFS were evident in this study. Our results also revealed a considerable unobserved heterogeneity at community and district levels, even after controlling for a range of relevant potential factors. Repeated, focussed and concurrent monitoring as well as improvised implementation of public provisioning systems (such as community outreach programmes conducted by peripheral sub-centres, Village Health Nutrition Day, etc.) in the targeted areas would be a key for effective, sustainable and enhanced public health nutrition programmes in diverse community settings such as in India.
Acknowledgements
Acknowledgements: During the preparation of this article, the first author (P.K.S.) was a Max Planck India Mobility Fellow (M.PG.A.DEFO0002) at the Max Planck Institute for Demographic Research, Rostock, Germany. The authors thank anonymous reviewers for their helpful comments and feedback on an earlier draft of this article. We also thank the Demographic and Health Survey of India for providing the NFHS-4 micro datasets. Financial support: This study received no specific grant from any funding agency, commercial or not-for-profit sectors. Conflict of interest: The authors declare that there is no conflict of interest. Authorship: P.K.S., L.S. and C.K. conceptualised the study. P.K.S. and L.S. analysed the data. P.K.S., R.D., C.K. and R.K.R. wrote the article. All authors critically revised the article and approved the final manuscript. Ethics of human subject participation: The present study is based on anonymised NFHS data available in the public domain. Thus, no separate ethical clearance was required for this study.
Supplementary material
For supplementary material accompanying this article visit https://doi.org/10.1017/S1368980020001007









