The clinical effectiveness of psychological therapy is generally accepted (Department of Health, 2001), but current focus is on issues of cost and the efficient use of limited psychological therapy resources in publicly funded or managed healthcare systems (Reference Christensen and JacobsonChristensen & Jacobson, 1994; Reference HaagaHaaga, 2000; Reference Lovell and RichardsLovell & Richards, 2000; Reference NewmanNewman, 2000; Reference Scogin, Hanson and WelshScogin et al, 2003). At present psychological therapy services provide poor access, with only a minority of patients in need able to receive therapy (Reference Lovell and RichardsLovell & Richards, 2000) and the vast majority receiving no treatment (Reference Bebbington, Brugha and MeltzerBebbington et al, 2000). This is because the available treatment resource is limited by the relatively small number of trained therapists. A number of authors have recently suggested ‘stepped care’ as a solution (Reference Kaltenthaler, Shackley and StevensKaltenthaler et al, 2002; Reference Marks, Mataix-Cols and KenwrightMarks et al, 2003; National Collaborating Centre for Mental Health, 2003; Reference Scogin, Hanson and WelshScogin et al, 2003). This review considers the meaning of stepped care in relation to psychological therapies, reviews the current evidence to support stepped care and outlines the future research agenda.
STEPPED CARE MODELS
Stepped care is a model of healthcare delivery with two fundamental features. First, the recommended treatment within a stepped care model should be the least restrictive of those currently available, but still likely to provide significant health gain. Second, the stepped care model is self-correcting.
The definition of ‘least restrictive’ may refer to the impact on patients in terms of cost and personal inconvenience (Reference Sobell and SobellSobell & Sobell, 2000), but in the context of publicly funded healthcare systems where specialist therapist time is a key limiting factor, ‘least restrictive’ is often interpreted as referring to the amount of specialist therapist time required (i.e. treatment intensity). In stepped care, more intensive treatments are generally reserved for people who do not benefit from simpler first-line treatments, or for those who can be accurately predicted not to benefit from such treatments (Reference NewmanNewman, 2000). In this way, stepped care has the potential for deriving the greatest benefit from available therapeutic resources. However, the focus on low-intensity treatment delivery might actually be counter-productive, without the crucial self-correcting mechanism. ‘Self-correcting’ means that the results of treatments and decisions about treatment provision are monitored systematically, and changes are made (‘stepping up’) if current treatments are not achieving significant health gain. Rather than regarding withdrawal from therapy as a reflection of a lack of motivation for treatment on the part of the patient, stepped care models see monitoring of progress and outcome as a fundamental responsibility of therapists and the system of care within which they work. A simple two-step model is outlined in Fig. 1.
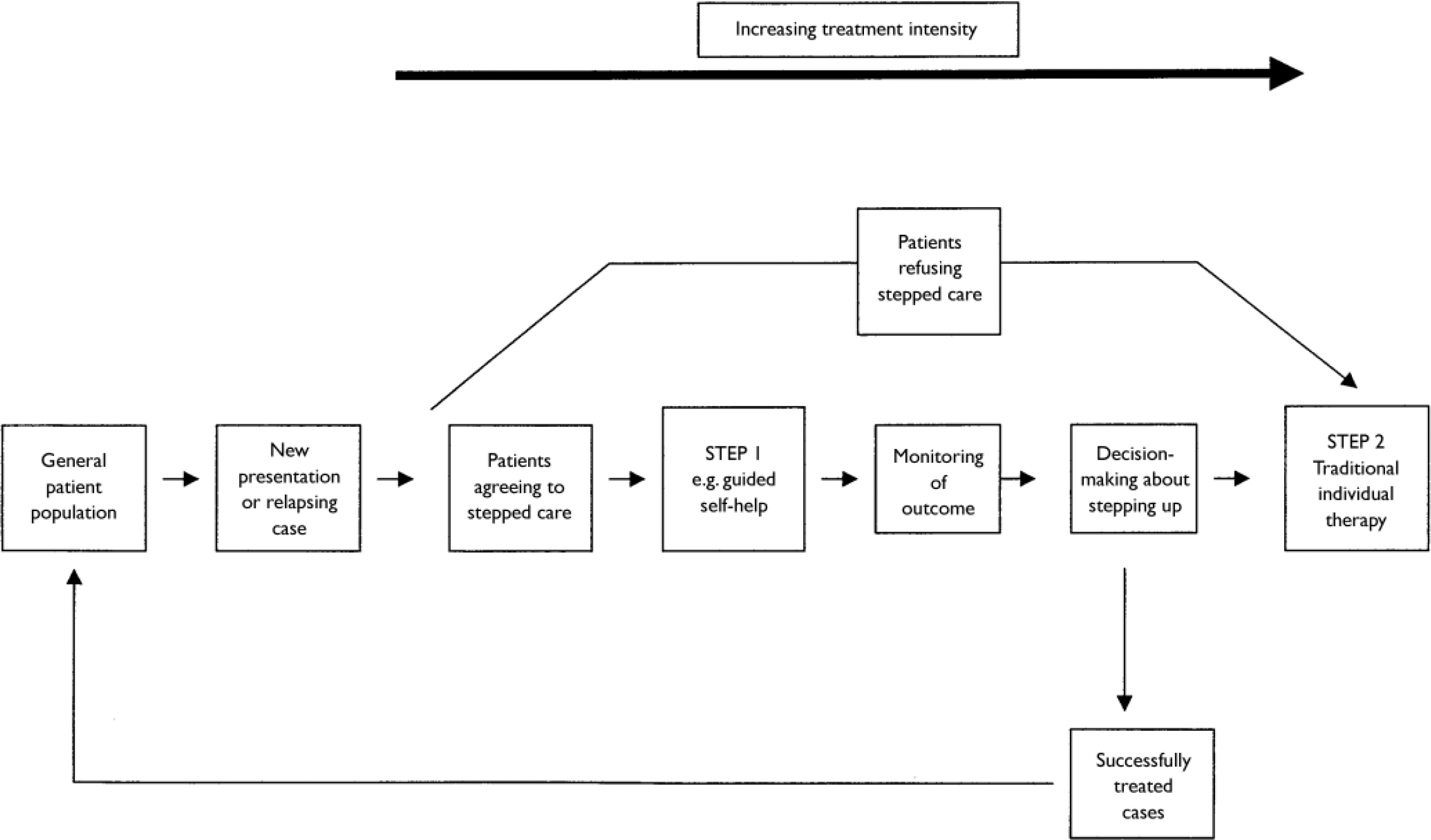
Fig. 1 Key elements in a simple stepped care model.
Although these features of stepped care may seem to resemble the way in which many clinicians implicitly operate (Reference Breslin, Sobell and SobellBreslin et al, 1997; Reference King, Stoller and HayesKing et al, 2002), stepped care standardises systems and procedures with an explicit aim of improving efficiency (Reference Katon, Von Korff and LinKaton et al, 1997; Reference Scogin, Hanson and WelshScogin et al, 2003). Stepped care models have been described in relation to smoking (Reference Abrams, Orleans and NiauraAbrams et al, 1996; Reference Smith, Jorenby and FioreSmith et al, 2001), back pain (Reference Von Korff and MooreVon Korff & Moore, 2001), alcohol treatment (Reference Breslin, Sobell and SobellBreslin et al, 1997; Reference Sobell and SobellSobell & Sobell, 2000), migraine (Reference Sculpher, Millson and MeddisSculpher et al, 2002), anxiety (Reference NewmanNewman, 2000), eating disorders (Reference Wilson, Vitousek and LoebWilson et al, 2000), methadone maintenance (Reference King, Stoller and HayesKing et al, 2002) and depression (Reference Simon, Katon and Von KorffSimon et al, 2001; Reference Scogin, Hanson and WelshScogin et al, 2003).
Key elements in stepped care models
What treatments are of relevance to stepped care?
Stepped care requires treatments of differing intensity. This requirement is amply satisfied in psychological therapies, where a number of less intensive treatments (or ‘minimal interventions’) have been developed, for example brief therapies (Reference Scott, Tacchi and JonesScott et al, 1997), group treatments (Reference Dowrick, Dunn and Ayuso-MateosDowrick et al, 2000) and self-help approaches such as bibliotherapy (Reference CuijpersCuijpers, 1997) and computerised treatments (Reference Proudfoot, Ryden and EverittProudfoot et al, 2004).
The main candidate for stepped care is cognitive–behavioural therapy. This therapy has been highlighted by guidelines as the treatment of choice for a number of disorders (Department of Health, 2001). It also has the advantage that there can be a degree of commonality between different ‘steps’, all being based on the same theoretical model and therapeutic techniques. There might be advantages to such consistency, although ‘stepping up’ to an approach that has already failed might be seen as counterproductive (Reference NewmanNewman, 2000). However, there is no requirement for stepped care to involve a single therapeutic approach (Reference DavisonDavison, 2000; Reference Sobell and SobellSobell & Sobell, 2000). Other brief treatments such as problem-solving (Reference Dowrick, Dunn and Ayuso-MateosDowrick et al, 2000) are of proven benefit, and a stepped care model might involve ‘stepping up’ from cognitive–behavioural bibliotherapy to counselling (Reference Ward, King and LloydWard et al, 2000) or interpersonal therapy (Reference Schulberg, Block and MadoniaSchulberg et al, 1996). Different treatments may have an effect on different aspects of the patient's problem (Reference NewmanNewman, 2000).
The issue of medication should also not be ignored. Generally, access to medication is not constrained in the same way as access to psychological therapy, because it does not generally require access to a specialist therapist. However, modern models of collaborative care do involve significant support from case managers to improve compliance with medication (Reference Badamgarav, Weingarten and HenningBadamgarav et al, 2003), and thus the principles of stepped care can be applied in this context (Reference Katon, Von Korff and LinKaton et al, 1999; Reference Araya, Rojas and FritschAraya et al, 2003; Reference Unutzer, Katon and CallahanUnutzer et al, 2003).
How many steps should be involved?
The number of steps will be bounded by two factors. First, there are only a finite number of interventions available that differ qualitatively in terms of intensity. Second, since stepped care seeks to reduce the average amount of therapeutic input per patient, an upper limit is provided by the amount of therapist input that is routinely provided in traditional services. In the UK National Health Service, this might be 8–16 sessions (50 min long) of face-to-face therapy, often cognitive–behavioural (Reference Lovell and RichardsLovell & Richards, 2000; Department of Health, 2001). Given this ceiling, there are probably four qualitatively different steps: pure self-help (no therapist input beyond assessment); guided self-help and group therapy (therapist input around 1–2 h per patient); brief individual therapy (therapist input around 6 h per patient); and longer-term individual therapy (therapist input around 16 h per patient). Different steps might use different professionals, with pure self-help at the initial step, followed by guided self-help from a practice nurse (Reference Richards, Richards and BarkhamRichards et al, 2002) or primary care mental health worker (Reference BowerBower, 2002), then individual therapy from a clinical psychologist or mental health nurse.
Much informal mental healthcare is undertaken by patients in the community without the intervention of mental health services (Reference Rogers, Hassell and NicolaasRogers et al, 1999), and the first level of any stepped care system might involve facilitating ‘natural recovery’ outside statutory services (Reference Sobell and SobellSobell & Sobell, 2000). However, the relationship between such community-level initiatives and statutory services is likely to be complex (Reference Abrams, Orleans and NiauraAbrams et al, 1996).
How are decisions to be made about ‘stepping up’?
‘Stepping up’ requires a decision about patient progress based on judgements about ‘significant health gain’ or ‘improvement’, but the exact definition will be dependent on the type of disorder, its natural history and the effectiveness of available treatments (Breslin et al, Reference Breslin, Sobell and Sobell1997, Reference Breslin, Sobell and Sobell1999; Reference Sobell and SobellSobell & Sobell, 2000). This might involve the use of ‘clinically significant and reliable change’ (Reference Jacobson and TruaxJacobson & Truax, 1991) or individualised ‘expected outcomes’ based on patient pre-treatment variables (Reference LutzLutz, 2003). In some disorders, different criteria might be relevant. For example, in depression, because residual symptoms are associated with later relapse, treatment until full remission has been recommended (Reference Scogin, Hanson and WelshScogin et al, 2003).
Decisions may be based on data collected within treatment (Reference Breslin, Sobell and SobellBreslin et al, 1997). The use of simple assessment and decision rules (e.g. a threshold score on the Beck Depression Inventory completed by a patient) has the advantage that this approach is cheap and easily standardised (Reference Scogin, Hanson and WelshScogin et al, 2003). More complex assessments by experienced clinicians might have advantages but would add significantly to costs, and it is important that the benefits of stepped care are not swallowed up by the professional time required to implement the system. Furthermore, professional decision-making may on occasion be less valid than judgements made on the basis of guidelines and decision rules (Reference Breslin, Sobell and SobellBreslin et al, 1997). There is also a trade-off between false positives (i.e. inappropriate ‘stepping up’) and false negatives (failure to ‘step up’ when appropriate), and the complexity of decision-making should therefore be sensitive to the costs of treatment at different steps (Reference Sobell and SobellSobell & Sobell, 2000).
The role of the patient requires consideration, as choice of treatment might be an important component of patient-centred services, but might also have important implications for efficiency within stepped care. The whole issue of the acceptability of stepped care to patients is dealt with in more detail below.
Which patients or disorders are appropriate for stepped care models?
Stepped care models may be most appropriate for disorders in which adverse consequences would not result from starting patients on too low a step, or where the perception of ‘treatment failure’ at lower levels does not greatly affect later outcome. For example, in the treatment of eating disorders, stepped care might be far more appropriate for bulimia and binge eating than for anorexia nervosa (Reference Wilson, Vitousek and LoebWilson et al, 2000). A recent model for depression (Reference Scogin, Hanson and WelshScogin et al, 2003) suggests that stepped care psychological therapy might be particularly relevant for minor depression, as opposed to major depression: the latter might be better managed through complex collaborative models of care (Reference Gilbody, Whitty and GrimshawGilbody et al, 2003). There is a general perception that minimal interventions are best restricted to less severe disorders, although the evidence for this is not definitive (Reference Lovell and RichardsLovell & Richards, 2000). However, it is important that decisions about the use of minimal interventions as a first-line treatment are made on the basis of good research evidence, as there may be cases in which early intensive treatment is actually more clinically effective and cost-effective than a minimal intervention.
CLINICAL AND ECONOMIC EVALUATION OF STEPPED CARE MODELS
Although the practical issues outlined above are important, current interest in stepped care is based on three fundamental assumptions:
-
(a) minimal interventions can provide ‘significant health gain’ equivalent to that of traditional psychological therapies, at least for a proportion of patients (equivalence assumption);
-
(b) using minimal interventions will therefore allow current healthcare resources to be used more efficiently (efficiency assumption);
-
(c) minimal interventions and the stepped care approach are acceptable to patients and professionals (acceptability assumption).
Equivalence assumption
There is evidence that minimal interventions can, like their more therapist-intensive versions, be more effective than ‘usual care’ or ‘no treatment’ conditions (Reference CuijpersCuijpers, 1997; Reference Dowrick, Dunn and Ayuso-MateosDowrick et al, 2000; Reference Lovell and RichardsLovell & Richards, 2000; Reference Bower, Richards and LovellBower et al, 2001; Reference Kaltenthaler, Shackley and StevensKaltenthaler et al, 2002). However, such comparisons are not the most relevant to the equivalence assumption. First, they do not compare minimal interventions with traditional, more intensive versions. Furthermore, they may also validate the efficiency assumption. For example, if a simple bibliotherapy treatment is superior to ‘no treatment’, providing bibliotherapy to patients would still need an overall increase in the amount of resources required – or cutbacks in other parts of the service – even if the bibliotherapy were relatively cheap. Whether that is worthwhile is a question of allocative efficiency (Reference Donaldson, Currie and MittonDonaldson et al, 2002). Only when a treatment costs less and provides equal effectiveness is it described as technically efficient, which is the key criterion for stepped care treatments. Therefore, published demonstrations of the benefits of ‘stepped care’ treatments v. usual care may not be definitive in the current context.
The key demonstration required to support stepped care models is the comparison of minimal interventions with traditional psychological therapy. A number of studies have reported that minimal interventions do not differ in effectiveness from more intensive, therapist-delivered treatments (Reference Lovell and RichardsLovell & Richards, 2000). However, the finding that there is no difference in the clinical effectiveness of two treatments does not prove that they are equivalent. Most psychological therapy trials are designed and powered to examine whether there are differences in effectiveness, whereas proving equivalence requires specific analytical procedures (Reference Rogers, Howard and VesseyRogers et al, 1996; Reference Ebbutt and FrithEbbutt & Frith, 1998) and routinely requires a larger sample size (Reference Hargreaves, Shumway, Hu, Miller and MagruderHargreaves et al, 1999; Reference Durand and KingDurand & King, 2003). A trial with a small sample size might conclude that two treatments did not differ significantly in a statistical sense, even though the outcomes differed in a clinically significant way.
This problem can be illustrated with respect to a recent systematic review of computerised cognitive–behavioural therapy. Six trials compared it with the therapist-led form of this therapy, and the review reported that five of them showed computerised therapy to be as good as the therapist-led treatment (Reference Kaltenthaler, Shackley and StevensKaltenthaler et al, 2002). However, the sample sizes per group in these studies ranged from 6 to 38, which means that the finding of ‘no statistically significant difference’ between the two forms of delivery of cognitive–behavioural therapy is likely to occur even in the presence of important treatment effects. This can be illustrated most easily by summarising the data in terms of standardised effect sizes, rather than statistical significance (available from the author upon request). In four trials reporting ‘no statistically significant differences’ between treatments, 32 comparisons were made between computerised and therapist-led cognitive–behavioural therapy, and 9 (28%) of these differences were either ‘medium’ or ‘large’ according to current conventions (Reference LipseyLipsey, 1990). This highlights the fact that small trials may report no significant difference between treatments that do in fact differ in clinically significant ways.
However, it should be noted that traditional equivalence trials examine equivalence at the level of the individual patient, whereas it is also possible to view this issue from the perspective of a population. For example, a modestly effective treatment that could be used with a large number of patients might provide more population health benefit than a more effective treatment that could only be provided to a small proportion of the population. An alternative trial design, the so-called outcome maximisation design (Reference SuttonSutton, 1997), seeks to determine how much overall clinical benefit can be derived from a given therapeutic resource. Such a design may be appropriate for testing whether traditional, intensive psychological therapies, which might be more clinically effective with individual patients, are also delivering greater benefits at the level of the population.
Efficiency assumption
Equivalent clinical outcomes in traditional and minimal interventions have been taken to imply that the latter are more efficient because of the lower amount of therapist input required. For example, studies in alcohol treatment have quoted data relating to ‘therapist hours per abstinent patient’ (Reference Wilson, Vitousek and LoebWilson et al, 2000). This may be valid from the perspective of a psychological therapy services manager. However, other stakeholders may require a more comprehensive analysis of costs, such as direct treatment costs in other sectors (e.g. primary care visits and medication, use of social services and voluntary sector providers) and patient costs (such as purchasing manuals or using private therapy). Limiting the analysis of costs to those associated with the psychological therapy service alone ignores the potential for cost-shifting to other sectors. Demonstrations of increased efficiency in stepped care models may be illusory if significant cost-shifting occurs. There is some evidence that patients receiving minimal interventions are more likely to seek additional interventions than those receiving traditional treatments (Reference Treasure, Schmidt and TroopTreasure et al, 1996; Reference Thiels, Schmidt and TreasureThiels et al, 1998).
Acceptability assumption
Patient attitudes to psychological therapy are generally very positive (Reference Priest, Vize and RobertsPriest et al, 1996), but it cannot be assumed that these positive attitudes will generalise to minimal interventions. Patients may feel that the provision of minimal interventions is inappropriate (Reference Scogin, Hanson and WelshScogin et al, 2003), especially for more severe disorders (Reference Landreville, Landry and BaillargeonLandreville et al, 2001). Trials of minimal interventions in primary care rarely report overall uptake rates to the offer of such treatment (Reference Bower, Richards and LovellBower et al, 2001). One non-randomised study found that one-fifth of patients motivated to return a screening questionnaire to a computerised self-help clinic refused computer-aided treatment when it was offered (Reference Marks, Mataix-Cols and KenwrightMarks et al, 2003). In another study, scarcely more than half of patients offered self-help while on a waiting list for cognitive–behavioural therapy took up the offer (Reference Whitfield, Williams and ShapiroWhitfield et al, 2001).
The issue of patient acceptability raises the possibility of tension between the desire to gain the greatest amount of clinical benefit from available resources, and the need to provide services that are patient-centred and meet current policy concerns with providing choice to patients. Clearly, the goal is to allow patients to have a role in treatment decision-making, and there are published trials in which psychological therapy and pharmacotherapy treatments were both available within a stepped care model, and patients could choose between them in collaboration with their clinicians (Reference Unutzer, Katon and CallahanUnutzer et al, 2003). Equally, within a stepped care system such as that outlined in Fig. 1, patients may be provided with a choice of interventions within steps (for example, guided self-help, computerised cognitive–behavioural therapy or group therapy at step 1), even if choices between steps are more constrained. However, the efficiency benefits of stepped care may be determined in part by constraints on choice: for example, offering minimal interventions such as bibliotherapy at the first step may have little effect if patients are allowed to choose more intensive treatment, and if most have an expectation of (and preference for) the latter type of treatment.
A second important issue is the acceptability of stepped care to professionals. Trials may be conducted by advocates of minimal intervention, and it cannot be assumed that all professionals will feel comfortable with the philosophical assumptions that underpin stepped care models or the changes to working methods that may be required (Reference Cushman and GilfordCushman & Gilford, 2000).
Equivalence, efficiency and acceptability assumptions in published ‘stepped care’ trials
There are few studies of a complete stepped care model. Two relevant studies of stepped care for eating disorders have been conducted in the UK (Reference Treasure, Schmidt and TroopTreasure et al, 1996; Reference Palmer, Birchall and McGrainPalmer et al, 2002), and one is considered here in detail to highlight important issues relating to the equivalence, efficiency and acceptability assumptions. This trial compared standard 16-session cognitive–behavioural therapy for bulimia nervosa with a stepped care model, in which the first step was the use of a self-help manual for 8 weeks (Reference Treasure, Schmidt and TroopTreasure et al, 1996). After this period patients were assessed, and those who no longer met ICD–10 criteria for bulimia were not offered further therapy, whereas those who did were offered eight sessions of cognitive–behavioural therapy. Sample size at baseline was 55 per group. In the stepped care arm, 16 out of 41 patients (39%) were deemed to be recovered at 8 weeks and were not offered further therapy. Of the remaining patients, 9 were offered treatment but did not take it up. There was an 11% difference in withdrawal rates in favour of the stepped care group. In terms of outcomes, end-of-treatment abstinence rates in both groups were 30%, and at 18 months remission was 40% in the stepped care group and 41% in the traditional treatment group. Outside the trial, 38% of patients in the stepped care group sought extra treatment, compared with 17% of the traditional treatment group.
The trial does highlight some of the problems in providing a rigorous evidence base for stepped care. First, it should be noted that none of the main results listed (relating to withdrawal from the trial, other treatment or clinical outcome) were reported as being statistically significant, although the differences reported in withdrawal rates and treatment outside the trial may be important clinically and economically. This highlights the problems of demonstrating equivalence when the sample size is relatively modest. The trial did provide some evidence of similar outcomes in the less intensive treatment arm, and implementation would allow more patients to be treated from the same therapeutic resources. However, this evidence of efficiency was restricted to the psychological therapy service, and there were no data on where the ‘extra treatment’ was sought and where the costs fell (e.g. on the wider healthcare system or the patient). Also, the costs of the ‘stepping up’ assessment were not taken into account. No specific data were presented on the acceptability of the model, although the rates of withdrawal suggest that the manual was generally acceptable to patients.
FUTURE RESEARCH AGENDA
The acceptability of stepped care is crucial for effective implementation; however, there is little information about this. Research on the patient acceptability assumption would need to access the views of a number of different populations, including not only those attending traditional psychological therapy services (who may be the first to enter stepped care models) but also those in primary care and the wider community, who currently do not access services but might be able to, if more efficient services were implemented. The views of these patients may differ in important ways (Reference Meltzer, Bebbington and BrughaMeltzer et al, 2000).
Given the concerns discussed above about current evidence on the equivalence and efficiency assumptions, the initial research agenda needs to focus on rigorous evaluations of these assumptions in the comparison of a selection of current minimal interventions (such as bibliotherapy and computerised treatments) with traditional psychological therapy. Such studies would provide evidence concerning the components of the stepped care model, but not about the model as a whole. Observational evaluations of a functioning stepped care model could be used to examine issues such as patient throughput within the various steps, issues relating to decision-making about ‘stepping up’ and possible negative effects of treatment failure at lower steps and loss of continuity caused by changes in providers. As noted above, economic benefits might be dependent on patients restricting their help-seeking to the minimal interventions provided, and qualitative research to understand patient decision-making would be useful (Reference Pilgrim, Rogers and ClarkePilgrim et al, 1997; Reference Breslin, Sobell and SobellBreslin et al, 1999).
The final stage in the research agenda would be a controlled trial evaluation to compare an entire stepped care model with a traditional model of service delivery. This might require a large-scale cluster randomised trial (Reference Gilbody and WhittyGilbody & Whitty, 2002), and would seek to quantify the overall public health benefit of traditional and stepped care models.
However, the time required to complete such an ambitious research agenda may significantly delay service development. A more efficient alternative might be the use of modelling, which refers to the use of mathematical simulations to assess outcomes and costs associated with different health technologies and patient populations (Reference Chilcott, Brennan and BoothChilcott et al, 2003). Modelling could identify the potential for stepped care to be both clinically effective and cost-effective based on current data; in addition, models might be useful to extend results from existing randomised controlled trials and in the design of future trials (Reference Chilcott, Brennan and BoothChilcott et al, 2003).
First, modelling could be used to extend current trial data by examining longer-term outcomes (e.g. relapse and recurrence), different comparators, the effect of context (e.g. US data in the UK setting) and the effects of minimal interventions within a broader system of care (Reference Brennan and AkehurstBrennan & Akehurst, 2000). For example, modelling could be used to determine the optimal number of steps in a stepped care model (Fig. 1), by identifying the number that provided the best potential trade-off between efficiency and complexity. Cost-effectiveness within a model could be examined from a wider societal perspective than is the case with existing research. Data on the effects of different interventions in the hierarchy of stepped care could be combined to examine pathways through the model of a hypothetical cohort of people with depression (Reference Valenstein, Vijan and ZeberValenstein et al, 2001). The effect of the patient acceptability assumption could be modelled by examining the effect of assuming that different proportions of patients refuse to enter the lower levels of the hierarchy and enter more intensive steps.
Second, modelling could assist in informing the design of future trials and indicating their likely value. Models could help to specify an appropriate equivalence limit for future comparisons of minimal interventions and traditional therapy, suggest the optimal length of follow-up of outcomes (Reference Chilcott, Brennan and BoothChilcott et al, 2003) and highlight the key parameters that determine the likely cost-effectiveness of stepped care, and thus assist in the prioritisation of future trials (Torgerson & Byford, 2002).
CONCLUDING REMARKS
Stepped care models have potential to improve the efficiency of psychological therapy provision. However, the optimal content and organisation of stepped care is as yet unclear. Although there is some supportive evidence for the use of stepped care, rigorous evaluations of the underlying assumptions are scarce, and a significant research agenda remains. Modelling may be a useful research method in the shorter term.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Traditional models of the delivery of psychological therapy cannot meet current demand. Other forms of delivery, such as brief therapies, group treatments and self-help, may provide useful alternatives.
-
▪ Delivering alternative forms of psychological therapy through a stepped care model has significant potential to improve the efficiency of psychological therapy and ensure good outcomes for patients.
-
▪ There is only preliminary supportive evidence concerning stepped care systems in psychological therapies.
LIMITATIONS
-
▪ Crucial research questions remain to be addressed in relation to the clinical and economic assumptions underlying stepped care models.
-
▪ The acceptability of stepped care models to patients and professionals is unclear.
-
▪ The exact nature of the optimal stepped care model is also unclear, in terms of the number of steps, the treatments available at each step and the decision-making processes to determine when patients move between steps.




eLetters
No eLetters have been published for this article.