Dialectical behaviour therapy (DBT) is an evidence-based intensive treatment for borderline personality disorder and self-harm created by Linehan. In its original form it offers a year-long treatment consisting of 2-2.5 hours per week of group-based skills training, 1 hour a week of a one-to-one session, the opportunity for between-session crisis skills coaching and weekly peer supervision for the treatment team. Reference Linehan1,Reference Linehan2 Randomised controlled trials (RCTs) in the USA, The Netherlands and the UK have demonstrated that DBT is effective at helping people reduce self-harming behaviour. Reference Feigenbaum, Fonagy, Pilling, Jones, Wildgoose and Bebbington3-Reference Verheul, van den Bosch, Koeter, De Ridder, Stijnen and van den Brink9 The average treatment retention rate in non-UK-based studies was 67%. However, the UK-based RCTs comparing DBT with treatment as usual Reference Feigenbaum, Fonagy, Pilling, Jones, Wildgoose and Bebbington3,Reference Priebe, Bhatti, Barnicot, Bremmer, Gaglia and Katsakou10 demonstrated much higher treatment drop-out rates: 58 and 52%, whereas an earlier UK-based observational study reported an even higher drop-out rate of 67%. Reference Zinkler, Gaglia, Arokiadass and Farhy11 The McMain et al Reference McMain, Links, Gnam, Guimond, Cardish and Korman7 study of treatment as usual v. DBT in Canada also had a relatively high drop-out rate of 39%.
Previous studies on drop out and disengagement from mental health services identified associations with socioeconomic characteristics such as younger age, male gender, ethnic minority background, low socioeconomic status and social isolation. Reference Kreyenbuhl, Nossel and Dixon12,Reference O'Brien, Fahmy and Singh13 Those studies also linked clinical characteristics such as substance misuse, forensic history, high levels of psychopathology and lack of insight to higher drop-out rates. Some research has found poor alliance with the therapist as well as a lack of active participation in treatment by the patient to be correlated with drop out. Reference Priebe, Watts, Chase and Matanov14,Reference Young, Grusky, Jordan and Belin15 Drop out is more likely to occur during the early period of treatment. Reference Kreyenbuhl, Nossel and Dixon12,Reference O'Brien, Fahmy and Singh13 In contrast to those studies, Barnicot et al’s Reference Barnicot, Katsakou, Marougka and Priebe16 meta-analysis on drop out for patients with borderline personality disorder revealed that sociodemographic variables are consistently non-significantly associated with drop out for this group of patients, whereas lower commitment to change, a poorer therapeutic relationship, and higher impulsivity consistently predicted drop out. Other work has shown that patients with borderline personality disorder who perceive their treatment as less credible, do not use the skills taught in therapy, and have lower self-efficacy, and are also more likely to drop out of DBT (further details from K.B., on request).
McMain et al Reference McMain, Links, Gnam, Guimond, Cardish and Korman7 put down treatment context as a possible explanatory factor for their high drop-out rate - and specifically, the availability of other publicly funded treatment options - and Priebe et al Reference Priebe, Bhatti, Barnicot, Bremmer, Gaglia and Katsakou10 speculated that the National Health Service (NHS) context might lead to higher drop-out rates since alternative treatments or (crisis) management options are more easily available in the UK than in other settings, such as the healthcare system in the USA. Yet, no further research has been conducted to explore this. The current study examines the characteristics of patients dropping out from DBT in the UK and focuses on the question of whether being the recipient of care coordination under the care programme approach at the start of treatment leads to higher drop-out rates from DBT. A person with complex needs who is involved with multiple services (Social Services, mental health services, etc.) and who has a history of risky behaviour, such as suicide attempts or harm to others, may be appointed a key worker who monitors mental health symptoms and risk and coordinates care by meeting regularly with the individual. 17 In line with the suggestion of McMain et al, Reference McMain, Links, Gnam, Guimond, Cardish and Korman7 it may be possible that patients who have received care coordination will have learnt to rely on the care coordination system. Thus, they will be, first, more attuned to management of symptoms rather than change, which could lead to dissatisfaction with the change-oriented aspect of DBT, and second, aware that the care coordination system will be there for them as a ‘fallback’ should they drop out of therapy. To get a better understanding of the role of treatment context on drop out and because the link between care coordination and drop out from DBT has not been investigated yet, this study aims to address two questions:
-
1 What are the characteristics of patients dropping out from DBT?
-
2 How important is care coordination status to explain drop out from DBT?
Method
The study included data of 102 patients who were offered 1 year of DBT from a specialised team in the London Borough of Newham between 2008 and 2011; the drop-out rate for this group was 58%. Inclusion criteria for DBT were self-harming behaviour, defined as intentional tissue damage, on at least 5 days in the previous year, and a diagnosis of at least one personality disorder. Participants were all referred from either primary or secondary mental healthcare services.
To identify possible factors influencing drop out from DBT (measured as a binary variable: yes = 1; no = 0), a range of variables were selected based on predicators of outcome for borderline personality disorder identified in Gunderson et al’s study. Reference Gunderson, Daversa, Grilo, McGlashan, Zanarini and Shea18 Personality disorder as identified through SCID-II screening, Reference First, Gibbon, Spitzer, Williams and Benjamin19 a diagnosis of depression or post-traumatic stress disorder (PTSD; assessed through the Mini-International Neuropsychiatric Interview Reference Sheehan, Lecrubier, Sheehan, Amorim, Janavs and Weiller20 (MINI) are measured as binary variables (conditions identified: yes = 1; no = 0). History of hospitalisation, sectioning, substance misuse and psychotherapy were retrieved from patients’ medical histories and coded as ‘1’ if those factors were present and ‘0’ if absent. Trauma history was identified as a stated history of emotional, physical or sexual abuse and was also coded as a binary variable (yes = 1; no = 0). Time in secondary care prior to starting DBT is measured as the number of months in secondary care. Incidence of self-harm and intended suicide attempts are measured in number of attempts during the year prior to treatment commencement. Severity of mental health symptoms on the Brief Psychiatric Rating Scale (BPRS), Reference Ventura, Green, Shaner and Liberman21 the Brief Symptom Inventory Reference Derogatis and Melisaratos22 and Zanarini Reference Zanarini23 score for severity of borderline personality disorder symptoms at baseline are based on administered questionnaires.
Our main variable of interest was a history of care coordination. Two indicators of care coordination status were available from patients’ records. First, whether patients received care coordination some time in the past, and second, whether patients still received it at the beginning of treatment (a subset of the first group). Based on our hypothesis that care coordination may result in less commitment to change, we would expect only those patients that had care coordination at the time of treatment entry to be affected by higher drop-out rates. Hence, care coordination status at treatment commencement was used in this study and coded as a binary variable (yes = 1; no = 0). This choice was further supported by Fischer’s exact tests revealing that the drop-out rates of the 5 patients no longer in care coordination did not differ significantly from those of patients that never received care coordination (P = 1.000), whereas those 17 patients who did receive care coordination when entering DBT had significantly higher drop-out rates (P = 0.006), as almost 90% of this group dropped out. Although information on care coordinators or length of care coordination was not available, information on time in treatment was available for the majority of patients. Time in treatment was measured as the total number of contact hours.
Finally, a number of socioeconomic characteristics such as age, gender, ethnicity and employment status at baseline were also tested for their relationship to drop out. We then further compared the sociodemographic and clinical characteristics of patients with and without care coordination to get a better understanding of how the two groups may differ (detailed results available from the authors on request).
Statistical analysis
The association of each of those factors with drop out was first established using t-tests and χ2-tests. The results constituted the basis for building a multivariate logistic regression model in which all variables were included with a univariable association with drop out that was significant at the P<0.1 level. This included care coordination at the start of DBT treatment, a history of significant substance misuse, gender, and a diagnosis of obsessive-compulsive personality disorder (OCPD). To gain a better understanding of the impact of care coordination on the timing of drop out, Kaplan-Meier curves are provided for the two groups of patients.
Results
Over the 1 year studied, 59 patients dropped out of treatment. Table 1 shows the sociodemographic and clinical characteristics of the total sample, those who completed the treatment and those who dropped out, as well as the results of the statistical comparison of the groups.
Table 1 Descriptive statistics and univariate analysis of variables hypothesised to predict patient drop out from treatment

| % | Difference dropped out/completers χ2/t (P) |
|||
|---|---|---|---|---|
| Characteristics | All (n = 102) |
Dropped out (n = 59) |
Completers (n = 43) |
|
| Gender | 3.62 (0.06) | |||
| Male | 11.8 | 16.9 | 4.7 | |
| Female | 88.2 | 83.1 | 95.3 | |
| Age, years: mean | 32.4 | 32.8 | 31.9 | –0.43 (0.67) |
| Ethnicity | 2.10 (0.72) | |||
| White | 61.8 | 62.7 | 60.5 | |
| Black | 13.7 | 10.2 | 18.6 | |
| South Asian | 18.6 | 20.3 | 16.3 | |
| East Asian | 2.0 | 1.7 | 2.3 | |
| Mixed | 3.9 | 5.1 | 2.3 | |
| Employment | 0.79 (0.67) | |||
| Out of work | 62.7 | 64.4 | 60.5 | |
| Voluntary/sheltered | 8.8 | 10.2 | 7.0 | |
| Regular | 28.4 | 25.4 | 32.6 | |
| Living situation | 0.20 (0.65) | |||
| Living alone | 32.7 | 35.5 | 30.2 | |
| With partner/family | 67.3 | 65.5 | 69.8 | |
| History of:Footnote a | ||||
| Care coordination | 16.7 | 25.4 | 4.7 | 7.73 (<0.01) |
| Hospitalisation | 43.1 | 47.5 | 37.2 | 1.07 (0.30) |
| Sectioning | 9.8 | 7.0 | 11.9 | 0.67 (0.41) |
| Psychotherapy | 62.8 | 67.8 | 53.5 | 2.16 (0.14) |
| Trauma (emotional, physical or sexual abuse) | 89.2 | 91.5 | 86.1 | 0.78 (0.38) |
| Significant substance misuse | 29.4 | 37.3 | 18.6 | 4.18 (0.04) |
| Diagnosis of personality disorder (SCID-II)Footnote a | ||||
| Avoidant | 62.8 | 67.8 | 55.8 | 1.53 (0.22) |
| Dependent | 23.5 | 25.3 | 20.9 | 0.28 (0.60) |
| Obsessive-compulsive | 46.1 | 39.0 | 55.8 | 2.84 (0.09) |
| Paranoid | 49.0 | 50.9 | 46.5 | 0.19 (0.67) |
| Schizotypal | 14.7 | 15.3 | 14.0 | 0.03 (0.86) |
| Schizoid | 6.9 | 6.8 | 7.0 | 0.00 (0.97) |
| Histrionic | 2.0 | 1.7 | 2.3 | 0.05 (0.82) |
| Narcissistic | 12.8 | 13.6 | 11.6 | 0.08 (0.77) |
| Borderline | 99.0 | 100.0 | 97.7 | 1.39 (0.24) |
| Antisocial | 19.6 | 23.7 | 14.0 | 1.51 (0.22) |
| Depression (MINI)Footnote a | 76.5 | 80.0 | 72.1 | 0.79 (0.37) |
| Post-traumatic stress disorder | 53.9 | 54.2 | 53.5 | 0.01 (0.94) |
| Time in secondary care before DBT, months: mean | 21.4 | 24.4 | 17.4 | –1.55 (0.12) |
| Baseline tests, mean | ||||
| Incidence of self-harmFootnote b | 85.0 | 75.7 | 97.6 | 0.97 (0.34) |
| Suicide attemptsFootnote b | 2.3 | 3.0 | 1.4 | –1.37 (0.18) |
| ZanariniFootnote c | 17.3 | 17.4 | 17.2 | –0.11 (0.91) |
| BPRSFootnote c | 51.2 | 50.5 | 52.3 | 1.08 (0.28) |
| BSIFootnote c | 124.4 | 124.9 | 123.3 | –0.14 (0.89) |
BPRS, Brief Psychiatric Rating Scale; BSI, Brief Symptom Inventory; DBT, dialectical behaviour therapy; MINI, Mini-International Nueropsychiatric Interview. Values in bold are χ2 as opposed to t-values.
a. Measured as binary variables (yes = 1; no = 0).
b. Number of attempts during year prior to the start of treatment.
c. Based on administered questionnaires.
Table 1 reveals that men tended to drop out of treatment more often, whereas patients with OCPD were more likely to complete treatment (trend). The two groups showed statistically significant differences with respect to a history of care coordination and of substance misuse: 88% (n = 15) of patients who received care coordination at the start of treatment (n = 17) dropped out as compared with 52% (n = 44) of those without such a history (n = 85) (χ2 = 7.73, P⩽0.01). Drop-out rates for patients who had received care coordination in the past, but have no longer done so at the beginning of DBT treatment did not differ significantly from those that had never received care coordination and were thus not classified as ‘care coordinated’. Only those patients who still had care coordination at the start of treatment were classified as such. Regarding history of substance misuse, 73% (n = 22) of patients with a history of substance misuse (n = 30) dropped out as compared with 51% (n = 37) of patients without (n = 72) (χ2 = 4.18, P = 0.04). Of patients diagnosed with OCPD (n = 47), 49% (n = 23) dropped out as compared with 65% (n = 36) of those who did not have that diagnosis (n = 55). Patients receiving care coordination were more likely to be hospitalised (χ2 = 21.62, P<0.01) and sectioned (χ2 = 8.87, P<0.01) in the past, spent twice as many days in secondary care (t = –3.25, P<0.01) and were six times more likely to attempt suicide (t = –3.18, P<0.01). Care coordination was not related to any sociodemographic characteristics or diagnoses (SCID-II), but patients who received it had lower Zanarini scores for symptom severity of borderline personality disorder at baseline (t = 1.78, P = 0.08). Care coordination is thus associated with a number of variables indicating risky behaviour and tends to include patients with lower symptom severity of borderline personality disorder.
Table 2 reports the results of the multivariate logistic regression analysis ((pseudo) R 2 = 0.11; model χ2(4) = 15.51) revealing that care coordination history was the only predictor variable to remain statistically significant (B = 1.77; P = 0.03; odds ratio (OR) = 5.86), whereas substance misuse history (B = 0.77; P = 0.14; OR = 2.16), gender (B = –1.03; P = 0.23; OR = 0.36) and OCPD (B = –0.50; P = 0.26; OR = 0.61) were no longer statistically significant. The results indicate that the odds of a patient who receives care coordination dropping out are 5.86 times higher than the odds of a patient who does not receive it.
Table 2 Relationship between drop out, care coordination status, substance misuse history, gender and OCPD diagnosis: results from logistic regression

| Drop outFootnote a | ||
|---|---|---|
| Variables | Parameter estimates (P) |
Odds ratio (95% CI) |
| Constant | 2.08 (0.22) | - |
| Care coordinationFootnote a | 1.77 (0.03) | 5.86 (1.22-28.17) |
| Significant substance misuseFootnote a | 0.77 (0.14) | 2.16 (0.78-5.97) |
| GenderFootnote b | –1.03 (0.23) | 0.36 (0.07-1.93) |
| OCPDFootnote a | –0.50 (0.26) | 0.61 (0.26-1.43) |
| Log likelihood | –61.68 | |
| Model χ2 (d.f.) | 15.51 (4) | |
| P = 0.004 | ||
| N | 102 | |
OCPD, obsessive-compulsive personality disorder.
a. Binary variables: yes = 1, no = 0.
b. Male = 1, female = 2.
To get a better understanding of how care coordination affects the pattern of drop out, Fig. 1 depicts the Kaplan-Meier survival curves by care coordination status. Although both groups experience fast rates of drop out during the early stages of treatment (probability to remain in treatment for each group is 80% after 5 hours, including 2 hours of assessment), drop out occurs at a much more rapid pace for the ‘care coordinated’ group at between 5 and 11 hours of treatment. At 9 treatment hours, the probability to remain in treatment drops to 53% for patients receiving care coordination compared with 80% for the group who do not. At 11 hours, probabilities drop to 33.3% and 78% respectively.
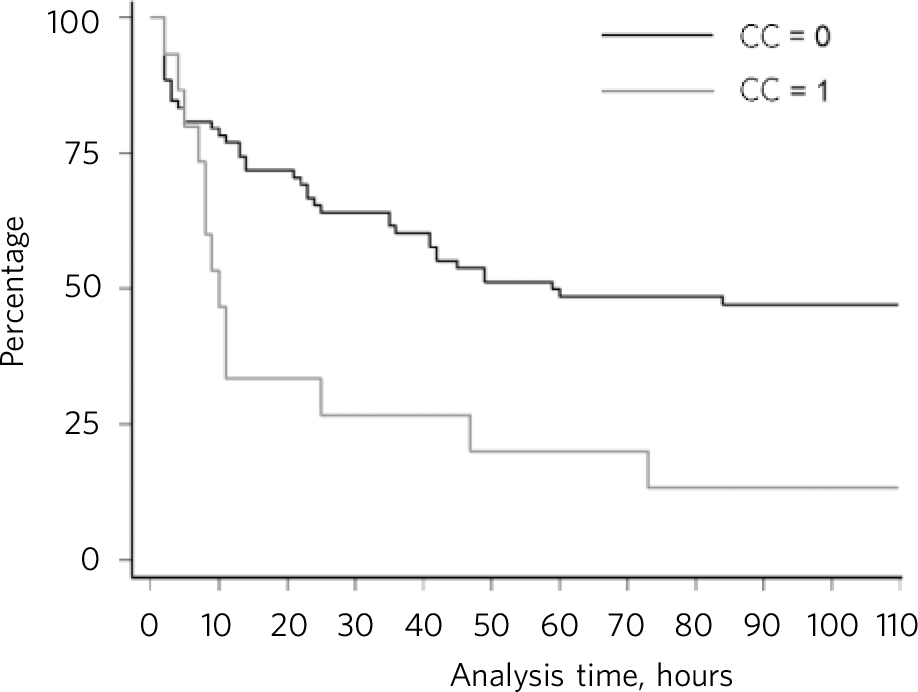
Fig 1 Kaplan-Meier survival curves by care coordination status. CC, care coordination (yes = 1, no = 0).
Discussion
Historically, people with borderline personality disorder were reported to have low treatment completion rates, particularly in psychological therapies that were not tailored to treating the disorder, with one study reporting an 8% completion rate. Reference Budman, Demby, Soldz and Merry24 In the past two decades, however, treatments have been created specifically for borderline personality disorder. Average treatment completion rates for these treatments (DBT, mentalisation-based therapy, transference-focused psychotherapy) are 71-75%. Reference Barnicot, Katsakou, Marougka and Priebe16 However, as reported earlier, the much lower completion rates in several more recent studies conducted in the UK are inconsistent with this.
A high drop-out rate affects patients and service providers alike. For patients, it may mean increased hopelessness, frustration and perhaps even a sense of one’s illness being untreatable. High drop-out rates also negatively affect service providers and are disheartening to therapists who are trained in specific models of treatment, particularly in DBT, which has as one of its goals keeping people in treatment. Reference Linehan1
This study is consistent with other results on treatment drop out for patients with borderline personality disorder and reveals that sociodemographic characteristics, with the exception of gender, are not associated with drop out (see O’Brien et al Reference O'Brien, Fahmy and Singh13 and Table 1). A history of care coordination was a significant predictor of drop out in this sample and the predictive association was not explained by the influence of other sociodemographic and clinical variables tested. Although drop-out rates tend to be higher during the early stages of treatment for all patients, the analysis revealed that they increased much more rapidly for patients receiving care coordination during the early treatment period. Care coordination is arguably more oriented towards helping patients manage rather than treat or change the mental health symptoms and can provide the experience of comprehensive and always available care.
The predictive value of the history of care coordination in this study might explain the difference in drop-out rates between studies in the USA and the UK, because the treatment-as-usual condition is different in the USA. Not taking up an offer of DBT in the USA often means not having any service. Although case management does exist in the USA, it is not as readily available as it is in the UK and there is no safety net of a universal healthcare system that will always provide some level of care. McMain et al Reference McMain, Links, Gnam, Guimond, Cardish and Korman7 raised a similar issue when discussing the relatively high treatment drop-out rate found in their study of DBT v. treatment as usual in the Canadian healthcare context, where they stated that they believed high drop out might have something to do with the availability of ‘quality’ publicly funded alternatives to DBT.
Thus, with such a stark drop-out rate related at least in part to care coordination, we are left with the question of whether care coordination, as it is currently delivered, helps or hinders people with borderline personality disorder. More research is needed into the effects of care coordination as the risk issues associated with people with borderline personality disorder and at times the chaotic social situations that many with borderline personality disorder find themselves in are often managed through care coordination. Further research may also consider whether DBT could be adapted for the NHS context to more effectively address any effects of a history of care coordination. For example, it might be possible to develop or modify DBT treatment preparation done by care coordinators and DBT therapists to specifically ameliorate any unintended deleterious effects of care coordination. It is also possible that DBT’s strict attendance rules may not be as effective in the NHS context as they were in the USA, but more research on DBT in the NHS would be needed to establish this.
The strengths of the study are that we considered a wide range of sociodemographic and clinical variables as potential predictors. Limitations are that the predominantly female gender mix was not ideal to test the influence of gender, and that the sample size was not very large, although still substantial for this type of research. Reference Linehan1 The most significant limitation of this study is the lack of detailed quantitative and qualitative information about the care coordination experience. No information about the care coordinators, the nature of the care coordination process (i.e. frequency of contact or issues covered in the contact) and the length of time patients were receiving care coordination as well as a lack of explicit information on patient-stated reasons for dropping out from DBT limits the interpretation of the role of care coordination for DBT drop out.
Data on DBT in the NHS consistently report higher drop-out rates than in the US-based studies. However, the drop-out rate among patients without a history of care coordination in our study was still high at 52%. One can only speculate as to whether, and if so, to what extent, the availability of alternative management/treatments has contributed to dropping out in this group, too. Although these patients have not experienced care coordination themselves, many of them will have been aware of additional treatment options in primary and secondary care. The statistical relationship between care coordination and DBT drop out flags up an important area for future research, including more detailed quantitative and qualitative work to investigate the role of care coordination in patients’ behaviour and whether they have learnt to rely on care coordination system, and thus, (1) will be more attuned with the management of symptoms rather than change, or (2) will be aware that the care coordination system will be there as a ‘fallback’ option if they drop out of treatment. Once we establish the exact link between care coordination and drop out, further research should also explore how DBT can be modified to increase retention rates in the NHS, particularly for patients with a history of care coordination, and possibly develop more appropriate interventions for this patient group as a whole.






eLetters
No eLetters have been published for this article.