Periodic alternating nystagmus (PAN) refers to a conjugate horizontal nystagmus that periodically reverses its direction. Acquired PAN has been reported occasionally after visual loss and mostly in cerebellar disorders.Reference Furman, Wall and Pang1 Lesions involving the cerebellar nodulus/uvula has been considered responsible for PAN. In monkeys, selective ablation of the nodulus/uvula produces PAN. In humans, PAN has been described in focal lesions involving the cerebellar nodulus.Reference Jeong, Oh, Kim, Kim, Lee and Oh2 While PAN usually has a periodicity of alternating horizontal nystagmus with approximately every 90–120 s, spontaneously alternating nystagmus without a periodicity has also been described in vertebrobasilar insufficiency, cervical whiplash injury, and Meniere’s disease,Reference Nuti, Ciacci, Giannini, Rossi and Federico3, Reference Murofushi, Chihara, Ushio and Iwasaki4 but the mechanisms of those aperiodic alternating nystagmus are largely unknown. This study describes two patients with aperiodic alternating nystagmus from strokes restricted to the lateral medulla, which allowed speculation on the mechanism of alternating nystagmus.
A 64-year-old man with hypertension developed sudden vertigo and imbalance. Neurological examination 16 days after the symptom onset found normal visual acuity in both eyes, ptosis of the right eye, and square-wave jerks with visual fixation. Without visual fixation in darkness, small horizontal nystagmus irregularly alternated its direction, in conjunction with upbeat component (Figure 1(A) and (B)). He had horizontal gaze-evoked nystagmus greater in the leftward gaze, rightward hypermetric and leftward hypometric saccades, and right-beating head-shaking nystagmus. In addition, he showed veering to the right while walking and ataxia of the right upper extremity. Video head impulse tests (HITs) were normal. Ocular torsion and subjective visual vertical were within normal ranges. Brain MRIs showed a hemorrhagic lesion restricted to the right lateral medulla (Figure 1(C)).
Figure 1: Patient 1 (A) The patient 1 shows mostly square-wave jerks with visual fixation, but small horizontal nystagmus that irregularly alternates its direction in darkness. (B) Plotting the slow phase velocity of the nystagmus (arrowed in A) documents alternating horizontal nystagmus. (C) Brain MRI of the patient 1 shows a focal hemorrhagic lesion restricted to the right lateral medulla. LH, horizontal position of the left eye; LV, vertical position of the left eye. Upward deflection indicates rightward and upward eye motion.
A 50-year-old woman developed acute vertigo, headache, and binocular horizontal diplopia. Examination 11 days after the symptom onset found right ptosis and miosis, consistent with right Horner’s syndrome. She showed esophoria, rightward head tilt, and rightward deviation of the eyes during eye closure, which was evidenced by corrective leftward centripetal eye movements on eye opening. Her ocular motor ranges were full, and visual acuity was normal. Oculography documented spontaneous nystagmus beating leftward, upward, and counterclockwise with a decreasing slow phase velocity in light, which changed its horizontal direction at irregular intervals in darkness (Figure 2(A) and (B)). She had gaze-evoked nystagmus greater in the leftward gaze, rightward hypermetric and leftward hypometric saccades, and right-beating head-shaking nystagmus. In addition, she showed hypoesthesia of the right face and left-side extremities, and rightward veering on standing and attempted gait. Video HITs were normal. During caloric tests, vestibular hyperreflexia was found with impaired visual suppression. Ocular torsion was normal, but subjective visual vertical was tilted to the right (13.5°, normal: −2.4–2.6°). Brain MRIs showed an infarction in the right lateral medulla (Figure 2(C)).
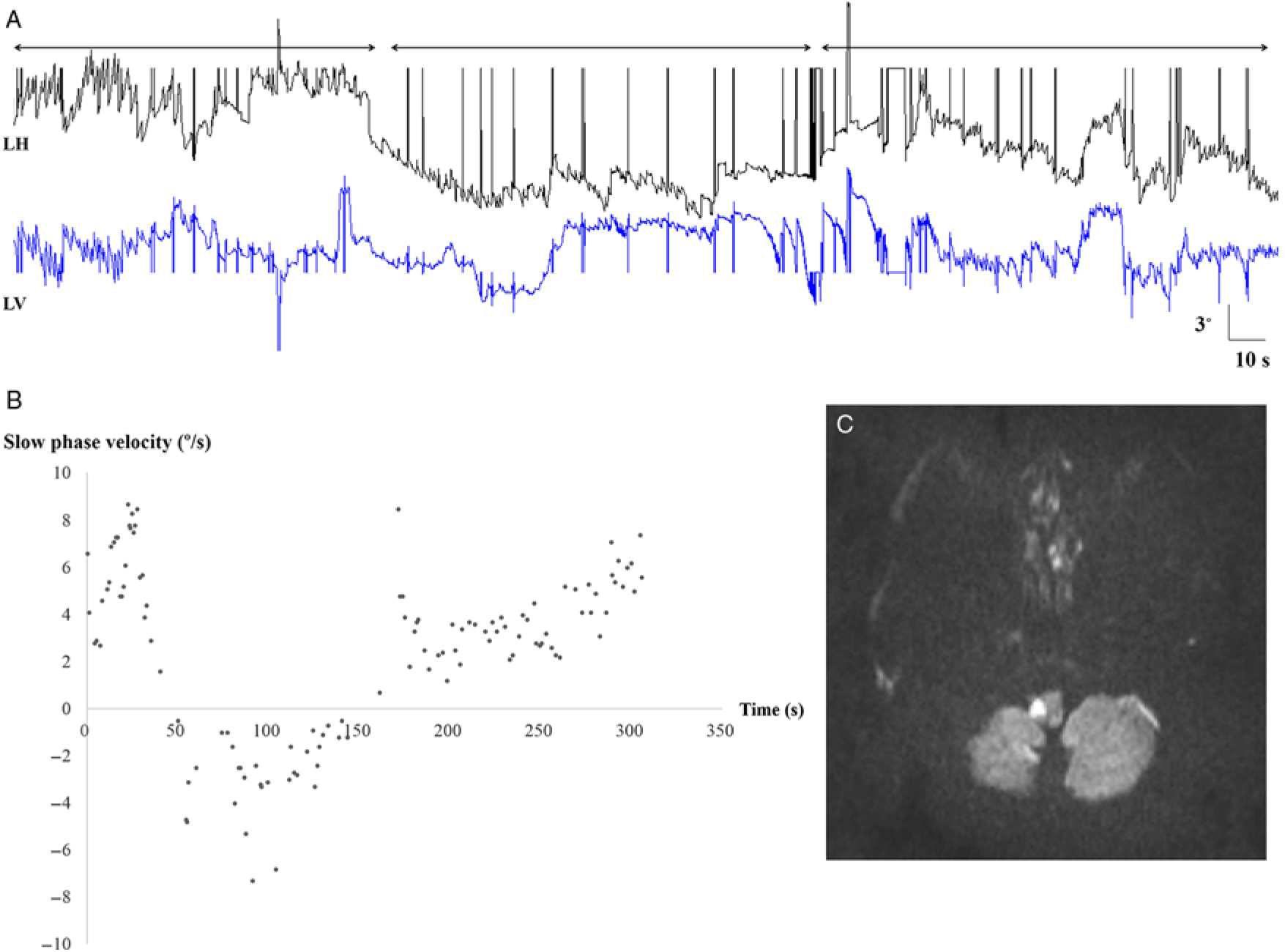
Figure 2: Patient 2 (A) Video oculography shows spontaneous nystagmus beating leftward and upward that changes its horizontal direction at irregular intervals in darkness. (B) Plotting the slow phase velocity of horizontal nystagmus (arrowed in A) demonstrates alternating directions. (C) Brain MRI shows an infarction restricted to right lateral medulla. LH, horizontal position of the left eye; LV, vertical position of the left eye. Upward deflection indicates rightward and upward eye motion.
Both patients showed aperiodic alternating spontaneous nystagmus from strokes restricted to the dorsolateral medulla. The localization of lesions to the dorsolateral medulla is also supported by the associated ocular motor findings of ipsilesional Horner’s syndrome, ipsiversive ocular tilt reaction, ocular ipsipulsion, and ipsilesional head-shaking nystagmus in association with crossed sensory changes, ipsilesional limb ataxia and ipsiversive falling. In lateral medullary lesions, the neural substrate for each ocular motor finding has been well established: the oculosympathetic fibers for Horner’s syndrome, olivocerebellar fibers for ocular lateropulsion, Reference Meyer, Baloh, Krohel and Hepler5 ascending vestibular tracts for the ocular tilt reaction, and nodulouvular inhibitory fibers for ipsilesional head-shaking nystagmus.Reference Choi, Oh, Park, Kim, Koo and Kim6 However, aperiodic alternating spontaneous nystagmus has not been reported in a unilateral medullary lesion. In the acute dorsolateral medullary infarction, spontaneous nystagmus is often observed with a various combination of horizontal, vertical and torsional components. Later, patients may show a reversal in the direction of spontaneous nystagmus. However, alternating spontaneous horizontal nystagmus has not been described in unilateral lateral medullary strokes. Given that the time constant of the vestibulo-ocular reflex is three times larger than that of the cupula, the velocity storage mechanism has been postulated to act in the central neural system. This velocity storage is assumed to be mediated by the vestibular nuclei and their commissural fibers.Reference Leigh, Robinson and Zee7 The Purkinje cells in the cerebellar nodulus and ventral uvula project to the ipsilateral vestibular nuclei. Acquired PAN has been explained by defective cerebellar inhibitory control over the velocity storage.Reference Leigh, Robinson and Zee7 This disinhibition would result in inappropriately prolonged vestibular responses and lead to the action of repair mechanism to periodically reverse the direction of the vestibular eye movements.Reference Leigh, Robinson and Zee7
The velocity storage mechanism is also important for head-shaking nystagmus. Ipsilesional head-shaking nystagmus in unilateral lateral medullary lesions is attributed to asymmetric velocity storage due to unilateral damage to the nodulouvular inhibitory.Reference Choi, Oh, Park, Kim, Koo and Kim6 While acquired PAN has mostly been found in cerebellar disorders such as spinocerebellar degeneration, Chiari malformation, and ischemic lesions involving the midline cerebellar structure,Reference Jeong, Oh, Kim, Kim, Lee and Oh2, Reference Leigh, Robinson and Zee7 our patients support a role of disruption of unilateral nodulouvular inhibitory pathway at the brainstem for spontaneously alternating nystagmus. The gaze-evoked nystagmus in our patients is suggestive of an injury of the horizontal neural integrator that includes the medial vestibular nucleus. In contrast to a lesion involving the cerebellar nodulus/uvula that would affect the inhibitory pathway alone, lateral medullary lesions are more likely to damage the vestibular nuclei as well as the nodulouvular inhibitory projections. Therefore, even if the cerebellar inhibitory signals are interrupted in lateral medullary strokes, simultaneous damage of the vestibular nucleus may disturb perseveration of the transduced vestibular signals. Since the vestibular storage leading to the prolonged vestibular responses requires the functioning vestibular nuclei as the raw vestibular velocity repository and amplifier, impairment of the vestibular nuclear function, if any, should have been partial in our patients with alternating nystagmus. The normal HITs in the presence of gaze-evoked nystagmus in our patients suggested a partially injured vestibular nucleus, given that a lesion involving unilateral medial vestibular nucleus gave rise to decreased head impulse vestibulo-ocular reflex gains, more to the lesion side, and gaze-evoked nystagmus, greater during contralesional gaze.Reference Kim, Zee, du Lac, Kim and Kim8 While the typical PAN was caused by the nodulouvular injury combined with the intact vestibular nuclei, the nodulouvular disinhibition with the partially damaged vestibular nucleus in lateral medullary strokes may produce relatively short and irregular cycles of alternating nystagmus.
Statement of Authorship
SHK designed the study, interpreted and analyzed the data, and drafted the manuscript. JSK designed the study, interpreted the data, and made critical revisions of the manuscript.
Conflicts of Interest
The authors declare that they have no conflicts of interest.



