1. Introduction
Studies applying an experience sampling method (ESM) have found that individuals with psychosis and those at risk show elevated self-reported negative affect in response to daily hassles, which is commonly referred to as “stress-sensitivity” or “stress-reactivity” [Reference Myin-Germeys and van Os1]. Moreover, ESM studies find self-reported daily stress to be associated with psychotic symptoms in clinical and non-clinical samples [Reference Lataster, Wichers, Jacobs, Mengelers, Derom and Thiery2–Reference Thewissen, Bentall, Oorschot, Campo, van Lierop and van Os6], and in the most recent study, Van Der Steen et al. [Reference Van Der Steen, Gimpel-Drees, Lataster, Viechtbauer, Simons and Lardinois7] found that this association is even larger in high risk groups than in patients. Daily stress thus appears to be especially relevant to the development of psychotic symptoms even before the unfolding of the full disorder. However, several issues require further clarification.
One of these issues is related to the operationalization of stress. Researchers using experimental designs to investigate stress-reactivity have widely acknowledged the importance to assess both physiological and psychological parameters of stress [Reference Allen, Kennedy, Cryan, Dinan and Clarke8] in order to gain a fuller understanding of the processes involved. In contrast, most ESM studies are limited to self-reported stress. In one of few ESM studies in the field of psychosis that investigated the activation of the autonomous nervous system (ANS) as a physiological marker of stress, Kimhy and colleagues [Reference Kimhy, Delespaul, Ahn, Cai, Shikhman and Lieberman9] found no evidence for an association between self-reported stress and heart rate. They did, however, find self-reported stress to be associated with other ANS parameters, such as sympathovagal balance. Another ESM study found acute psychosis patients to have an increased heart rate and an altered autonomic variation in comparison to healthy controls [Reference Boettger, Hoyer, Falkenhahn, Kaatz, Yeragani and Bär10]. These studies show alterations in physiological stress in the context of daily life in patients with psychosis. They also indicate that physiological stress parameters capture different aspects of stress than self-report. To further corroborate this notion and better understand the link between stress and symptom formation, research on the association between physiological stress, self-reported stress, and psychotic symptoms within a daily life context is required.
Another issue related to the association between daily stress and psychotic symptoms refers to its temporality. So far, there is only limited evidence for the assumption that stress precedes (rather than follows from) psychotic symptoms [Reference Ben-Zeev, Ellington, Swendsen and Granholm11, Reference Kramer, Simons, Wigman, Collip, Jacobs and Derom12]. Moreover, few ESM studies have aimed to investigate the reversed pathway in which psychotic symptoms trigger stress [Reference Van Der Steen, Gimpel-Drees, Lataster, Viechtbauer, Simons and Lardinois7, Reference Armando, Nelson, Yung, Ross, Birchwood and Girardi13, Reference Peters, Lataster, Greenwood, Kuipers, Scott and Williams14]. This is surprising as – considering the literature on the distress related to psychotic symptoms [Reference Armando, Nelson, Yung, Ross, Birchwood and Girardi13, Reference Yung, Buckby, Cotton, Cosgrave, Killackey and Stanford15] – a vicious circle, in which stress and symptoms are driving each other can be expected.
Finally, given that we can corroborate the assumption that stress predicts an exacerbation of psychotic symptoms in the earliest stage of disorder formation, the question arises whether we can identify specific factors that make people vulnerable to developing psychotic symptoms in the face of stress. Recent research suggests that deficits in emotion regulation (ER) could constitute a crucial vulnerability factor [Reference Aldao, Nolen-Hoeksema and Schweizer16, Reference Garnefski and Kraaij17]. Compared to healthy controls, individuals with psychosis use more maladaptive and less adaptive ER [Reference Kimhy, Vakhrusheva, Jobson-Ahmed, Tarrier, Malaspina and Gross18–Reference van der Meer, van’t Wout and Aleman22]. Furthermore, ER seems to be related to physiological and self-reported stress [Reference Clamor, Schlier, Köther, Hartmann, Moritz and Lincoln23, Reference Lincoln, Hartmann, Köther and Moritz24]. In a laboratory experimental study, Lincoln et al. [Reference Lincoln, Hartmann, Köther and Moritz24] found adaptive ER to moderate the association between induced stress and paranoid symptoms, indicating that ER could be a protective factor that prevents stress from translating into paranoid symptoms. However, this assumption needs further corroboration by testing to which extent the habitual use of adaptive or maladaptive ER skills makes people vulnerable to responding to stress with psychotic symptoms in daily life.
Building upon the solid evidence showing that self-reported stress is associated with paranoid symptoms in daily life, the goal of this study was to investigate the temporality of the association between self-reported stress, physiological stress and paranoid experiences, and to identify the moderating value of ER. We expected that self-reported and physiological stress would predict the subsequent report of paranoia over the course of a day. Furthermore, we expected that paranoia would in turn predict the intensity of subsequent self-reported and physiological stress. Finally, we hypothesized that the habitual use of adaptive and maladaptive ER would moderate the path from daily stress to paranoia. Building on the continuum of psychotic symptoms and their associated risk factors [Reference Van Os and Linscott25], we used a community sample with elevated levels of psychotic-like experiences in order to gain insight into the development of subclinical symptoms prior to the full unfolding of the disorder.
2. Methods and materials
2.1. Participants
Participants from previous studies who had consented to be contacted for future projects and first semester psychology students were prescreened for the occurrence of psychotic-like experiences as measured by the Community Assessment for Psychotic Experiences (CAPE) [Reference Stefanis, Hanssen, Smirnis, Avramopoulos, Evdokimidis and Stefanis26]. Potential participants were invited to participate starting from those with highest value and ending with score of eight on the positive syndrome subscale of CAPE, which corresponds to the score of 50th percentile of the large community sample published in Schlier et al. [Reference Schlier, Jaya, Moritz and Lincoln27]. The acquired sample consisted of 67 individuals (71.6% female, M age = 23.01, SD age = 4.63). Nine participants reported to have been given a diagnosis of a mental disorder in the past, and 18 participants reported a mental disorder of a family member. The majority of participants (80.6%) were students; 47.8% reported to be working six or more hours per week. Most participants (83.6%) were German nationals. All participants provided written informed consent and were compensated with 10€ per hour or granted credit points.
2.2. Procedure
Baseline assessment took place at Universität Hamburg in Germany. First, an electrocardiogram (ECG) sensor was attached to the participants’ chest and activated. The participants then completed paper-pencil questionnaires. Thereafter, they received Android smartphones that allowed the use of the movisensXS ESM application (Movisens GmbH) only. After activating the application, the participants left the laboratory and the ESM assessment phase began. As can be seen in Fig. 1a, the ECG recorded arousal continuously over 24 h. The smartphones were programmed to beep in approximately 20-min-intervals (between 9 AM and 10 PM) resulting in 38 samples over 24 h. The starting and ending time-point of the ESM assessment phase varied across participants, but no participant was subject to any assessments between 10 PM and 9 AM. Participants were instructed to behave as usual, with the restriction that they were not allowed to take a shower or exercise excessively. Fig. 1b illustrates the time references between any two ESM questionnaires. As can be seen, after the beep at any given time-point (t), participants answered questions regarding their stress level since the previous beep (thus for the time-period between t-1 and t). Furthermore, participants answered questions on momentary paranoid symptoms referring to the time-point t.
2.3. Assessment
2.3.1. Psychosis proneness assessment
Psychosis proneness was assessed with the CAPE [Reference Stefanis, Hanssen, Smirnis, Avramopoulos, Evdokimidis and Stefanis26] that captures lifetime psychotic-like experiences. The CAPE is a self-report questionnaire composed of the depressive, negative, and positive syndrome subscales. The scale is constructed with 42 items to be self-rated on a four-point Likert scales ranging from 0 = “never” to 3 = “nearly always”. The CAPE has been found to be a valid and reliable measure of psychosis proneness [Reference Konings, Bak, Hanssen, Van Os and Krabbendam28] and to be sensitive in detecting individuals at ultra-high risk for psychosis [Reference Mossaheb, Becker, Schaefer, Klier, Schloegelhofer and Papageorgiou29]. The German version of the CAPE has good to excellent internal consistency [Reference Schlier, Jaya, Moritz and Lincoln27].
2.3.2. Emotion regulation assessment
2.3.2.1. Adaptive ER.
In order to capture the comprehensive spectrum of strategies, adaptive ER was measured with a composite score derived from two questionnaires – German version of the emotion specific Emotion Regulation Skills Questionnaire (ERSQ-ES) [Reference Ebert, Christ and Berking30] and the adaptive subscale of the German version of the Cognitive Emotion Regulation Questionnaire (CERQ) [Reference Loch, Hiller and Witthöft31]. The ERSQ-ES assesses the following adaptive strategies: clarity, understanding, acceptance, tolerance, self-support, willingness to confront situations cuing undesired emotions when necessary to attain personally relevant goals, and modification. The ERSQ-ES measures the use of strategies differentially for stress, anxiety, anger, sadness and shame. The total score used for this study was the mean score of all items relative to the number of emotions. The psychometric properties of the ERSQ-ES were good to excellent in large clinical and non-clinical samples [Reference Ebert, Christ and Berking30]. The following additional adaptive strategies were assessed with the CERQ: acceptance, positive refocusing, refocusing on planning, positive reappraisal and putting into perspective. The German version of the CERQ has acceptable to good psychometric properties [Reference Loch, Hiller and Witthöft31]. The internal consistency of the composite adaptive ER scale consisting of the ERSQ-ES total mean score and CERQ adaptive ER subscale mean score was excellent on our sample, with Cronbach’s α = 0.92.
2.3.2.2. Maladaptive ER.
Maladaptive ER was assessed with the mean score on the maladaptive ER subscale of CERQ, which includes the strategies self-blame, catastrophizing, rumination/focus on thought, and blaming others. The maladaptive strategies subscale in our sample showed an acceptable internal consistency with Cronbach’s Alpha = 0.703.
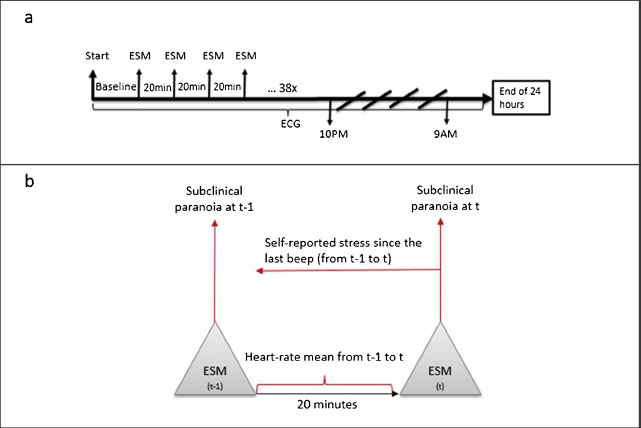
Fig. 1 Study procedure (1a) and time reference between any two experience sampling time-points (1b). ESM, Experience Sampling Method; t, time-point; t-1, time-point preceding.
2.3.3. Assessment of momentary physiological stress
Physiological arousal was measured as heart rate per minute using a sensor (Movisens ECGmove) designed for collecting ambulatory ECG. ECGmove is a small 62.3 × 38.6 × 11.5 mm sensor attached to electrodes that were placed on the left side of the chest. As presented in Fig. 1, heart rate was measured continuously and was subsequently analyzed as a mean heart rate between two beeps. The correction of artefacts that can emerge from physical activity during assessment or from the disturbances in electrode connection was performed automatically in DataAnalyzer (Movisens GmbH).
2.3.4. Assessment of momentary self-reported stress
The self-reported stress was assessed with 10 items referring to the previous 20 min (between t-1 and t, see Fig. 1b) rated on a 10-point scale. The scale included self-ratings of arousal, stress and control (subscale based on Gaab et al. [Reference Gaab, Rohleder, Nater and Ehlert32]: “The situation was stressing me”; I was able to control the situation”; I was calm and relaxed”; “I was helpless in the situation”) as well as self-ratings of fear, sadness, anger, shame, guilt, and (un-)happiness (subscale based on Stemmler et al. [Reference Stemmler, Heldmann, Pauls and Scherer33]). The pre-analysis showed that two subscales loaded on a common factor so that the score was computed as the mean of the 10 items at each time-point. Geldof, Preacher and Zyphur [Reference Geldhof, Preacher and Zyphur34] propose to conduct the multilevel analysis of reliability when dealing with hierarchical data, since the single level Cronbach’s α yields untrusty parameters due to the confounding variance of the two measurement levels (between and within). For the momentary self-reported stress the within-subject-level internal consistency was acceptable to good with Cronbach’s α = 0.82 and good for the between-subject-level with Cronbach’s α = 0.88.
2.3.5. Assessment of momentary paranoia
Momentary subclinical paranoia was assessed with a three item version of the Paranoia Checklist containing items identified as sensitive to change in previous studies: “I need to be on my guard against others”; “Strangers and friends look at me critically”; and “People try to upset me” [Reference Schlier, Moritz and Lincoln35]. Participants were asked to which extent each of the statements applies to them at the moment of the beep (time-point t, see Fig. 1b) on a 10-point scale. The scores used were the mean scores of the three items at each time-point. The multilevel reliability was questionable to poor for the within-subject-level (Cronbach’s α = 0.62), and excellent for the between-subject-level (Cronbach’s α = 0.92).
2.4. Statistical analysis
Data was analyzed using IBM SPSS Statistics software (version 22) and R. First, correlations were computed between self-reported stress and heart rate. Second, in order to account for the hierarchical design of the study we applied multilevel analysis. As suggested in literature [Reference Wang and Maxwell36], independent variables that were repeated measures were centered around the subject-mean and baseline independent variables were grand-mean centered. The time-point was included as a control variable in all models. To test whether preceding stress (at time-point between t and t-1) predicted subsequent paranoia (at time-point t) we calculated linear mixed-effect models (Package ‘lme4′ for R) with random intercept and random slope. The same analysis was done in order to test the reversed causation (preceding paranoia at time-point t-1 predicting subsequent stress at the time-point between t-1 and t). In the final model, we entered the adaptive and maladaptive ER as moderators. As proposed by Singer and Willet [Reference Singer and Willett37] we calculated pseudo-R2 statistic as an indicator of the effect size and classified these as small, medium or large [Reference Cohen38]. The pseudo-R 2 statistic expresses the proportion of variance explained between and within persons in comparison to the null model.
3. Results
3.1. Descriptive statistics
The sum scores and standard deviations of the psychotic experiences measured with the CAPE, ER mean scores at baseline, as well as the ESM scores of self-reported stress, heart rate and paranoia symptoms are presented in Table 1. Regarding psychosis-proneness measured by CAPE, the mean sum-score on CAPE positive syndrome subscale in our sample with M = 16.16 was higher than the mean sum-score found in psychosis samples (M = 14.50) in Schlier et al. [Reference Schlier, Jaya, Moritz and Lincoln27]. Specifically, all participants indicated to experience no less than one symptom of each CAPE subscale at least “sometimes”. All participants indicated to experience at least one positive symptom “often” and 32% of participants indicated to experience at least one positive symptom “nearly always”. The compliance rate for the ESM assessment was 81% in average, ranging from 8 to 100%, which is comparable with compliance rates usually found in ESM studies [Reference Silvia, Kwapil, Eddington and Brown39]. Only four participants had a compliance rate for the ESM assessments of less than 50%. Excluding these from the analysis under assumption of “non-random missing” did not alter the results, so that all participants were included in all subsequent analyses. Four percent of heart rate data points were missing due to technical issues.
Table 1 Mean, standard deviation and range of baseline and experience sampling method variables.

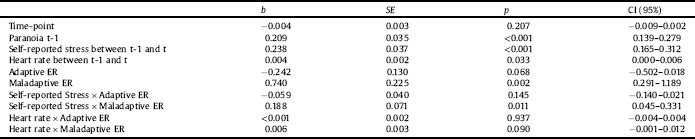
Table 2 Self-reported stress and heart rate as predictors of paranoia when controlled for time-point and paranoia on previous time-point, moderated by emotion regulation.
3.2. The association between self-reported stress and heart rate
The two indicators of daily stress, self-reported stress and heart rate were significantly correlated across subjects and time-points, with r = 0.202 (p < 0.05). However, within-subject correlation as calculated with “psych” package in R, function “statsBy”, was non-significant with r = –0.020 (p = 0.390). The same was found for the between-subject correlation with r = 0.180 (p < 0.140).
3.3. Preceding stress indicators as predictors of subsequent paranoid symptoms
For all ESM measures, one part of their variance was explained by the variation at the within-subject level (fluctuations within one person over the time) and another part at a between-subject level (differences between individuals). This was expressed by intra-class-correlation coefficient ICC (ρ = 0.523 indicating that 52.3% of the variance in paranoia was explained by fluctuations within individuals; ρ = 0.419 for self-reported stress; ρ = 0.149 for heart rate). After controlling for preceding paranoia at t-1 and for the time-point, both preceding self-reported stress and heart rate between t-1 and t were significant predictors of subsequent paranoia at t (see Table 2). In case of self-reported stress, the explained proportion of variance was R 2within = 0.20, which means that 20% of the within person variance in paranoia was explained by self-reported stress, which corresponds to a medium to large effect. For heart-rate the explained proportion of variance was R 2within = 0.04 corresponding to a small effect.
3.4. Reversed model: preceding paranoia as a predictor of subsequent stress
After controlling for preceding self-reported stress (b = 0.389, SE = 0.032, p < 0.001, 95% CI [0.323, 0.456]) and time-point (b = 0.0007, SE = 0.003, p = 0.980, 95% CI [–0.006, 0.006]), preceding paranoia at t-1 was not a significant predictor of subsequent self-reported stress between t-1 and t (b = –0.009, SE = 0.029, p = 779, 95% CI [–0.69, 0.052]).
Similarly, in a separate model, when controlled for the preceding heart rate (b = 0.532, SE = 0.031, p < 0.001, 95% CI [0.469, 0.595]) and time-point (b = 0.121, SE = 0.033, p < 0.001, 95% CI [0.055, 0.187]), preceding paranoia at t-1 was not a significant predictor of subsequent heart rate between t-1 and t (b = 0.231, SE = 0.453, p = 0.615, 95% CI [–0.704, 1.166]).
3.5. ER as moderator of the path from stress to paranoia
Maladaptive and adaptive ER were not significantly correlated (r = –0.066, p = 0.592). As can be seen in Table 2, higher values on the CERQ maladaptive subscale were associated with higher momentary paranoia. The score in adaptive ER was not related to momentary paranoia.
Maladaptive ER significantly moderated the path from preceding self-reported stress between t-1 and t to subsequent momentary paranoia at t (Table 2). Specifically, the positive unstandardized estimate (see Table 2) indicated that the more maladaptive emotion regulation strategies an individual used, the more preceding self-reported stress predicted subsequent paranoia. The effect size was medium with R 2between = 0.16, meaning that 16% of the variance in slopes for preceding self-reported stress as a predictor of paranoia was explained by maladaptive ER. As depicted in Table 2, maladaptive ER was not a significant moderator of the path from preceding heart rate to subsequent paranoia. Adaptive ER was neither a significant moderator for the path from self-reported stress to paranoia nor for the path from heart rate to paranoia.
4. Discussion
This study investigated temporal effects of self-reported as well as physiological stress on subclinical paranoia in the daily life of individuals with the elevated psychosis-proneness. Furthermore, we investigated the relevance of emotion regulation for the emergence of paranoid symptoms in the face of everyday stress.
Consistent with our first hypothesis, both preceding self-reported stress and heart rate were significantly associated with subsequent paranoia in daily life. This corroborates previous studies that found self-reported stress to predict paranoia [Reference Thewissen, Bentall, Oorschot, Campo, van Lierop and van Os6, Reference Ben-Zeev, Ellington, Swendsen and Granholm11, Reference Kramer, Simons, Wigman, Collip, Jacobs and Derom12] and extends them by showing that physiological stress is also relevant to understanding the emergence or exacerbation of paranoia. Although we had expected to find a vicious circle, in which paranoid symptoms would not only be predicted by previous stress but also be predictive of subsequent stress, this is not what we found. Rather, our results indicate that on the “micro” level of one day, the association between both self-reported and physiological stress and paranoia appears to be a “one-way street”, where daily stress impacts the severity of paranoid symptoms, but not the other way around. Nevertheless, it remains possible and plausible that paranoid symptoms will lead to elevated levels of distress on the “macro” level over a period of days or even months. Only few longitudinal studies on the association of affect and symptoms in individuals with psychosis have tested for reverse pathways. In line with our findings, the few longitudinal studies that have investigated reverse pathways also do not support the notion that positive symptoms are followed by increased anxiety [Reference Oliver, O’Connor, Jose, McLachlan and Peters40], or depressed mood [Reference Oliver, O’Connor, Jose, McLachlan and Peters40, Reference Fowler, Hodgekins, Garety, Freeman, Kuipers and Dunn41]. It needs noting that Van der Steen et al. [Reference Van Der Steen, Gimpel-Drees, Lataster, Viechtbauer, Simons and Lardinois7] report a reversed path in a clinical high risk sample, but their analysis was based on correlations and thus – strictly speaking – only supports co-occurrence between symptoms and affect rather than temporal prediction.
Maladaptive ER was predictive of paranoia and also moderated the link between self-reported stress and paranoia. In particular, participants who reported more maladaptive strategies tended to report more paranoia after experiencing stress. This implies that maladaptive ER could be a risk factor for exacerbation of paranoid symptoms under stress. In contrast to our expectation and to a previous finding from our group showing adaptive ER to moderate the increase of paranoia following a stressor [Reference Lincoln, Hartmann, Köther and Moritz24] – adaptive ER was not a significant moderator. The stronger relevance of maladaptive compared to adaptive ER are in line with findings of Aldao et al. [Reference Aldao, Nolen-Hoeksema and Schweizer16] who found maladaptive strategies to be more strongly related to general psychopathology than adaptive strategies, as well as with findings of Westermann et al. [Reference Westermann, Boden, Gross and Lincoln42] who reported only maladaptive ER to prospectively predict subclinical paranoia. Due to differences between studies in measures and in the methodological approach (experimental versus ESM), it might be premature to conclude that adaptive ER is not relevant to paranoia.
Surprisingly, the path from the physiological stress to paranoia was not moderated by ER. We can only speculate on the reasons for this; one possibility being that this pathway is influenced by different types of ER strategies (i.e. behavioral rather than cognitive strategies, such as changing the pace of breathing, or muscle relaxation) that were not assessed here.
The findings must be interpreted in light of several limitations. First, the sample primarily consisted of students limiting the generalizability of the findings to the general population where lower education and socio-economic status could be expected. Moreover, recruiting from the participant-database could have increased the risk of a selection-bias. For instance, it could be that the participants who already took part in psychological studies have a higher interest in psychological processes in general, or a higher introspection ability due to previous experiences in psychological testing. Another limitation is that due to technical features, the ambulatory physiological measurement was limited to a time period of one day. Furthermore, the intensive assessment with 38 assessment points in the course of only one day could have triggered reactivity in participants. Such a reactivity effect could become evident in a time effect (e.g. if participants pay more attention to symptoms and affective states over time resulting in higher ratings at later time-points or pay more attention in the beginning but get accustomed over time, resulting in lower ratings at later time-points). However, time-point of the assessment was included as a control variable in our analyses and showed no such effect on stress or paranoia. Also, an assessment over a longer period of time would have been beneficial to differentiate between rapid and slow changes in stress and symptoms as proposed in Jahng et al. [Reference Jahng, Wood and Trull43] as well as to measure daily life more reliably by covering both workdays and weekends. Future studies should include a direct comparison of subclinical and clinical samples to test whether the moderating mechanism of maladaptive ER found in this study applies across the continuum of psychosis.
Despite these limitations, the findings corroborate previous work showing stress to precede paranoid symptoms in daily life and shed further light on the directionality of association between stress and paranoia. A central contribution of this study is in showing that this association is not limited to the self-reports as shown in previous work but also holds true for physiological indicators of stress, i.e. heartrate. This finding thus further corroborates the relevance of autonomic stress responses for the formation and exacerbation of psychotic symptoms long-since postulated by vulnerability-stress-models [Reference Nuechterlein and Dawson44] but seldom put to rigorous empirical tests. As a clinical implication we suggest that bio-feedback methods focusing on heart-rate monitoring [Reference Clamor, Koenig, Thayer and Lincoln45, Reference McAusland and Addington46] could potentially be used to regulate physiological stress and in turn prevent the emergence of psychotic experiences for those at risk. However, further research on such bio-feedback methods is necessary before implementing them in clinical practice.
Finally, our study highlights the importance of maladaptive ER as a significant risk factor related to the question why stress in daily life translates into psychotic symptoms. Considering that we found this pattern in a subclinical sample with only elevated psychosis-proneness, we suggest that maladaptive emotion regulation should be addressed in the earliest stage possible.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
None.
Acknowledgements
We thank Edo Sebastian Jaya for his helpful feedback on the manuscript and Björn Schlier for his support in conceptualizing the study design and organizing the data collection. Furthermore we thank thestudents who conducted the data collection.





Comments
No Comments have been published for this article.