Introduction
Siblings feature prominently in the lives of most children. By middle childhood, the time a child spends with their sibling is typically greater than that spent with their parents (McHale et al., Reference McHale, Whiteman, Kim and Crouter2007), such that sibling relationships are likely to be formative for children’s development and adjustment (Pike & Oliver, Reference Pike and Oliver2017). If negative, these relationships are difficult to escape.
Although many siblings experience occasional conflict, some sibling relationships can be a source of victimization. Sibling victimization is a harmful and repeated form of intrafamily aggression, which encompasses “Any unwanted aggressive behavior(s) by a sibling that involves an observed or perceived power imbalance and is repeated multiple times or is highly likely to be repeated; bullying may inflict harm or distress on the targeted sibling including physical, psychological, or social harm. It includes two modes of bullying (direct and indirect) as well as four types of bullying (physical, verbal, relational, and damage to property).” (Wolke et al., Reference Wolke, Tippett and Dantchev2015, p. 918). Estimates of sibling victimization suggest that around 40% of young people may be exposed to sibling victimization during early adolescence (Bowes et al., Reference Bowes, Wolke, Joinson, Lereya and Lewis2014; Toseeb et al., Reference Toseeb, McChesney, Oldfield and Wolke2020b), decreasing slightly to approximately 30% in mid-adolescence (Toseeb et al., Reference Toseeb, McChesney, Oldfield and Wolke2020b). Prevalence rates appear similar globally, with estimates ranging between 20 and 30% (Borualogo & Casas, Reference Borualogo and Casas2023; Deniz et al., Reference Deniz, Derinalp, Gulkanat, Kaz, Ozhan and Toseeb2023; Liu et al., Reference Liu, Peng, Yu, Yang, Qing, Qiu and Yang2020). Taken together, these findings suggest that sibling victimization is likely to be at least as prevalent as peer victimization, with global estimates suggesting that approximately 30% of young people aged 12–17 have been victimized at school by their peers at least once in the last month (Biswas et al., Reference Biswas, Scott, Munir, Thomas, Huda, Hasan, David de Vries, Baxter and Mamun2020). Indeed, longitudinal UK cohort data have even indicated that during early to mid-adolescence, a higher percentage of children report experiencing sibling victimization (48%) than peer victimization (23%) (Sharpe et al., Reference Sharpe, Fink, Duffy and Patalay2021).
The motivations underlying sibling victimization can be conceptualized in several different ways. Sibling aggression research suggests that aggression might occur due to children mimicking behaviors such as conflict, hostility, and aggression that they observe at home (Dunn et al., Reference Dunn, Deater-Deckard, Pickering and Golding1999). Sibling victimization can also be conceptualized within Miller’s Frustration–Aggression hypothesis (Miller, Reference Miller1941), which posits that a child feels frustrated by their sibling receiving parental attention, leading to the child behaving aggressively towards their sibling. As with peer victimization (Volk et al., Reference Volk, Camilleri, Dane and Marini2012), acts of sibling aggression might also represent efforts to establish social dominance. For example, resource control theory (Hawley, Reference Hawley1999) posits that in social groups (such as families), asymmetries foster social dominance for resource acquisition. Because siblings differ in age, and therefore in size and abilities, power asymmetry is likely to exist. This means that siblings are likely to have differential access to finite parental resources, such as attention, affection, or even material goods, which might lead to aggression between siblings, as they compete for access to these resources.
There are some similarities between peer and sibling victimization, with both types of victimization involving repeated aggressive behavior with an intent to cause harm in the context of a power imbalance (Smith et al., Reference Smith, Catalano, Junger-Tas, Slee, Morita and Olweus1999). However, there are also important differences. Not least is that the perpetrator of the victimization (sibling vs peer) differs, as does the context in which they occur (inside the home vs outside of the home/in school). Furthermore, although both types of victimization involve an assertion of social dominance, sibling victimization might be more likely to be motivated by access to parental resources (according to resource control theory (Hawley, Reference Hawley1999)), whereas peer victimization is often motivated by a desire to improve social status amongst peers (Volk et al., Reference Volk, Camilleri, Dane and Marini2012).
Despite its prevalence, the severity of sibling victimization is often underestimated. It is frequently perceived as less severe than peer victimization and normalized by family members (Khan & Rogers, Reference Khan and Rogers2015). This is concerning, given emerging evidence from longitudinal cohort studies that there are many negative mental health outcomes associated with sibling victimization. Sibling victimization research typically focuses on victimization occurring during late childhood and adolescence, as these are vulnerable periods for the emergence of mental health problems. Indeed, research suggests that half of all mental health problems are established by age 14, and three quarters by age 24 (Kessler et al., Reference Kessler, Berglund, Demler, Ma, Jin, Merikangas and Walters2005). For example, Bowes et al. (Reference Bowes, Wolke, Joinson, Lereya and Lewis2014) analyzed data from the Avon Longitudinal Study of Parents and Children (ALSPAC; Boyd et al., Reference Boyd, Golding, Macleod, Lawlor, Fraser, Henderson, Molloy, Ness, Ring and Smith2013) and found that being bullied by a sibling at age 12 was prospectively associated with a doubling in the odds of both depression and self-harm at age 18. Dantchev et al. (Reference Dantchev, Hickman, Heron, Zammit and Wolke2019) built on this work, finding that, within the ALSPAC cohort, sibling victimization during early adolescence was associated with a doubling in the odds of self-harm with suicidal intent at age 24. There is also evidence from the Millennium Cohort Study (MCS) to suggest that there is a dose–response relationship between sibling victimization in early adolescence and later mental health outcomes, such that, as the frequency of sibling victimization increases, so does the severity of later mental health outcomes (Sharpe et al., Reference Sharpe, Fink, Duffy and Patalay2021; Toseeb & Wolke, Reference Toseeb and Wolke2022). Whilst such studies indicate that sibling victimization may have enduring effects on mental health, there is a lack of research exploring who is most vulnerable to developing poor mental health, and how such individuals can be supported.
As with peer victimization (Craig et al., Reference Craig, Harel-Fisch, Fogel-Grinvald, Dostaler, Hetland, Simons-Morton, Document Molcho, de Matos, Overpeck, Due, Pickett, Mazur, Favresse, Leveque, Pickett, Aasvee, Varnai, Harel and Korn2009), there are some gender differences in the prevalence of sibling victimization. Girls are more likely to report experiencing sibling victimization, whereas boys are more likely to perpetrate sibling victimization (Toseeb et al., Reference Toseeb, McChesney, Dantchev and Wolke2020a). Importantly, however, mental health and wellbeing outcomes following sibling victimization appear to be similar for both genders (Bowes et al., Reference Bowes, Wolke, Joinson, Lereya and Lewis2014).
When considering the mental health and wellbeing outcomes associated with sibling victimization, it is important to remember that sibling relationships do not exist in a vacuum. Socio-ecological theory proposes that sibling relationships can vary according to a number risk factors. These risk factors are also associated with children’s likelihood of experiencing later poor mental health and wellbeing, thus potentially confounding the relationship between sibling victimization and mental health. These risk factors can be at an individual level, such as children’s early internalizing (Kim-Cohen et al., Reference Kim-Cohen, Caspi, Moffitt, Harrington, Milne and Poulton2003) and externalizing problems (Arslan et al., Reference Arslan, Lucassen, van Lier, de Haan and Prinzie2021) and experience of peer victimization (Arseneault et al., Reference Arseneault, Bowes and Shakoor2010), or at a family level, such as parental mental health (Fitzsimons et al., Reference Fitzsimons, Goodman, Kelly and Smith2017), and family violence (Meltzer et al., Reference Meltzer, Doos, Vostanis, Ford and Goodman2009). It is important to adjust for these factors in analyses, to determine the effects of sibling victimization on mental health outcomes over and above other risk factors for poor mental health. Furthermore, there is currently a lack of research exploring factors that predict children doing better than expected following sibling victimization – that is, who display resilience. In this context, we define resilience according to Ungar and Theron’s multisystemic approach (Ungar & Theron, Reference Ungar and Theron2020) which suggests that resilience can be understood as “the process of multiple biological, psychological, social, and ecological systems interacting in ways that help individuals to regain, sustain, or improve their mental wellbeing when challenged by one or more risk factors” (Ungar & Theron, Reference Ungar and Theron2020, p. 1). Resilience therefore is not the result of individual traits, rather it emerges from an individual’s experience with multiple, interacting systems (Ungar & Theron, Reference Ungar and Theron2020). It is also important to note that resilience is not a concept which can be directly measured, rather it can be inferred from an individual’s mental health and wellbeing following adversity (Schoon, Reference Schoon2009).
Resilience research has identified factors associated with better-than-expected outcomes following adversity, known as promotive factors. These are main effects which are associated with a decrease in problematic outcomes. This means that regardless of whether an individual is in a high- or low-risk group for experiencing negative outcomes, a promotive factor will be associated with improved outcomes (Brumley & Jaffee, Reference Brumley and Jaffee2016). Protective factors, on the other hand, are moderating variables which have an especially positive effect in the presence of risk – they interact with the risk exposure (Brumley & Jaffee, Reference Brumley and Jaffee2016). This means that they have a greater effect at reducing problematic outcomes for those in high-risk groups than in low-risk groups.
Studies have focused on factors at the family, peer, school, and neighborhood level associated with risk and resilience following forms of interpersonal violence such as victimization by peers, however there is a lack of research on victimization by siblings. Models of cumulative adversity indicate that children growing up in more disadvantaged circumstances might be more sensitized to stressful life experiences, such as victimization (McLaughlin et al., Reference McLaughlin, Green, Gruber, Sampson, Zaslavsky and Kessler2012; Shonkoff et al., Reference Shonkoff, Garner, Dobbins, Earls, Garner, McGuinn, Pascoe and Wood2012). In terms of resilience, supportive relationships with both family and friends have been found to promote resilience to peer victimization (Bowes et al., Reference Bowes, Maughan, Caspi, Moffitt and Arseneault2010; Hodges et al., Reference Hodges, Boivin, Vitaro and Bukowski1999). At the broader ecology, the wider context, including the school and neighborhood, might also promote resilience to peer victimization (Armitage et al., Reference Armitage, Wang, Davis, Collard and Haworth2021; McVie, Reference McVie2014). However, given the differences in context, perpetrator, and motivation (outlined above) between peer and sibling victimization, it is unclear whether promotive and risk factors for peer victimization will generalize to sibling victimization.
Identifying promotive and risk factors for better or worse mental health and wellbeing following sibling victimization may help to identify potential targets for future interventions to support children who have experienced sibling victimization. Such interventions are needed, as at the time of writing there are no interventions designed specifically for sibling victimization. Even within the wider field of sibling relationships, a recent meta-analysis of parenting interventions to improve sibling interactions concluded that although interventions showed promising effects, this area is underdeveloped in terms of the number, size, and robustness of studies (Leijten et al., Reference Leijten, Melendez-Torres and Oliver2021).
To help to address gaps in the sibling victimization literature, we used data from over 12,000 families from the MCS, a large representative contemporary longitudinal UK birth cohort (Connelly & Platt, Reference Connelly and Platt2014), to answer the following research questions: is exposure to sibling victimization at 11 years old and/or 14 years old associated with mental health and wellbeing outcomes at 17 years old, when controlling for other risk factors known to influence later mental health? And, if a relationship is found between sibling victimization and mental health and wellbeing, are there promotive and risk factors at the family, peer, school, and neighborhood level which predict better or worse mental health and wellbeing outcomes following victimization?
Previous research using MCS data has shown that sibling victimization is associated with a range of poor mental health and wellbeing outcomes (Sharpe et al., Reference Sharpe, Fink, Duffy and Patalay2021; Toseeb & Wolke, Reference Toseeb and Wolke2022). Our work builds on this research to explore associations between sibling victimization and later mental health and wellbeing when adjusting for additional key covariates, and most importantly, to address a gap in the sibling victimization literature by investigating risk and promotive factors associated with children’s resilience to sibling victimization. This will help to identify those most at risk of poor outcomes following exposure to sibling victimization, as well as informing the potential targets of future interventions to support young people following sibling victimization.
We considered measures of both negative mental health (symptoms associated with mental illness) and positive mental health (general wellbeing) following exposure to sibling victimization. This is in line with the World Health Organization definition of health as “a state of complete physical, mental and social wellbeing and not merely the absence of disease or infirmity.” (World Health Organization, 1948, p. 2), and the two-continua model of mental health which proposes that negative and positive mental health are related but distinct constructs (Westerhof & Keyes, Reference Westerhof and Keyes2010). Indeed, research using data from the MCS found that correlates of positive and negative mental health are largely distinct during adolescence, demonstrating the importance of considering these two constructs separately (Patalay & Fitzsimons, Reference Patalay and Fitzsimons2016).
It was hypothesized that there would be a dose–response relationship between victimization frequency and poor outcomes, such that those who were victimized more frequently during early and mid-adolescence might experience worse mental health and lower levels of wellbeing at age 17 than those victimized less frequently. We expected the association to remain after adjusting for the following covariates: child’s biological sex, living with a stepsibling, number of siblings in the household, early internalizing and externalizing problems, autism spectrum disorder diagnosis, experience of peer victimization, household income, maternal depression, frequent parental alcohol use, and household domestic violence.
In line with a socio-ecological approach, promotive and risk factors potentially associated with resilience were explored at the family, peer, school, and neighborhood level. We identified factors in the MCS data set which most closely matched promotive and risk factors identified in the peer victimization literature. It was hypothesized that the following factors would be associated with worse-than-expected mental health and wellbeing outcomes following exposure to sibling victimization: at the family level – experiencing financial strain, overcrowding in the home, experiencing lower levels of parental monitoring and having a poor quality parent-child relationship; at the peer level – having no close friends; at the school level, having lower levels of school motivation and engagement; and at the neighborhood level-not feeling safe to walk, play or hangout in the area around their home.
It was hypothesized that the following factors would be promotive and associated with better-than-expected mental health and wellbeing outcomes following exposure to sibling victimization: at the family level – experiencing higher levels of parental monitoring and higher-quality parent-child relationship; at the peer level – having at least one close friend; at the school level – having higher levels of school motivation and engagement; and at the neighborhood level – feeling safe to walk, play or hangout in the area around their home.
It was not clear whether any factors would be particularly helpful in the context of sibling victimization specifically (i.e., protective factors). If any factors were identified as promotive, we planned to conduct exploratory analyses to see whether these factors moderated the impact of sibling victimization on outcomes.
Method
Data source
The sample consisted of participants from the MCS, an ongoing multi-disciplinary longitudinal birth cohort, following 19,517 individuals born in the UK between September 2000 and January 2002 (Connelly & Platt, Reference Connelly and Platt2014). MCS data is publicly available through the UK Data Service. The NHS Research Ethics Committee provided ethical approval for all sweeps. Detailed information on the MCS can be found in the MCS technical reports (https://cls.ucl.ac.uk/cls-studies/millennium-cohort-study/).
Sample
We analyzed data from sweeps 1 to 2 and 4 to 7 (ages 9 months, 3, 7, 11, 14 and 17 years). All cohort members who provided information on sibling victimization at either the age 11 or age 14 survey were included. Those without any siblings at both age 11 and at age 14 were excluded.
Study measures
Exposure to sibling victimization
Sibling victimization was assessed at age 11 and 14 using cohort member responses to the following survey item: “How often do your brothers or sisters hurt you or pick on you on purpose?” Response options were: “Most days,” “About once a week,” “About once a month,” “Every few months,” “Less often,” “Never,” “Don't have brothers or sisters.”
For descriptive purposes, we created three categorical groups of sibling victimization: no victimization exposure (not victimized at either 11 or 14 years old, or, for cases where data at one time point was missing – not victimized at one time point and missing data at the other time point); victimized at one time point (victimized at either at 11 or 14 years old, or, for cases where data at one time point was missing – victimized at one time point and missing data at the other time point); and victimized at both time points (victimization at both 11 and 14 – it was not possible to have missing data for this category). Following the definition of sibling victimization by Wolke et al., (Reference Wolke, Tippett and Dantchev2015, p. 918) which states that bullying behavior is “repeated multiple times,” to be categorized as experiencing sibling victimization, a frequency of at least “about once a week” had to be selected. We excluded those without siblings at both timepoints. It was possible that some cohort members reported sibling victimization at one timepoint, but reported not having a sibling at another timepoint. In this scenario, the response option “Don't have brothers or sisters” was recoded as “Never.”
For the main analyses, we created a continuous variable of sibling victimization frequency, summing the victimization frequency at 11 and 14 years old after reverse coding such that, for each time point, victimization frequency ranged from 0 (“Never”) to 5 (“Most days”). Possible summed scores ranged from 0 to 10, with higher scores indicating more frequent victimization. When there was missing data at one time point (6% were missing sibling victimization data at age 11, and 17% were missing sibling victimization data at age 17), missing data for that time point was included as a frequency of 0 (“Never”), meaning that those with data at one time point automatically scored in the lower end of frequency (with a possible maximum score of 5). Missing data at both time points was excluded from complete case analyses.
Mental health and wellbeing outcomes
The following outcomes were assessed when cohort members were age 17:
Cohort members’ internalizing and externalizing problems were assessed using the self-report Strengths and Difficulties Questionnaire (SDQ; (Goodman, Reference Goodman1997)), with reference to the preceding six months. Responses were coded on a three-point scale (0 = Not true, 1 = Somewhat true, 2 = Certainly true). As per instructions for scoring, four five-item subscales were created: emotional problems (Complains of headaches/stomach aches/sickness, Often seems worried, Often unhappy, Nervous or clingy in new situations, Many fears, easily scared), peer problems (Tends to play alone, Has at least one good friend, Generally liked by other children, Picked on or bullied by other children, Gets on better with adults), conduct problems (Often has temper tantrums, Generally obedient, Fights with or bullies other children, Steals from home, school or elsewhere, Often lies or cheats), and hyperactivity and inattention (Restless, overactive, cannot stay still for long, Constantly fidgeting, Easily distracted, Can stop and think before acting, Sees tasks through to the end). Following established scoring guidelines (https://www.sdqinfo.org/py/sdqinfo/c0.py), the emotional and peer problems subscales were combined to create an internalizing problems subscale and the conduct and hyperactivity subscales were combined to create an externalizing subscale. For all subscales, higher scores indicated more mental health difficulties. In this study, the SDQ shows acceptable internal reliability for internalizing problems (α = 0.59) and low internal reliability for externalizing problems (α = 0.46).
Cohort members’ mental wellbeing was assessed using the self-report Short Warwick-Edinburgh Mental Wellbeing Scale, which consists of seven items asking about thoughts and feelings over the past two weeks (Tennant et al., Reference Tennant, Hiller, Fishwick, Platt, Joseph, Weich, Parkinson, Secker and Stewart-Brown2007). Sample questions include “I’ve been feeling optimistic about the future” and “I’ve been thinking clearly.” Responses to the questions were coded on a five-point scale (1 = None of the time, 2 = Rarely, 3 = Some of the time, 4 = Often, 5 = All of the time). These were summed and scaled in line with scoring guidelines, so that higher scores indicated higher levels of wellbeing. The Short Warwick-Edinburgh Mental Wellbeing Scale has good internal reliability (α = 0.83) in this study.
To assess self-harm, young people were asked whether they had hurt themselves on purpose in the preceding year. They were provided with examples of self-harming behaviors and asked to respond on a binary scale (0 = No, 1 = Yes). The behaviors were: “cut or stabbed yourself,” “burned yourself,” “bruised or pinched yourself,” “taken an overdose of tablets,” “pulled out your hair” and “hurt yourself in some other way.” They were also asked “Have you ever hurt yourself on purpose in an attempt to end your life?.” These questions were taken from the Edinburgh Study of Youth and Transitions (https://www.edinstudy.law.ed.ac.uk/). The internal reliability of these measures in this study is acceptable (α = 0.74). A single binary variable (self-harm, no self-harm) was created, based on whether a young person answered yes to any of the above behaviors, or no to all the above behaviors.
Potential risk and promotive factors
We selected potential risk and promotive factors at the family, peer, school, and neighborhood level a priori based on theoretical knowledge and the research literature for peer victimization. We used factors measured at age 14, to ensure that potential risk and potential promotive factors were in place between sibling victimization occurring and the later measurements of mental health and wellbeing.
Family level
Financial strain within the cohort member’s household was assessed using a variable derived by the MCS, flagging whether family income was below the Organization for Economic Co-operation and Development 60% median poverty indicator for the UK (for more information on MCS derived variables, see http://doc.ukdataservice.ac.uk/doc/8156/mrdoc/pdf/mcs6_user_guide_ed2_2020-08-10.pdf).
Overcrowding at home (rooms per capita) was assessed in this study using a variable created from two existing variables: primary caregiver reported variables of how many people (including the cohort member) live in the household, divided by how many rooms the family had (excluding bathrooms, toilets, halls, and garages). A higher value indicated a higher level of overcrowding.
Parental monitoring was assessed via a composite variable, created for this study, which summed responses to the primary caregiver report items of: “When [^Cohort member’s name] goes out how often do you know where [^he/she] is going?,” “When [^Cohort member’s name] goes out how often do you know who [^he/she] is going out with?,” “When [^Cohort member’s name] goes out how often do you know what [^he/she] is doing?.” Responses to each question were coded on a four-point scale (1 = Never, 2 = Sometimes, 3 = Usually, 4 = Always), a higher total score indicated a higher level of monitoring. The internal reliability of these measures in this study is acceptable (α = 0.77).
Parent-child relationship was assessed via the primary caregiver reported item of “How often do you talk to [^Cohort member’s name] about things that are important to [^him/her]?.” Responses were coded on a five-point scale (1 = Every day or almost every day, 2 = Several times a week, 3 = Once or twice a week, 4 = Once or twice a month, 5 = Less often than once a month, 6 = Not at all) and reverse coded so that a higher score indicated a higher-quality relationship.
Peer level
Whether a cohort member had a close friend(s) or not was measured using the cohort member report item: “By close friends we mean other young people you feel at ease with or who you can talk to about things that are private. Do you have any close friends?,” with binary responses (Yes/No).
School level
School motivation/engagement was assessed via a composite measure created for this study, from cohort member responses to six items, which were adapted from items in the 1970 British Cohort Study (Elliott & Shepherd, Reference Elliott and Shepherd2006) and National Child Development Survey (Power & Elliott, Reference Power and Elliott2006). Items were as follows: “How often do you try your best at school?,” “How often do you find school interesting?,” “How often do you feel unhappy at school?,” “How often do you get tired at school?,” “How often do you feel school is a waste of time?,” “How often do you find it difficult to keep your mind on your work at school?.” Responses to each question were coded on a four-point scale (1 = Never, 2 = Sometimes, 3 = Usually, 4 = Always), and reverse coded where necessary. Responses to each item were summed, a higher total score indicated a higher level of school motivation/engagement. The internal reliability of these measures in this study is acceptable (α = 0.74) and in line with previous studies which have utilized these measures (e.g., Duckworth & Schoon (Reference Duckworth and Schoon2012) in the British Cohort Study).
Neighborhood level
Whether young people felt safe in their neighborhood was assessed using cohort member responses to the item: “How safe is it to walk, play or hang out in this area during the day? By this area we mean within about a mile or 20-minute walk from your home.” Possible responses were: “Very safe,” “Safe,” “Not very safe” and “Not at all safe.”
Due to the small sample size for the “Not at all safe” category, this category was collapsed into the “Not very safe” category for all study analyses.
Potential confounders
We selected potential confounders at the individual and family level, for risk of experiencing sibling victimization and experiencing poor mental health and wellbeing outcomes, a priori based on factors in the MCS which matched most closely onto the research literature for sibling victimization (e.g., the precursors to sibling victimization in Dantchev et al. (Reference Dantchev, Hickman, Heron, Zammit and Wolke2019) and Toseeb et al. (Reference Toseeb, McChesney, Dantchev and Wolke2020a)) and family violence. We chose confounders which were measured at or before age 11, as age 11 is the first time point at which sibling victimization is measured.
Individual characteristics
At the first wave of data collection, when cohort members were aged 9 months, primary caregivers reported their child’s biological sex (male/female).
To assess pre-existing mental health difficulties (early internalizing and externalizing problems), the parent-report SDQ was completed by the primary caregiver when the child was seven years old (Goodman, Reference Goodman1997).
Whether a child had received an autism spectrum disorder diagnosis was also assessed via primary caregiver report when the child was seven years old, as previous research from the MCS highlights that those with an autism spectrum disorder diagnosis are more likely to be victims of sibling victimization and have internalizing and externalizing problems (Toseeb et al., Reference Toseeb, McChesney, Oldfield and Wolke2020b). Whether the cohort member had any stepsiblings living in the same household as them was also assessed via primary caregiver report at age seven, as was whether the cohort member had experienced any victimization by peers, assessed via the item “[^Cohort child’s name] is picked on or bullied by other children.”
Family level
Analyses were also adjusted for a range of family factors derived from primary caregiver reports. Socio-economic position of the family was assessed when the cohort member was three years old via household income (a measure of total take-home household income after tax and other deductions, split into six categories).
At age seven, the following variables were assessed via primary caregiver report: parental depression, measured using the K6 Kessler Distress Scale (Kessler et al., Reference Kessler, Andrews, Colpe, Hiripi, Mroczek, Normand, Walters and Zaslavsky2002); frequent alcohol consumption by the primary caregiver, coded for this study as primary caregivers who selected that they drink alcohol “Every day” or “5–6 times per week”; primary caregiver’s experience of domestic violence was assessed via the question “People often use force in a relationship – grabbing, pushing, shaking, hitting, kicking etc. Has your [^husband/wife/partner] ever used force on you for any reason?,” with the response options “Yes,” “No,” “Don't wish to answer.”
At age 11, the number of cohort member’s siblings living in the cohort member’s household was assessed using a variable derived by the MCS from the main caregiver report on household composition.
Statistical analyses
All analyses were pre-registered at the Open Science Framework (https://osf.io/qsvya) and conducted using R version 4.1.1 (R Core Team, 2021).
As there can be differences between the genders in terms of sibling victimization prevalence (Toseeb et al., Reference Toseeb, McChesney, Dantchev and Wolke2020a), we tested for interactions between sibling victimization frequency and gender for each outcome variable using unadjusted linear regressions. The interaction term was significant for externalizing problems only (β = 0.06, 95% CI = 0.02–0.10, p = .006. Internalizing problems: β = 0.02, 95% CI = −0.03 to 0.06, p = .464; wellbeing: β = −0.02, 95% CI = −0.06 to 0.02, p = .347; self-harm β = 0.04, 95% CI = −0.01 to 0.08, p = .103). Therefore, analyses were stratified by gender for externalizing problems.
To determine a potential dose–response effect of sibling victimization on later mental health and wellbeing, we ran five unadjusted univariate regression models for each outcome (internalizing problems (1), externalizing problems – girls (2), externalizing problems – boys (3), wellbeing (4), and self-harm (5)), after which we entered covariates (potential confounding variables) into each model. In line with previous sibling victimization literature (Bowes et al., Reference Bowes, Wolke, Joinson, Lereya and Lewis2014), quadratic (sibling victimization frequency variable squared) and cubic (sibling victimization frequency variable cubed) terms were added to the models to test whether the relationship between victimization and mental health and wellbeing outcomes was non-linear. Model fit indices (Akaike Information Criterion, Bayesian Information Criterion, and Likelihood ratio tests) were used to determine whether non-linear relationships were present. There was no evidence for non-linear relationships for any of the models, except internalizing problems, where a cubic model provided a marginally better fit according only to Bayesian Information Criterion. However, in the interest of parsimony, a linear model was applied. Thus, in the interest of simplicity and comparability across outcomes, we applied linear models for all outcomes thereafter. Bonferonni corrections were also applied to correct for multiple testing.
We followed a residuals approach to measure resilient functioning for each mental health and wellbeing outcome following exposure to sibling victimization. This approach has been used in previous studies exploring children’s resilience to adverse experiences (for example, Bowes et al. (Reference Bowes, Maughan, Caspi, Moffitt and Arseneault2010); Collishaw et al. (Reference Collishaw, Hammerton, Mahedy, Sellers, Owen, Craddock and Thapar2016); van Harmelen et al. (Reference van Harmelen, Kievit, Ioannidis, Neufeld, Jones, Bullmore, Dolan and Goodyer2017)). Recent research demonstrated that operationalizing young people’s resilience to psychopathology following exposure to adversity using a residuals approach had good construct and predictive validity (Cahill et al., Reference Cahill, Hager and Chandola2022).
The conceptual basis for a residuals approach to resilience follows the assumption that psychosocial outcomes are determined by multiple factors (exposure to sibling victimization being one such determinant), and that the independent contributions of these factors can be estimated (Cahill et al., Reference Cahill, Hager and Chandola2022). This approach decomposes variance in the outcome variables into a component explained by exposure to a particular adversity (in our study, sibling victimization) and a residual component that is independent of exposure to the measured adversity. The residual component therefore reflects individual differences in the outcome variable which are not explained by exposure to the measured adversity. The residual scores consequently reflect a range of functioning from “risk” to “resilient,” that is, the extent to which a young person had worse, or better, outcomes than predicted given their level of exposure to sibling victimization, and as such is our measure of resilient functioning. Please see Cahill et al. (Reference Cahill, Hager and Chandola2022) for a comprehensive overview of this method.
For each mental health and wellbeing outcome, we extracted residual scores from the unadjusted linear regressions. The extracted residual scores were then associated with risk and promotive factors for each mental health and wellbeing outcome using adjusted univariate regression models for each factor, followed by adjusted multiple regression models, which included all potential risk and promotive factors in one model for each outcome variable. In exploratory analyses, we conducted additional regression models for each mental health and wellbeing outcome, with interaction effects (sibling victimization*promotive factor) for any promotive factors found to have significant main effects, to examine whether these factors may buffer the impact of sibling victimization on outcomes (i.e., to test for protective effects).
Missing data
Multiple imputation by chained equations (Azur et al., Reference Azur, Stuart, Frangakis and Leaf2011) was used to impute to outcome, and account for missing data in risk factors, promotive factors, and covariates for main regression analyses (percentages of missing data can be found in the supplementary material). The multiple imputation by chained equations package (van Buuren & Groothuis-Oudshoorn, Reference van Buuren and Groothuis-Oudshoorn2011) was used on a data set with complete data on sibling victimization and mental health outcomes at age 17 (n = 8682). To improve missing data estimates, socio-economic variables which are known to predict later missingness in the MCS were included as auxiliary variables in the imputations. The auxiliary variables are available from the authors on request. Averaged parameter estimates (White et al., Reference White, Royston and Wood2011) from data imputed over 30 data sets are presented. Analyses with the original, complete case data can be found in the supplementary material.
Following the MCS data handling guide, weights were applied by including the stratum design variable “PPTYPE2” as a dummy variable in all regression analyses (see, https://cls.ucl.ac.uk/wp-content/uploads/2020/09/MCS1-5_User_Guide_ed9_2020-08-07.pdf).
Results
Descriptive statistics
There were 12,521 participants in the complete case sample (those who provided data on sibling victimization for at least one time point). Of this sample, nearly half (47.87%) reported experiencing sibling victimization, with 35.07% reporting victimization at one time point (at either age 11 or 14 years) and 12.80% reporting sibling victimization at both age 11 and 14 years (Table 1). Boys were less likely to have experienced victimization at both time points than girls. Generally, girls experienced higher mean levels of mental health problems and lower wellbeing at age 17 than boys, except for mean externalizing problems (Table 1).
Table 1. Sibling victimization frequencies and mental health and wellbeing outcomes

Note: Using complete case responses (n = 12, 521).
Table 2 shows individual and family characteristics of children as a function of their exposure to sibling victimization. Overall, children who experienced sibling victimization were more likely to be female, to have parents identify them as “white,” be the eldest child and live in families with more than two siblings. There were significant differences (p < .001) between sibling victimization groups for each characteristic.
Table 2. Sample characteristics

Note: Using complete case responses (n = 12, 521).
Table 3 shows the descriptive statistics for covariates, split by sibling victimization exposure group. For individual factors, those who experienced sibling victimization were more likely to live in a household with a higher number of siblings, have higher levels of early internalizing and externalizing problems, and have received an autism spectrum disorder diagnosis. Percentages of children who had experienced peer victimization at age 7 were similar across sibling victimization categories.
Table 3. Covariates

Note: Using complete case responses (n = 12, 521). ***indicates p < .001, **indicates p < .01, *indicates p < .05.
For family factors, generally a slightly higher percentage of children who experienced sibling victimization came from households with a higher household income. Mean level of maternal depression was slightly higher for those who had experienced sibling victimization. Similarly, a slightly higher percentage of main caregivers reported frequent alcohol use and domestic violence in the sibling victimization categories.
Missing data analysis
A missing data analysis was conducted to explore whether any covariates significantly correlated (at p < .05) with missing mental health and wellbeing outcome data at age 17 (Table 4). Those who had missing outcome data were significantly more likely to be female, have higher levels of early internalizing and externalizing problems (at age 7 years), experience higher levels of peer victimization (at age 7 years), have a mother with a higher level of depression (measured at age 3 years), and live in a household with a lower income (measured at age 3 years).
Table 4. Missing data analysis comparing covariates between those with full sibling victimization (exposure) and mental health and wellbeing data (outcome), and those with complete exposure data but incomplete outcome data
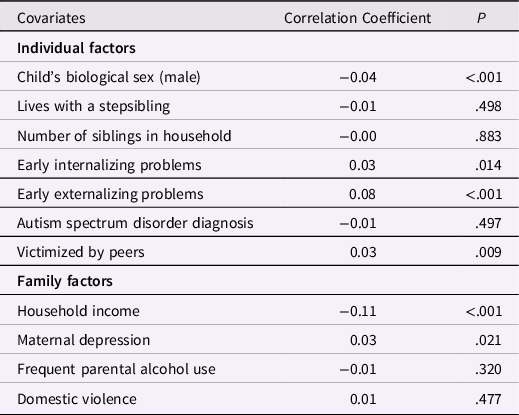
Note: Using complete case responses.
Main analyses
The association of sibling victimization with later mental health and wellbeing
In all models (using imputed data), sibling victimization was associated with worse mental health and wellbeing outcomes (Table 5). In unadjusted models, sibling victimization was associated with small but significant (at p < .001) effect sizes (Table 5), for internalizing and externalizing problems, and wellbeing outcomes. Effect sizes were only slightly attenuated when adjusting for confounding variables and remained significant at p < .001. For the binary outcome of self-harm, in the unadjusted model, greater exposure to sibling victimization was associated with a higher likelihood of having self-harmed, the odds ratio was small but significant. The odds ratio remained significant after adjusting for confounders.
Table 5. The association between sibling victimization frequency (at 11 and/or 14 years old) and mental health and wellbeing outcomes at 17 years old
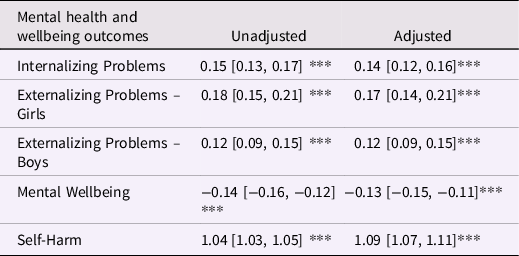
Note: 1. With imputed data, n = 8682 for Internalizing Problems, Mental Wellbeing and Self-Harm, n = 4298 for Externalizing – Girls, and 4072 for Externalizing – Boys. 2. Standardized beta values and [95% confidence intervals] are reported for Internalizing and Externalizing Problems and Mental Wellbeing. The Odds Ratio and [95% confidence interval] is reported for Self-Harm. 3. Positive coefficients indicate worse outcomes for Internalizing and Externalizing Problems. For Mental Wellbeing, negative coefficients indicate worse outcomes. For Odds Ratios (Self-Harm), a higher value indicates a higher likelihood of the outcome occurring. 4. Adjusted models controlled for child’s biological sex (with the exception of Externalizing models, which are stratified by gender), pre-existing mental health difficulties (early internalizing and externalizing problems), diagnosis of autism spectrum disorder, whether cohort member lives with a stepsibling(s), number of siblings in the cohort member’s household, experience of peer victimization, family household income, maternal depression, frequent parental alcohol use, and household domestic violence. 5. *** indicates p < .001.
Sensitivity analyses were run on imputed data to further explore the association between sibling victimization and self-harm, separating self-harm outcomes into “self-harm with suicidal intent” (n = 685) (those who answered “yes” to the question : “Have you ever hurt yourself on purpose in an attempt to end your life?”) and “self-harm without suicidal intent” (n = 2, 535) (those who answered no to “Have you ever hurt yourself on purpose in an attempt to end your life?” but yes to any of the other six self-harm items which assessed self-harm behaviors without suicidal intent – see the methods section for the full description of these items). Fully adjusted and weighted univariate linear regression models were run for each outcome, with sibling victimization frequency as the predictor and self-harm type as the outcome. In both models, sibling victimization was significantly associated with self-harm types at p < .001. The odds ratio for each outcome were similar to the odds ratio for the overall self-harm group model: “self-harm without suicidal intent” model: OR = 1.09, 95% CI = 1.06–1.10; “self-harm with suicidal intent” model – OR = 1.05, 95% CI = 1.03–1.08.
Are there promotive and risk factors which predict children’s resilience to sibling victimization?
Results of univariate and multivariate regression analyses indicated that a range of factors at the family, peer, school, and neighborhood level were associated with children’s resilience to sibling victimization (Tables 6 and 7 – risk and promotive factors for externalizing problems are presented separately in Table 7, as results for this outcome are stratified by gender). Generally, the largest effect sizes were for factors at the peer, school, and neighborhood level. Significant associations are reported in this section, other non-significant results can be seen in Tables 6 and 7.
Table 6. The association between potential risk and promotive factors and children’s resilience to internalizing problems, low wellbeing, and self-harm following sibling victimization
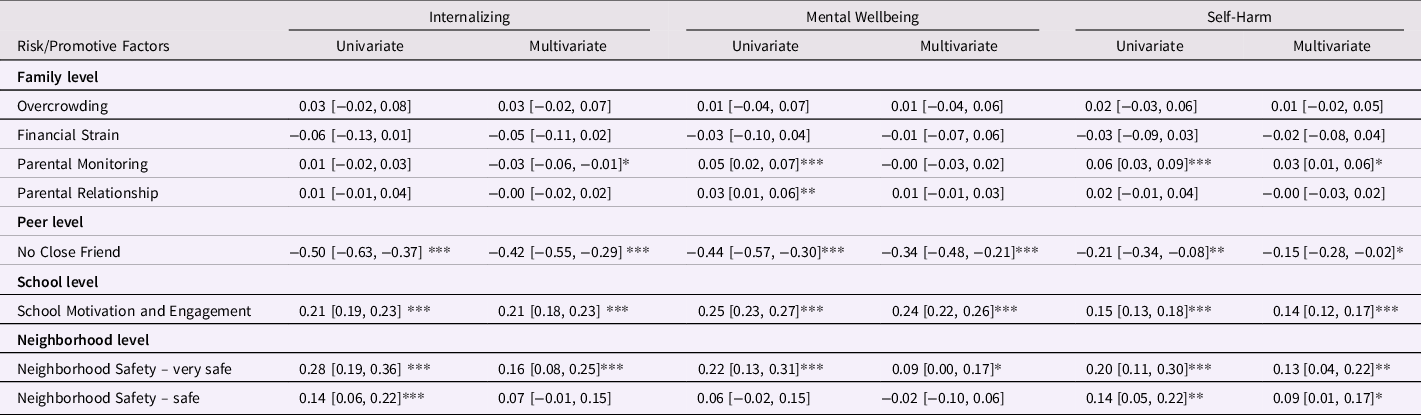
Note: 1. Using imputed data, n = 8682 for each outcome. 2. Standardized beta values and [95% confidence intervals]. 3. Positive coefficients indicate better-than-expected outcomes, negative coefficients indicate worse-than-expected outcomes. 4. All models adjusted for: child’s biological sex, pre-existing mental health difficulties (early internalizing and externalizing problems), diagnosis of autism spectrum disorder, whether cohort member lives with a stepsibling(s), number of siblings in the cohort member’s household, experience of peer victimization, family household income, maternal depression, frequent parental alcohol use, and household domestic violence. 5. *** indicates p < .001, ** indicates p < .01, *indicates p < .05. 6. For the Neighborhood Safety variable, the responses are in comparison to those who answered “Not very Safe.”
Table 7. The association between potential risk and promotive factors and children’s resilience to externalizing problems following sibling victimization
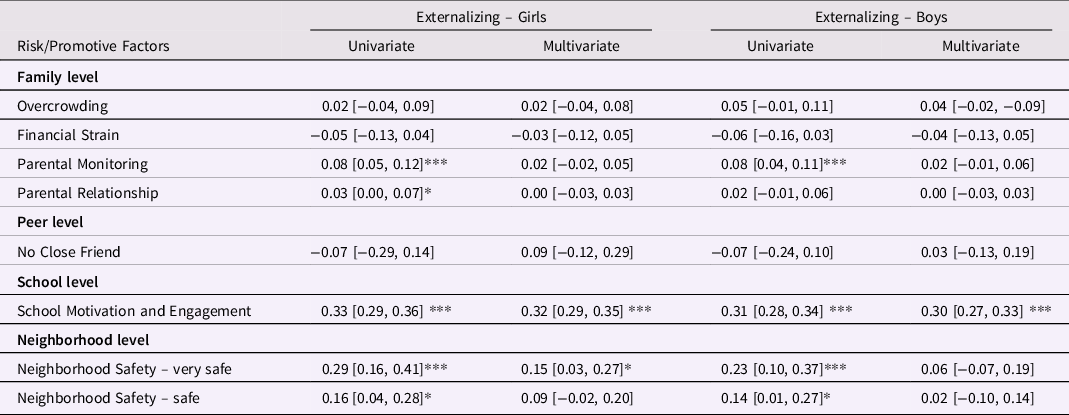
Note: 1. Using imputed data, n = 4298 for Externalizing – Girls, and n = 4072 for Externalizing – Boys. 2. Standardized beta values and [95% confidence intervals]. 3. Positive coefficients indicate better-than-expected outcomes, negative coefficients indicate worse-than-expected outcomes. 4. Models adjusted for: pre-existing mental health difficulties (early internalizing and externalizing problems), diagnosis of autism spectrum disorder, whether cohort member lives with a stepsibling(s), number of siblings in the cohort member’s household, experience of peer victimization, family household income, maternal depression, frequent parental alcohol use, and household domestic violence. 5. *** indicates p < .001, ** indicates p < .01, *indicates p < .05. 6. For the Neighborhood Safety variable, the responses are in comparison to those who answered “Not very Safe.”
Univariate analyses
Family level
Higher levels of parental monitoring were significantly associated with better-than-expected outcomes for externalizing problems (girls and boys), wellbeing and self-harm, with very small (but significant) effects on resilient functioning. Higher-quality parental relationships were significantly associated with better-than-expected outcomes for externalizing problems (girls) and wellbeing. However, for both factors, effect sizes were very small (β = 0.03 to β = 0.08), and as such should be interpreted with caution.
Peer level
Having no close friend (compared to having a close friend) was significantly associated with worse-than-expected levels of internalizing problems, wellbeing, and self-harm, with small to medium effect sizes (Tables 6 and 7).
School level
Having higher levels of school motivation and engagement was significantly associated with better-than-expected outcomes across all measures of mental health and wellbeing, with small effect sizes (Tables 6 and 7).
Neighborhood level
Living in a neighborhood where cohort members felt “very safe” (compared to feeling “not very safe”) was associated with better-than-expected functioning for all mental health and wellbeing outcomes, with small but significant effect sizes (Tables 6 and 7). Living in a neighborhood where cohort members felt “safe” (compared to feeling “not very safe”) was also associated with better-than-expected levels of internalizing problems and girls’ externalizing problems, wellbeing, and self-harm, but with smaller effect sizes than living in a “very safe” neighborhood.
Multivariate analyses
There were several factors which still had independent effects on resilience to sibling victimization when all potential risk and promotive factors were included in multivariate models for each mental health/wellbeing outcome (see Tables 6 and 7). Generally, effect sizes and significance values for factors were slightly attenuated in multivariate models.
Family level
In multivariate models, higher levels of parental monitoring remained a significant promotive factor for resilience to self-harm, albeit with a very small effect size. Parental monitoring was no longer a significant promotive factor for better-than-expected levels of externalizing problems and wellbeing. Parental relationship was no longer a significant promotive factor for any outcomes.
Peer level
In multivariate models, having no close friend remained a significant risk factor for worse-than-expected outcomes for internalizing problems, wellbeing and self-harm, however with attenuated effect sizes. Despite reduced effect sizes, in multivariate models for internalizing problems, wellbeing and self-harm, having no close friend was the factor associated with the largest effect sizes for worse-than-expected outcomes.
School level
Higher levels of school motivation and engagement remained a significant (at p < .001) promotive factor for better-than-expected functioning for all mental health and wellbeing outcomes. Effects were only slightly attenuated when moving from a univariate model for school motivation and engagement to including it as a factor in multivariate models.
Neighborhood level
Feeling “very safe” remained a significant predictor of better-than-expected outcomes for all outcomes apart from boys’ externalizing problems. However, effect sizes were between 35 and 59% smaller and significance levels reduced when this factor was included in multivariate models for each outcome, compared to the univariate model for feeling “very safe.” Feeling “safe” remained a significant promotive factor only for lower-than-expected levels of self-harm, however both effect size and level of significance were reduced.
Exploratory analyses – are any promotive factors in fact protective?
Exploratory analyses were run to check whether, for each mental health and wellbeing outcome, there were any significant (p < .05) interactions between promotive factors (factors identified as being significantly associated with better-than-expected outcomes for that particular outcome in multivariate linear regressions – see Tables 6 and 7) and sibling victimization frequency (Table 8). For all outcomes, the effect size for interactions between the promotive factor and sibling victimization frequency were small. There was only one significant interaction (p = .037), between neighborhood safety (very safe)* sibling victimization frequency and lower-than-expected internalizing problems (β = 0.09, 95% CI = 0.01–0.17). Further exploration of this interaction showed that living in a “very safe” neighborhood, compared to living in a “not very safe” neighborhood, was associated with greater increases in children’s resilience to internalizing problems for those who had experienced higher levels of sibling victimization (scores equal to or above +1 standard deviation of the mean level of sibling victimization frequency) compared to those exposed to lower levels of victimization (scores equal to or below −1 standard deviation of the mean level of sibling victimization frequency). See Figure 1 in the supplementary materials for more information.
Table 8. Exploratory analyses – adjusted regression models including an interaction term of sibling victimization frequency by each potential protective factor predicting mental health and wellbeing at age 17

Note: 1. Using imputed data, n = 8682 for Internalizing problems, Mental Wellbeing and Self-Harm, n = 4298 for Externalizing – Girls, and n = 4072 for Externalizing – Boys. 2. Adjusted models controlled for child’s biological sex (with the exception of Externalizing models, which are stratified by gender), pre-existing mental health difficulties (early internalizing and externalizing problems), diagnosis of autism spectrum disorder, whether cohort member lives with a stepsibling(s), number of siblings in the cohort member’s household, experience of peer victimization, family household income, maternal depression, frequent parental alcohol use, and household domestic violence. 3. * indicates p < .05.
Discussion
Using longitudinal data from a contemporary UK birth cohort to explore children’s resilience to sibling victimization, we found that, even after controlling for a range of confounders, any experience of sibling victimization in early and/or mid-adolescence was associated with significantly worse mental health and wellbeing in later adolescence. There was also evidence of dose–response associations between exposure to sibling victimization and all mental health and wellbeing outcomes at age 17 years. Associations were similar for boys and girls, except for externalizing problems, where sibling victimization was associated with larger effects for girls than boys. However, it should be noted that the internal reliability for measures of externalizing problems in this sample is low, so results relating to externalizing symptoms should be interpreted with caution.
The dose–response nature of the relationship between sibling victimization exposure and later mental health and wellbeing suggests that it is not only the most extreme cases of sibling victimization which are associated with poor mental health and wellbeing – rather any exposure to sibling victimization may be harmful for later mental health and wellbeing. We posit that this is because sibling relationships, unlike those with peers, are difficult to escape from, enduring over childhood, meaning that even less extreme sibling victimization may have a detrimental effect on children’s mental health and wellbeing. Importantly, this notion contrasts with the general societal view of sibling violence as normal and harmless (Caspi, Reference Caspi2012), or even a rite of passage between siblings (Krienert & Walsh, Reference Krienert and Walsh2011).
Of concern, our sensitivity analyses indicated that, far from being a normal or harmless experience, sibling victimization was also associated with the most extreme form of self-harm, namely self-harm with suicidal intent, at age 17. This finding is in line with previous sibling victimization research in the ALSPAC cohort (Dantchev et al., Reference Dantchev, Hickman, Heron, Zammit and Wolke2019), as well as with findings from the peer victimization literature. For example, using data from the Quebec Longitudinal Study of Child Development, Geoffroy et al. (Reference Geoffroy, Boivin, Arseneault, Turecki, Vitaro, Brendgen, Renaud, Séuin, Tremblay and Côté2016) found evidence that peer victimization during adolescence was associated with a threefold increase in the likelihood of suicide attempt, over and above concurrent suicidality and prior mental health problems. One proposed explanation for this association is that experiencing victimization may trigger mental health problems or suicidality due to an interaction with genetic vulnerability to psychopathology (Geoffroy et al., Reference Geoffroy, Boivin, Arseneault, Turecki, Vitaro, Brendgen, Renaud, Séuin, Tremblay and Côté2016). It is possible that this is also the case with sibling victimization. There is also research to suggest that those who experience sibling victimization at home are more likely to experience peer victimization at school (Dantchev et al., Reference Dantchev, Hickman, Heron, Zammit and Wolke2019). When this is the case, it means that there is no safe place for these young people to escape to, thus increasing their risk of serious mental health problems, such a self-harm with suicidal intent.
In line with a socio-ecological approach to resilience, nearly all factors at the family, peer, school, and neighborhood level (measured at age 14 years) were uniquely associated with better or worse-than-expected mental health and wellbeing outcomes in expected directions at age 17 years. It is interesting to note that our results suggested that factors outside of the home might be especially important for children’s resilience to sibling victimization. Specifically, across all mental health and wellbeing outcomes, having higher levels of school motivation and engagement was significantly associated with better-than-expected outcomes. Having no close friend was significantly associated with worse-than-expected outcomes for internalizing problems, wellbeing, and self-harm. These findings suggest that aspects of the school environment might offer both risk and promotive factors for children experiencing sibling victimization at home. This might be because, depending on how the school environment is experienced by a young person, schools have the potential to either offer a respite from victimization occurring at home, or be an additional environment in which young people experience further stressors.
Whilst school motivation and engagement was associated with resilience across all mental health outcomes, having no close friend was associated with worse-than-expected levels of all outcomes, apart from externalizing problems. This might be because individuals with no close friend might be less likely to access the emotional and cognitive resources for support and coping which friends can offer (Hodges et al., Reference Hodges, Boivin, Vitaro and Bukowski1999), which might be more closely related to internalizing problems, general wellbeing, and self-harm. Additionally, there is heterogeneity in the behaviors which are classified as externalizing problems in the SDQ (more so than for internalizing problems), therefore, it is possible that having no close friend might be associated with some aspects of externalizing problems, but not others. However, as the internal reliability of the externalizing measure in this sample was low, these findings might also be due to a measurement effect, so caution is warranted when interpreting these findings.
At the neighborhood level, living in a neighborhood perceived as “very safe” (compared to a “not very safe” neighborhood) was also associated with better-than-expected outcomes for internalizing problems, externalizing problems (for girls), wellbeing and self-harm. In the case of sibling victimization, neighborhood safety might be a promotive factor associated with better-than-expected mental health outcomes, as living in a neighborhood perceived as “very safe” might offer enhanced support, beyond the family, for those experiencing victimization at home. This is in line with a multisystemic approach to resilience, which highlights that there are multiple, interacting systems (including, for example, at a neighborhood or community level) which promote resilience following adversity (Ungar & Theron, Reference Ungar and Theron2020). For example, a systematic review of resilience factors associated with positive mental health outcomes in adolescents, despite their exposure to adversity, found that at the community level (alongside individual and family factors), experiencing high levels of social support was associated with better outcomes (Fritz et al., Reference Fritz, De Graaff, Caisley, van Harmelen and Wilkinson2018).
Although this is one of the first studies to investigate the promotive and risk factors associated with resilience to sibling victimization, the parallels with the peer victimization literature are striking. For example, in terms of school factors, Armitage et al. (Reference Armitage, Wang, Davis, Collard and Haworth2021) found that greater perceptions of scholastic competence buffered against some of the risks associated with peer victimization. Therefore, it is possible that promotive factors at a school level for peer victimization might also extend to sibling victimization, even though this form of victimization occurs within the home. Findings are also in line with resilience research more broadly, suggesting that school enjoyment may be a characteristic of “resilient” adolescents (Fergusson & Lynskey, Reference Fergusson and Lynskey1996). The notion of parallels with the peer victimization literature is also seen in our other findings. For example, that having no close friends was a risk for worse mental health and wellbeing outcomes following sibling victimization, is consistent with findings from the peer victimization literature (Hodges et al., Reference Hodges, Boivin, Vitaro and Bukowski1999).
Peer, school, and neighborhood factors might also have been particularly influential for resilience in our study, due to the age of the sample (early adolescence). Hallmarks of development during this time include social networks becoming more extensive as adolescents become more aware of the views of others, and a greater importance placed on relationships with peers (Collins & Laursen, Reference Collins, Laursen, Hendrick and Hendrick2000). Adolescents also tend to become more concerned with other people’s perceptions of them (Steinberg, Reference Steinberg2005). At the same time, there is usually a declining dependence on parents (Collins & Roisman, Reference Collins, Roisman, A.Clarke-Stewart and Dunn2006). Changing interpersonal relationships during adolescence might therefore account for this study’s finding that factors outside of the home were especially important for resilience to sibling victimization.
An alternative explanation for the lack of effects at a family level may be because there are differential sources for reports on family level factors (the main caregiver) and factors outside the home (cohort member). For family level factors, research suggests adolescent and parent reports of family relationships rarely converge (De Los Reyes et al., Reference De Los Reyes, Ohannessian and Racz2019), and that adolescent reports may be more predictive of later adolescent outcomes (Abar et al., Reference Abar, Jackson, Colby and Barnett2015). The MCS does not include cohort member report for family level items such as parent-child relationships, so it might be that the lack of effects of factors inside the home, such as parent-child relationships, may simply reflect that main caregivers were not the optimal informants to use for these measures during adolescence. Relatedly, measures of parental monitoring and parental relationship were created for the purpose of this study, and it may be that they do not adequately capture these concepts.
In general, promotive factors were associated with better outcomes for the whole sample, which means that whilst these factors might be important for mental health in general, they are not more important for those who have experienced sibling victimization compared to children who have not. The exception is our finding for living in a neighborhood perceived as “very safe,” which was especially protective against internalizing problems among those who had experienced more frequent victimization, compared to those who experienced little or no sibling victimization. However, it should be noted that the interaction effect size is extremely small and requires replication, so should be interpreted with caution.
Strengths of our study include the use of a large, nationally representative cohort study, as this allows for inferences to be made about what the results mean for the wider UK population. Furthermore, the use of multiple, validated measures of mental health and wellbeing allows for results to be compared with other victimization studies which use these measures. We also controlled for a wide range of confounders, at both the individual and family level. A further strength is the inclusion of sibling victimization measures at two time points (age 11 and age 14 years), which allowed for the effects of sustained victimization (i.e., exposure to sibling victimization at both time points) to be explored.
Despite these considerable strengths, our study also has several limitations. Firstly, sibling victimization was assessed via one question only, which asked how often a sibling hurt or picked on the cohort member on purpose. Although the use of single item measures is common in large scale cohort studies, this does mean that some specificity is lost. For example, it was not possible to capture additional aspects of sibling victimization which might distinguish victimization from sibling conflict more generally, such as the type of bullying behavior (e.g., verbal, relational and/ or damage to property) and whether there might be a power imbalance between siblings (assessed by ascertaining the age difference between the siblings).
However, there is research to suggest that sibling victimization can be sufficiently captured using a single item measure. For example, Toseeb & Wolke (Reference Toseeb and Wolke2022) found a high correlation between single and multi-item assessments of sibling victimization in the ALSPAC cohort. Furthermore, our finding that nearly half of the sample reported being bullied by a sibling is in line with estimates from research which utilized a more comprehensive assessment of sibling victimization (Bowes et al., Reference Bowes, Wolke, Joinson, Lereya and Lewis2014).
Secondly, there is also loss to follow up from the original MCS sample. We took a conservative approach to missing data imputation, imputing to outcome (meaning that we imputed covariates, and risk and promotive factors in a sample with complete mental health outcome measures). Missing data analyses results show that those who did not provide full mental health and outcome data at age 17 were more likely to have experienced a range of early risk factors for poorer mental health in adolescence. This means that those who remained in the sample at age 17 were probably doing better overall, compared to those who do not complete the age 17 measures. Therefore, it is possible that the true effect of sibling victimization on mental health and wellbeing was underestimated in this study. Consequently, caution is warranted when generalizing findings beyond this sample.
A third limitation is that although the earliest time point at which sibling victimization is measured in the MCS is age 11 years, it is possible that sibling victimization occurred earlier than this and had effects on children’s mental health. This means that controlling for early mental health at age 7 years might have been an over-adjustment, as it is possible that early sibling victimization may have led to some early internalizing/ externalizing problems.
A further limitation is that for promotive factors which were assessed using a continuous scale, it is not known whether they had promotive effect on mental health due to the absence of risk (e.g., the lack of low motivation and engagement towards school) or the presence of something positive (e.g., a particularly high level of school motivation and engagement). One way to assess this would be to trichotomize the variable, which explores whether the higher, positive end of a variable is associated with lower mental health problems compared with the mid-range, and whether mid-range scores are associated with fewer problems than the lower “risky” end (Brumley & Jaffee, Reference Brumley and Jaffee2016). Although we planned to trichotomize continuous promotive factors, there were not enough observations in the higher and lower end of each variable to meaningfully split the data, so trichotomizing the variable was not possible.
Finally, there are some potential limitations to utilizing a residuals approach to measure resilience. This is because, as residuals will, by design, be highly correlated with psychosocial outcomes (Ioannidis et al., Reference Ioannidis, Askelund, Kievit and van Harmelen2020), it could be argued that measuring resilience using residuals is not meaningfully distinctive from the measurement of mental health outcomes themselves. However, as Ioannidis et al. (Reference Ioannidis, Askelund, Kievit and van Harmelen2020) note, this approach explicitly separates an individual’s resilient functioning from their mental health and wellbeing outcome score more clearly towards the more extreme ends of exposure to an adverse experience. For example, in the case of sibling victimization, two individuals could have a similar level of, for example, internalizing problems, but the individual with a history of frequent exposure to sibling victimization would have a higher level of resilience to internalizing problems, when compared to an individual exposed to a much lower level of sibling victimization. This highlights that a residuals approach to resilience can reveal important differences in the functioning of individuals following exposure to adversity.
Overall, our study contributes to a growing literature indicating that sibling victimization is a frequent and harmful experience and is associated with mental health and wellbeing problems over and above additional individual and family risk factors (Bowes et al., Reference Bowes, Wolke, Joinson, Lereya and Lewis2014; Sharpe et al., Reference Sharpe, Fink, Duffy and Patalay2021; Toseeb & Wolke, Reference Toseeb and Wolke2022). This highlights the need for researchers, clinicians, and policymakers to widen their focus from the detrimental effects of peer victimization to include sibling victimization. For example, traditionally, research assessing the effects of adverse childhood experiences (ACEs) on risk for experiencing mental health problems has focused on experiences that affect a child either directly (such as abuse and neglect), or indirectly through their living environment, (such as parental mental illness, domestic violence, or criminal behavior) (Felitti et al., Reference Felitti, Anda, Nordenberg, Williamson, Spitz, Edwards, Koss, Marks and Perma-Nente1998). More recent research has included peer victimization as an ACE (Houtepen et al., Reference Houtepen, Heron, Suderman, Tilling and Howe2018; Hughes et al., Reference Hughes, Bellis, Hardcastle, Sethi, Butchart, Mikton, Jones and Dunne2017), however there is no mention of sibling victimization. Our findings suggest ACEs assessments should also include measures of sibling victimization.
We also identified promotive and risk factors for better or worse mental health and wellbeing following sibling victimization. Identifying such factors is essential, as they represent potential targets for future interventions to support children who have experienced sibling victimization. Despite sibling victimization occurring in the home, our study demonstrates that factors associated with the wider environment are important for children’s resilience to sibling victimization. This is especially the case for higher levels of school motivation and engagement, which was the only factor predictive of better-than-expected functioning across all mental health and wellbeing outcomes (with small to medium effect sizes). Traditionally, peer and sibling relationships are treated as different issues, in terms of both theory and intervention. For example, peer victimization interventions typically focus on changing factors relating to the school environment. Although there are currently no interventions specifically for sibling victimization, interventions to improve sibling relationships more broadly focus solely on parenting (Leijten et al., Reference Leijten, Melendez-Torres and Oliver2021). However, this study suggests that school level interventions may have impacts beyond the school environment (something not traditionally measured in school-based interventions).
In conclusion, our study supports existing sibling victimization research, demonstrating that sibling victimization is a pervasive risk factor for experiencing enduring mental health and wellbeing problems. This is one of the first studies to investigate the promotive and risk factors associated with resilience to sibling victimization. Results suggest that there are a range of promotive and risk factors at the family, peer, school, and neighborhood level which are associated with better or worse mental health and wellbeing following sibling victimization. The most salient factor, associated with resilience across multiple mental health and wellbeing domains, was school motivation and engagement. Given both the prevalence and the negative outcomes associated with sibling victimization, our study highlights the need for interventions to promote resilience following sibling victimization. Results of our study suggest that future effective sibling victimization interventions should be extended to include a focus on factors outside of the home.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0954579423001323.
Acknowledgements
Elise Sellars is funded by the Economic and Social Research Council Grand Union Doctoral Training Partnership. We are grateful to the Study families for their participation.
Funding statement
This work was supported by the Economic and Social Research Council [grant number ES/P000649/1] (ES).
Competing interests
The author(s) declare none










