Although progress has been made in improving child nutritional status, undernutrition, in particular wasting and stunting remain public health challenges in Burkina Faso with more than 21·1 % of children under the age of 5 years classified as stunted, and 9 % of them suffering from wasting in 2019(1). In addition to poor maternal health and nutrition, inadequate infant and young child feeding practices, repeated infections such as malaria, diarrhoea, measles, and acute respiratory infection, food insecurity(Reference Stewart, Iannotti and Dewey2), access to child care and nutrition services represent important factors contributing to a child’s poor nutritional status in Burkina Faso. Historically, access to healthcare among children under 5 years was extremely low in Burkina Faso and user fees were identified as the most important barrier to healthcare use(Reference Ridde3,Reference Belaid and Ridde4) . User fees lead to reduced use of health services, delayed diagnosis and limited access to appropriate treatment for mothers and their children, which then contributes to increase morbidity and mortality among children under 5 years of age(5–Reference Bassani, Arora and Wazny10). As with other sub-Saharan African countries, Burkina Faso first experimented with user fee removal in September 2008(Reference Ridde, Queuille and Atchessi11) in the Sahel region of the country. User fee removal was coupled with management of malnutrition of children under 5 years of age, which included screening and treatment of acute malnutrition and providing free care to reduce exposure to repeated illnesses among children by facilitating access to health services(Reference Ridde, Queuille and Atchessi11,Reference Ridde, Haddad and Heinmuller12) . Health workers were trained and equipped to provide quality medical and nutritional care to children and pregnant and lactating women. The intervention also included activities related to health service quality improvement through training and supervision of health workers maternal and child health practices(Reference Ridde, Queuille and Atchessi11,Reference Ridde, Haddad and Heinmuller12) . The intervention was implemented by HELP NGO (non-governmental organisation) with the objective to encourage mothers to bring their children for care at the onset of symptoms and to increase utilisation of health facilities by all sick children, including the poorest and those living furthest away(Reference Ridde, Queuille and Atchessi11). The HELP intervention was integrated into the health system and maintained through a national policy that began in April 2016. Conceptually, user fee removal acts as an enabling factor, allowing users to make choices about their use of public healthcare services(Reference Robert, Samb and Marchal13). By removing financial barriers to healthcare access and improving the management of malnutrition at the community level, individuals and households will change their health-seeking behaviour as services become more affordable(Reference Robert, Samb and Marchal13,Reference Sen14) . Individuals will use healthcare services more often and more regularly and will seek care promptly(Reference Yates15,Reference Giedion, Andrés Alfonso and Díaz16) . Health is then improved through the regular use of health services(Reference Robert, Samb and Marchal13,Reference Giedion, Andrés Alfonso and Díaz16–Reference Rutherford, Mulholland and Hill18) . Other individual, community, and environmental-level factors including socio-economic status (SES) and illness severity may also modify the use of free health services(Reference Ridde, Haddad and Heinmuller12,Reference Mosley and Chen17,Reference von Lengerke, Gohl, Babitsch, Janssen, Swart and von Lengerke19) . Therefore, the theory of change is that by removing user fees and strengthening the management of the severe acute malnutrition without complications at the community level, it will increase child health services use which will then contribute to reducing child morbidity through the improvement of health status(Reference Ridde, Queuille and Atchessi11). Removing user fees have also been shown to have an indirect impact on the underlying proximal determinants of health by reducing catastrophic expenditures, a factor that impoverishes households. By enhancing the financial protection of households(Reference Ridde, Agier and Jahn20,Reference Illou, Haddad and Agier21) and thus releasing income, it reduces poverty and thereby contributes to improved food consumption(Reference Powell-Jackson, Hanson and Whitty22). Improved food consumption should then result in a positive impact on measures of child health status, particularly malnutrition, and generally reduce the risk of more frequent episodes of illness(Reference Giedion, Andrés Alfonso and Díaz16). Previous research in the context of our study concluded that as a public health intervention facilitating the use of health services, the presence of the intervention in the villages of the Sahel region in Burkina Faso resulted, 1 year after its implementation, in a substantial increase of use of health services(Reference Ridde, Haddad and Heinmuller12,Reference Johri, Ridde and Heinmuller23) that maintained over time(Reference Zombré, De Allegri and Ridde24). In addition, the intervention resulted in better financial protection of households against the financial risks associated with poor health(Reference Illou, Haddad and Agier21) and provided an empowering environment for women(Reference Samb and Ridde25).
User fee removal policies have been extensively evaluated for their impact on access to care(Reference Ridde and Morestin26), demonstrating that exempting children under 5 years of age from user fees increases and maintains the use of healthcare(Reference Zombré, De Allegri and Ridde27) and helps reduce inequities of access in both the short(Reference Ridde, Queuille and Atchessi11) and long term(Reference Zombré, De Allegri and Ridde27). However, studies on the relationship between user fee removal and child morbidity are scarce with mixed findings(Reference Ansah, Narh-Bana and Asiamah28,Reference Deininger and Mpuga29) . To date, the association between user fee removal and child nutritional status has been explored only in one randomised controlled trial in Ghana(Reference Powell-Jackson, Hanson and Whitty22) and no effect on child nutritional status was found. This study used a relatively short follow-up time from the user fee removal (1 year), which is likely too short to have had an effect on child nutritional status. Nutritional status measured by stunting reflects cumulative effects of poverty, poor maternal and early childhood nutrition, and repeated episodes of illness in childhood without access to healthcare(Reference de Onis and Branca30–32). Furthermore, as the exposure to user fee removals occur at the population level, logistic regression or simple multilevel analysis are insufficient to appropriately assess contextual effects(Reference Merlo, Wagner and Ghith33) which are important determinants of effectiveness. Though epidemiologists normally investigate the effect of an intervention as changes in group means, public health interventions may cause a change in the variance of the distribution of health outcomes(Reference Merlo, Ohlsson and Lynch34). In order to provide useful information to policymakers to tailor the implementation of public health intervention across different contexts, it is important to include both measures of variance and means measures of association when performing contextual analyses(Reference Merlo, Ohlsson and Lynch34).
Consequently, the rationale of our study is to better understand to what extent a public health intervention, which included user fee removal, quality of care improvement, and malnutrition management, affected the nutritional status of children under 5 years of age and influenced its disparity between communities in Burkina Faso. Specifically, we investigated whether living in intervention communities was associated with decreased likelihood of stunting and wasting among children under 5 years of age. We also investigated if the intervention as a specific community-level characteristic may account for the disparities in stunting and wasting between communities.
Methods
Context and intervention
In the specific context of the Sahel, one of the country’s most disadvantaged regions, high levels of morbidity and malnutrition coincide with very low healthcare use or lack of access to health services(35). In 2008, 20 % of children under 5 years of age were severely anaemic. The rates of stunting (46·1 %) and wasting (17·6 %) were the highest in the country, while vaccination coverage (65 % for all vaccinations) and use of health centres were the lowest (only 32 % of children used health services in case of illness). As in the rest of the country, respiratory infections, malaria, and diarrhoea are the leading causes of infant morbidity and mortality. Inequalities in access to care remain substantial. For example, 54 % of children with fever in wealthy families were treated in public health centres, while this proportion was only 22 % for children in poor families(Reference Gwatkin, Rutstein and Johnson36).
In 2006, as a consequence of a food crisis, humanitarian agencies started piloting a Community-Based Management of Acute Malnutrition (CMAM) approach in the country. The Red Cross of Belgium, an international NGO, in collaboration with the National Red Cross in Burkina Faso, started a CMAM programme in June 2007, and the handover to the Ministry of Health was planned for 2010 in the Sahel region.
In September 2008, based on the UNICEF’s conceptual framework on the determinant of malnutrition, the regional health authorities, in collaboration with a German NGO (HELP), implemented an intervention that aimed to improve access to healthcare in order to reduce the burden of malnutrition in this specific context. The promoters of the intervention rely on the assumption that improved access to healthcare services would enable better management of acute malnutrition (wasting) and management of recurrent illness episodes, ultimately resulting in improved outcomes for chronic malnutrition (stunting). With regard with stunting, increased use of maternal and child healthcare may increase uptake of preventive services and curative services, and, to some extent, child immunisation, deworming medication and for severe infectious diseases as malaria, diarrhoea, and acute respiratory infections. In addition, by avoiding perpetuating illnesses over a long period of time due to lack of access to healthcare, nutritional status can be protected. While the intervention does not directly target nutrition, the link between access to curative services and nutritional status is there (even in high-income settings).
The critical intervention activities were user fee removal intervention to improve access to quality child health services (nutrition sensitive) combined with the management of malnutrition for children under-5 years old, which included monitoring the children that were identified as being malnourished (nutrition specific intervention)(Reference Ridde, Queuille and Atchessi11,Reference Ridde, Haddad and Heinmuller12) . The intervention also included activities related to social mobilisation, health education, and improvement of service quality.
The principle of the intervention was to make care free of charge for pregnant women and children under 5 years of age and to encourage mothers to have their children treated earlier, as soon as the first symptoms of illness appeared, and thus increase the use of services by all sick children, including the poorest and most deprived. In addition, to achieve more convincing results in the fight against malnutrition, free services have been combined with the medical management of malnutrition in the community. Thus, children suffering from malnutrition are detected, then referred and cared for free of charge in the health centres covered by the intervention. As the intervention is population-based, it systematically reached all the children who use health services less and all the acute malnourished children detected in the community.
The NGO focused its efforts on two of the region’s four districts, Dori (290 000 inhabitants, 18 health centres in 2009) and Sebba (180 000 inhabitants, 11 health centres in 2009). The intervention was established to improve access to health services by subsidising 100 % of the care for children under 5 years of age, for pregnant women, and for nursing mothers. Prior to the intervention, patients visiting a health centre had to pay for the consultation ($0·20 USD), for drugs (varying costs depending on the prescription), and for care under observation ($0·60/d USD) if they were hospitalised in the primary health centre(Reference Ridde, Queuille and Atchessi11).
Study design
We conducted a non-equivalent control group post-test-only design(Reference Shadish, Cook and Campbell37,Reference Krishnan38) . A representative cross-sectional household survey was conducted 4 years after the intervention onset. The study group comprised households from 41 communities from intervention district (Dori) in which the intervention was ongoing for 4 years. The control group comprised of households from 51 communities from neighbouring district (Gorom) in which the intervention had not been implemented. Dori and Gorom were chosen as intervention and comparison districts respectively given the similarities of their contexts and in terms of public health intervention except for the presence of HELP intervention in Dori district. In particular, two studies on the effects of the user fee removal intervention on the use of child health services(Reference Zombré, De Allegri and Ridde24) and assisted childbirth(Reference Nguyen, Zombré and Ridde39) showed similar patterns of service utilisation in both groups before the onset of the intervention. However, data from the national health information system and the 2009 nutrition survey show that among the four districts in the region, the district of Dori and the district of Gorom-Gorom showed a slight difference the nutrition outcomes(40). Indeed, the rate of stunting was estimated at 45·8 % in Gorom-Gorom (95 % CI 40·6, 51·2) and 46·3 % in Dori (95 % CI 41 0, 51·6), while 13·8 % of children suffered from wasting in Gorom-Gorom (95 % CI 10·8, 17·5) compared to 15·6 % in Dori (95 % CI: 12·1, 19, 8)(41).
Sampling and data collection
We collected cross-sectional data on household demographic characteristics as well as on a wide range of health-seeking behaviours and health outcomes for children under 5 years of age. The sampling strategy was a stratified two-stage random probability sampling approach following the WHO’s Expanded Program on Immunization (EPI) Cluster Survey Design(Reference Ridde, Haddad and Heinmuller12). The primary sampling unit was defined as census enumeration areas, based on the 1998 census. We use the term ‘community’ to describe these small areas. During the first sampling stage, we randomly selected communities in the two districts for inclusion in the study with the probability of selection proportional to their population size. During the second stage, households were enumerated in each community and between 30 and 40 households were randomly selected(Reference Milligan, Njie and Bennett42). All children who were 6 to 59 months present in each selected household were systematically included.
Mothers or primary caregivers were interviewed to obtain information on details on the occurrence of illness episodes and related health service utilisation in the last 30 d. In addition, we obtained information on household socio-economic and demographic characteristics, as well as on nutritional and health factors.
We used trained nurses as interviewers and proven measurement techniques to collect anthropometric data and objective measures of anaemia and malaria in the intervention and control groups. We took anthropometric measurements (age, weight, height, mid-upper arm circumference) for children under 5 years of age (6–59 months). We measured recumbent length for children less than 2 years old and standing height for children age for 2 years and older. We used digital scale for weight measurement while height and length was measured using a wooden measuring board as is done in Demographic and Health Surveys (DHS) and as recommended by UNICEF(43). We defined anaemia status according to the level of Hb concentration; the presence of anaemia was defined as lower or equal to 110 g/l or upper and measured by a Hemocue photometer as recommended(Reference Chaudhary, Dubey and Sonker44). All children were tested for malaria, using a rapid diagnostic test (CareStart™ Malaria HRP2/pLDH (Pf/PAN). A child was diagnosed with malaria when the rapid diagnostic test was positive and body temperature was above 37°C.
As communities were selected based on probability proportional to the size of the population, households within communities were then selected with approximately equal probability, and all eligible children in a household were systematically selected, the overall probability of any child having been selected was approximately equal. This resulted in a self-weighting approach with no further weighting being later required at the stage of analysis(Reference Milligan, Njie and Bennett42).
Outcomes
As childhood wasting and stunting are the most common form of undernutrition in the study setting and because the intervention was designed to help improve child nutritional status, we used the anthropometric Z-score to capture stunting status.
We first calculated the anthropometric Z-score using Stata ZSCORE06 module on the basis of the WHO growth standards(Reference de Onis, Dewey and Borghi45). We then considered stunting and wasting in their severe and non-severe forms. Stunting and wasting were expressed as a Z-score of height for age and weight for height, less than 2 sd, while severe stunting and severe wasting were defined for the values of a Z-score of height for age and weight for height less than three standard deviations(Reference de Onis, Dewey and Borghi45). Z-scores of greater than 6 sd above or below the reference mean were removed from the sample(Reference Rutstein and Rojas46) as they were regarded as implausible values (data entry or measurement errors).
Exposure
As a population intervention, the intervention with all its components was deployed in all primary health facilities within each community in the same manner, so that all children under 5 years of age who are identified malnourished or those who actually use health services systematically benefit from the intervention.
However, due the high risk of recall and misclassification bias, it was not accurate to prospectively measure the intensity of exposure to the intervention for children under 5 years to distinguish those who continuously benefit from the intervention from those who did not. Our analysis aims to estimate the effect of a real-life programme to improve the use of child health and nutrition services in which some children in the intervention group may have not received the intervention and some would have using health services even in the absence of the programme.
Therefore, we defined exposure according to the geographical location of residence and it was considering an ecological-level exposure(Reference Morgenstern47,Reference Subramanian, Glymour and Kawachi48) .Thus, the exposure was defined by living or not in the intervention communities. As a matter of fact, social epidemiologists consider the place as a source of exposure at the global level(Reference Diez-Roux49), and several studies in the field of public health have considered residence in communities that have benefited from an intervention to assess its impact on health outcomes(Reference Melhuish, Belsky and Leyland50–Reference Hurtig and San Sebastián53).
Individual- and household-level predictors
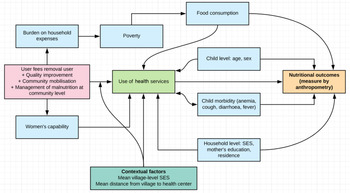
Based on the intervention theory(Reference Ridde, Queuille and Atchessi11), the framework developed by WHO(Reference Stewart, Iannotti and Dewey2) and UNICEF(32), we developed the potential pathways of impact for the intervention (Fig. 1) in order to select potential individual and household-level covariates relevant for the analysis.

Fig. 1 Potential pathways of impact for HELP intervention. SES, socio-economic status
We constructed bivariate relationships to examine the association of stunting across levels of categorical variables and we retained any variable whose univariable test had a P-value less than 0·20 along with all variables of known importance as identified by the literature(Reference Rakotomanana, Gates and Hildebrand54–Reference Corsi, Chow and Lear57). As a result, the following variables were included in the regression models: child age (from 6–11 months to 48–59 months), sex, mother’s education (if attended school or not), recent report of one of the following illness episodes: fever, cough or diarrhoea in the previous 30 d (yes/no), or anaemia (yes/no). In our conceptual framework (Fig. 1), we hypothesised an association between anaemia and stunting, and between stunting and the use of health services(Reference Rahman, Mushfiquee and Masud58). We also included household SES, type of residential area (rural or semi-urban), and community-level SES and measure of the distance. For the household distance measure, it represented the mean distance between each household and the health facility within a community. Indeed, in some communities, there were more households located more than 5 km away than households located less than 5 km away. Therefore, the impact of the distance may not be the same from one community to another. This implies that the average distance is a contextual factor that may differentially influence the use of health services and nutritional status.
We used an asset index as a proxy of household SES. This was computed using principal component analysis combining ownership of specific assets (cows, poultry, bicycle, motorbike and radio) and characteristics of the dwelling (type of source water, sanitation facilities and materials used for housing construction)(Reference Filmer and Scott59). Households were categorised as belonging to the lowest SES (< first quintile), middle SES (second to fourth quintiles) and highest SES (>fifth quintile).
Statistical analyses
Propensity score weighting
As the intervention was not randomly assigned; characteristics of communities, households and children living in the intervention district were likely to be different from those in the comparison district. We relied on generalised boosting modelling (GBM) propensity scores methods(Reference McCaffrey, Ridgeway and Morral60) to achieve balance in the distributions of selected covariates between the intervention and control groups. GBM is a non-parametric technique that allowed us to estimate the propensity score for the binary treatment indicator using a flexible estimation method that can adjust for a large number of pre-treatment covariates and complex functional forms(Reference McCaffrey, Ridgeway and Morral60,Reference Lee and Little61) . In practice, for each child in the intervention district, the propensity score was defined as the predicted probability of living in intervention communities as a function of individual, household and community-level confounders(Reference Pérez-Lu, Cárcamo and Nandi52,Reference Rosenbaum and Rubin62) . We fit the GBM using the package gbm, which was developed for the R statistical environment(Reference McCaffrey, Ridgeway and Morral60,Reference Lee and Little61) . All covariates which potentially related to the exposure and outcomes variables were included in the boosting models(Reference Lee and Little61). We ran the GBM algorithm using the standardized mean difference stopping rule to identify the iteration that minimises the average standardised mean differences(Reference McCaffrey, Ridgeway and Morral60). The minimum acceptable difference suggested in the literature ranges from 0·1 to 0·25 sd(Reference Lee and Little61,Reference Austin63,Reference Stuart, Lee and Leacy64) .
Investigation of the contextual effect of the intervention
To assess the relationship between intervention and nutritional status, we performed descriptive statistics and calculated the prevalence of individual nutritional status using the STATA statistical software package version 15.0 (StataCorp.). Given the multilevel structure of the data with children nested within households and households nested within communities, we used multilevel logistic regression analysis approach for our categorical outcomes. We used stabilisation procedures(Reference Robins, Hernan and Brumback65) to correct for the influence from children with extreme weights by multiplying inverse probability of treatment weights by a constant, equal to the expected value of receiving the treatment relative to what the child actually received(Reference Robins, Hernan and Brumback65). As recommended(Reference Lee and Little61), we incorporated the estimated propensity score as inverse probability of treatment weights into the two-level random intercept logistic regression model(Reference Lee and Little61) to assess the association between intervention and child nutritional status.
Multilevel analysis of disparities in stunting and wasting
We applied a two-step analytical strategy to distinguish the influence of the community context as a whole from the influence of the intervention as a specific contextual characteristic(Reference Merlo, Ohlsson and Lynch34).
We began by fitting a multilevel logistic regression including only the individual-level predictors and predicted the probability of stunting as function of individual characteristics(Reference Merlo, Wagner and Ghith33) and by incorporating community of residence as a random intercept. By quantifying the intra-class correlation (ICC)(Reference Merlo, Wagner and Ghith33), this model provides information on the proportion of the total individual variance in the propensity of stunting or wasting that can be found at the community level. We calculated the ICC using the latent variable method:
 $$ICC = \left[ {\frac{{{\sigma ^2}}}\over{{{\sigma ^2} +{ \frac{{{\pi ^2}}}\over{3}}}}} \right]*100,$$
$$ICC = \left[ {\frac{{{\sigma ^2}}}\over{{{\sigma ^2} +{ \frac{{{\pi ^2}}}\over{3}}}}} \right]*100,$$
where σ 2 is between-community variance and π 2/3 is the variance of the of standard logistic distribution.
In the second step of the analysis, we examined specific contextual effects of the intervention(Reference Merlo, Wagner and Ghith33) by addressing the question of whether living in an intervention community was associated with a reduced probability of stunting or wasting and to what extent the disparities in nutritional status were explained by the intervention. This helps with understanding the mechanism behind the observed general contextual effects. For this purpose, we included the exposure variable (living or not in communities which implemented user fee removal intervention) and calculated the adjusted ICC and the community-level variance explained by the presence of the intervention. The proportional change in variance defined as the proportion of the community-level variance was explained by adding the specific community effect (i.e. user fee removal) in the regression model(Reference Merlo, Wagner and Ghith33). A large proportional change in variance would inform us as to what extent the general contextual effect was substantially attributable to the community exposure to the user fee removal intervention combined with management of the malnutrition at the community level. We also estimated the Akaike information criterion to assess the goodness of fit of the different models. We reported estimated regression coefficients and OR by exponentiating the estimated regression coefficients as well as reporting model fit, Akaike information criterion and proportional change in variance. We also reported the estimates of the variance of the distribution of the random effects and statistical significance testing was conducted at the level of α = 0·05(Reference Merlo, Wagner and Ghith33).
Results
Propensity score weighting
Table 1 presents results of the test of balance in observables characteristics between intervention and comparison communities. Before weighting, the standardised mean differences were greater than 0·15 for 7 variables. After weighting, the values of the standardised mean difference were attenuated and fall to almost null for all covariates with values lower than 0·03, showing that the propensity score weighting successfully balanced intervention and comparison on observed covariates.
Table 1 Characteristics of children in the intervention and comparison group before and after balancing by propensity score

* std,eff,sz represents standardised effect size.
Sample characteristics
The study population consisted of 2421 children (aged 6 months to 59 months) from 92 communities (13 from semi-urban and 79 from rural areas), with an average of 30 children per community for a total of 1116 children from intervention communities and 1305 from control communities.
Table 2 shows the bivariate associations between the intervention, nutritional status, anaemia, illness episodes and the use of health services. Results shows that moderated stunted children were commonly from the intervention group (P < 0·03), whereas no difference was found in the prevalence of wasting between the two groups (P = 0·301). Additionally, the proportion of children who suffer from anaemia or illness episodes (P < 0·01) or had used health services (P < 0·001) is significantly higher in the intervention group compared to those in the comparison group (P < 0·001).
Table 2 Bivariate associations between the intervention, nutritional status, anaemia, illness episode and the use of health services

Effect of the intervention group on wasting and stunting
Table 3 shows the results of the mixed effects logistic regression model on the relationship between living in the intervention group and nutritional status. The results show that older children and those who experienced an illness episode and who suffer from anaemia are more likely to have poor nutritional status. In addition, the likelihood of stunting and wasting tend to reduce with the level of SES status. Finally, children from an educated mother and those from semi-urban areas are less likely to experience stunting compared to children living in rural areas or compared to those whose mothers are not educated. However, this relationship is not statistically significant for wasting.
Table 3 Multilevel logistic regression analysis of wasting stunting status in the children under 5 years of age

In addition, the results also show for children under 5 years of age, living in an intervention community was not associated with a reduced likelihood of stunting (OR = 1·13; 95 % CI 0·83, 1·54) nor with reduced likelihood of child wasting (OR = 1·21; 95 % CI 0·90, 1·64), while controlling for child and household-level characteristics. In addition, when comparing children living in the intervention district to children living in a non-intervention district in terms of severity (Table 4), we determined no differences in terms severely wasted (OR = 1·27; 95 % CI 0·79, 2·04) nor in severely stunted (OR = 0·99; 95 % CI 0·76, 1·26).

* Values for the comparison and intervention district are prevalence for severely stunted and severely wasted.
† We used a multilevel logistic regression analysis approach.
‡ All regressions include child age, sex, mother education level, SES, illness episodes in last month, anaemia, residential area and exposure to the intervention.
The analysis of the proportion of the variance explained by the context in general level and individual characteristics shows that 3 % of the variance of wasting (95 % CI 1·25, 10·42) and 9·4 % of the variance of stunting (95 % CI 6·45, 13·38) were due to systematic differences between communities of residence, while the remaining 90·6 % of the variance of stunting (95 % CI 86·6, 93·55) and 96·30 % of the variance of wasting (95 % CI 89·58, 98·75) was due to individual differences. This implies that the vast majority of the variance of stunting and mostly of wasting in children occurs at the individual level. Finally, in terms of influence of the intervention on the disparities of nutritional status, the results showed that presence of the intervention in the communities explains a very small proportion of a community’s level variance of stunting (2 %) and community’s level variance of wasting (3 %).
Discussion
We examined the contextual effects of a user fee removal intervention combined with healthcare quality improvement and malnutrition interventions, on child nutritional status and its variance at the community level. In our study, when comparing children living in the intervention district to children living in a non-intervention district, 4 years after the start of the intervention we found no statistically significant differences in terms of stunting and wasting, nor on their severity. We also determined that variance in stunting and wasting largely occurred at the individual level and only 2 % of the community-level variance of stunting and 3 % of the community-level variance of wasting was explained by the presence of the intervention in the communities.
A previous study determined that the intervention increased the use of services over the 4 years following the onset of the intervention(Reference Zombré, De Allegri and Ridde24). Despite this trend, this study estimated that the intervention was not associated with a reduction in the prevalence of chronic malnutrition among the children when compared to children living in non-intervention communities and also when compared to early intervention levels(41). This finding is in accordance with the results of a randomised controlled trial in Ghana(Reference Powell-Jackson, Hanson and Whitty22), which found that introducing free primary healthcare increased the use of healthcare but did not lead to measurable differences in any health outcome including children’s nutritional status after 1 year of follow-up.
Importantly, although we did not find a significant difference in nutritional status between the two groups, this does not mean that the intervention did not influence nutritional status. Despite the mean effect of the intervention being non-significant, the intervention affected the variance in nutritional status, which suggests the intervention may have had a positive impact on children’s nutritional status in some communities that our study design did not allow us to identify. In addition, it is worth noting that the CMAM has several components and the implementation of its various components may vary according to geography and implementers. While the intervention under study is being implemented in both groups, it is possible that CMAM may be effective in reducing the rate of undernutrition at the community level in both intervention and control communities, thus masking or reducing the impact of the other intervention components.
Furthermore, the lack of effect could be related to the study design and the difficulty to prospectively measure the intensity of exposure to the intervention for children under 5 years to distinguish those who continuously benefit from the intervention from those who did not.
While studies on determinants associated with child nutrition have traditionally focused on individual-level factors(Reference Akombi, Agho and Hall66,Reference Beiersmann, Bermejo Lorenzo and Bountogo67) ; our research demonstrates the importance of considering the influence of the community environment and the influence of the intervention as specific community-level factor on the distribution of nutritional status among children under 5 years of age. Our results are consistent with studies in Nigeria(Reference Adekanmbi, Kayode and Uthman55) and Bangladesh(Reference Corsi, Chow and Lear57) that differentiated between contextual and individual effects on the likelihood of stunting and wasting. These studies found that 8·5 % of the variance of height for age in Bangladesh and 8·7 % of stunting in Nigeria, respectively, were influenced by residential contexts(Reference Adekanmbi, Kayode and Uthman55,Reference Corsi, Chow and Lear57,Reference Mejía-Guevara, Corsi and Perkins68) that included context-specific public health and many other ecological-level exposures(Reference Morgenstern47,Reference Subramanian, Glymour and Kawachi48) . Those effects can be dissociated from the effect of the general residential context. Thus, we also estimated that 2 % of the variance of stunting and 3 % of the variance of wasting in communities were associated with the presence of the intervention in those communities. Though epidemiologists normally investigate effect of intervention as changes in group means(Reference Merlo, Ohlsson and Lynch34), our results show that the presence of the intervention was associated to some extent with the variance of the distribution of wasting and stunting in the communities. From a public health perspective, this result provides important information about the potential effect of the intervention combining free care with the management of undernutrition in community level on nutritional status.
Despite the use of advanced epidemiological analysis methods and anthropometric measurement tools recommended by UNICEF and WHO(43), our study has several limitations that must be considered when interpreting the results. The lack of effect of nutritional status could be explained by an insufficient study design, the propensity score adjustment, or from measurement error. With regard with measurement error, specifically given the nature of the intervention as the exposure variable was based on an ecological measure, which may have led to misclassification of exposure of individuals as we defined the area of residence. However, social epidemiologists often consider the site to be a source of exposure at the global level and several studies in the public health field have considered residence in intervention communities to assess the impact of public health interventions(Reference Melhuish, Belsky and Leyland50–Reference Hurtig and San Sebastián53). Secondly, we were unable to account for the prevalence of illnesses and height of the mother, as these variables were not collected. These data exclusion has likely resulted in residual confounding and would have diluted the intervention effects(Reference Fewell, Davey Smith and Sterne69). Thirdly, we were not able to collect baseline data from the two districts given the rapidity of the intervention implementation. Our cross-sectional study design does not allow for the evaluation of secular trends and pre-existing differences in child nutritional status. A difference-in-difference or regression discontinuity analysis using the data over a longer period is the next natural step, using regularly collected data such as the DHS data. Finally, in this study, we did not show whether the intervention was associated with the increase in the use of the healthy service at community level, nor did we analyse the trend of nutritional status before the intervention onset. This perspective of simultaneous evaluation of the effect of the intervention on health service utilisation and nutritional status would require the use of complex analytical methods, such as mediation analyses(Reference MacKinnon and Pirlott70) or structural equations modelling(Reference Beran and Violato71) with longitudinal data, but unfortunately the data we collected do not lend itself to such analyses.
Conclusion
Our study was not able to conclude that living in the intervention group was significantly associated with a reduced likelihood of stunting and wasting among children under 5 years of age in the Sahel region in Burkina Faso. However, combining free care with community-based management of undernutrition affects the variance of children’s nutritional status suggesting the intervention may have improved nutritional status in some communities. With the scaling-up of the national free health policy in Burkina Faso in June 2016, our study has shown the relevance of an intervention combining user fee removal interventions and management of malnutrition at the community level to increase the use of health services. However, as the intervention affected the variance of nutritional status at community level and given that the vast majority of the variance of stunting and wasting in children occurs at the individual level, if combined with tailored nutrition-specific interventions that target the proximal determinants of malnutrition, user fees removal intervention could act as an important contextual factor catalysing the impact of nutrition-specific interventions. The scaling-up of the national free health policy offers an exceptional opportunity to evaluate the effects of the user fee removal intervention more than 10 years after its initial introduction. This evaluation would provide decisions-markers further information to inform nutrition-specific interventions.
Acknowledgements
Acknowledgements: The authors thank the managers and the staff of the intervention studied (HELP), the health district authorities in Dori, Gorom-Gorom, Djibo and Sebba, the community leaders and beneficiaries in the areas studied, as well as the health workers for their collaboration in this study. A special thanks to Isabelle Agier and Moussa Bougma and the interviewers for assistance with the household survey data collection and entry. Finally, the authors would like to thank to Yves martin-prevel and Helene Deslile for their sound contribution to the revision of the manuscript. Financial support: This research was funded by the Humanitarian Aid Service (ECHO) of the European Commission and the Fonds de Recherche en Santé du Québec (FRSQ). DZ was supported by the Quebec Health Research Fund (FRQS) and IDRC (International Development Research Center) for data collection. The funding bodies and the NGO had no role in study design, data collection and analysis. Conflict of interest: The authors declare that they have no conflicts of interest. Authorship: V.R. and D.Z. prepared and supervised the field surveys. D.Z. supervised data management processes and conducted the primary analyses, led the analyses and drafted the manuscript in consultation with other authors. D.Z., M.A., K.Z. and V.R. interpreted the results and critically reviewed, improved and approved the final version of the manuscript. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects/patients were approved by Ministry of Health of Burkina Faso and ethics committees in Burkina Faso and The Centre de recherche du Centre Hospitalier de l’Université de Montréal (CRCHUM). Verbal consent was witnessed and formally recorded.