Book contents
- Psychotherapy for Bipolar Disorders: An integrative approach
- Psychotherapy for Bipolar Disorders
- Copyright page
- Contents
- Collaborators
- Preface
- Part 1 An Introduction to Treatments
- Part 2 The Foundations of an Integrative Approach to Bipolar Disorders
- Part 3 An Integrative Approach to Bipolar Disorders
- Book part
- Bibliography
- Index
- References
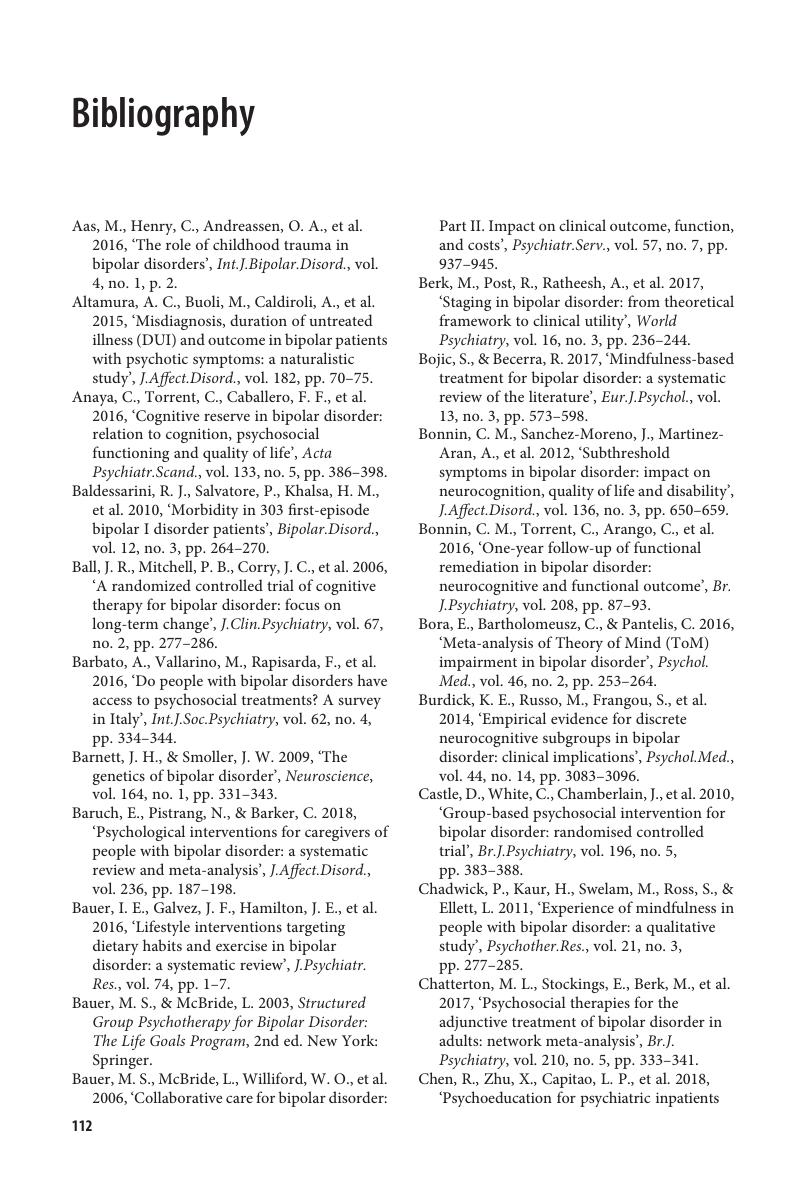
Bibliography
Published online by Cambridge University Press: 18 October 2019
- Psychotherapy for Bipolar Disorders: An integrative approach
- Psychotherapy for Bipolar Disorders
- Copyright page
- Contents
- Collaborators
- Preface
- Part 1 An Introduction to Treatments
- Part 2 The Foundations of an Integrative Approach to Bipolar Disorders
- Part 3 An Integrative Approach to Bipolar Disorders
- Book part
- Bibliography
- Index
- References
Summary
- Type
- Chapter
- Information
- Psychotherapy for Bipolar DisordersAn Integrative Approach, pp. 112 - 119Publisher: Cambridge University PressPrint publication year: 2019