Book contents
- Management of Complex Treatment-Resistant Psychotic Disorders
- Management of Complex Treatment-Resistant Psychotic Disorders
- Copyright page
- Contents
- Contributors
- Acknowledgements
- Abbreviations
- List of Icons
- Introduction
- Part I Treatment Strategies
- Part II Medication Reference Tables
- Appendices
- 3.01 Appendix Optimal Antipsychotic Plasma Concentration Ranges [–]
- 3.02 Appendix Optimal Mood Stabilizer Plasma Concentration Ranges [, ]
- 3.03 Appendix Formulas for Correcting QT Interval [, ]
- 3.04 Appendix Common Cytochrome P450 Inducers and Inhibitors [, ]
- 3.05 Appendix Management of Constipation [, ]
- 3.06 Appendix Child-Pugh Hepatic Function Scoring [, ]
- 3.07 Appendix Loading of Lithium and Valproic Acid [–]
- 3.08 Appendix Treatment of Prolactin Elevation [–]
- 3.09 Appendix A Select List of Foods High in Tyramine [–]
- 3.10 Appendix Medications That Present Risk for Serotonin Syndrome When Combined with Monoamine Oxidase Inhibitor [–]
- 3.11 Appendix Selected Treatment of Psychomotor Agitation Algorithm [–]
- Index
- References
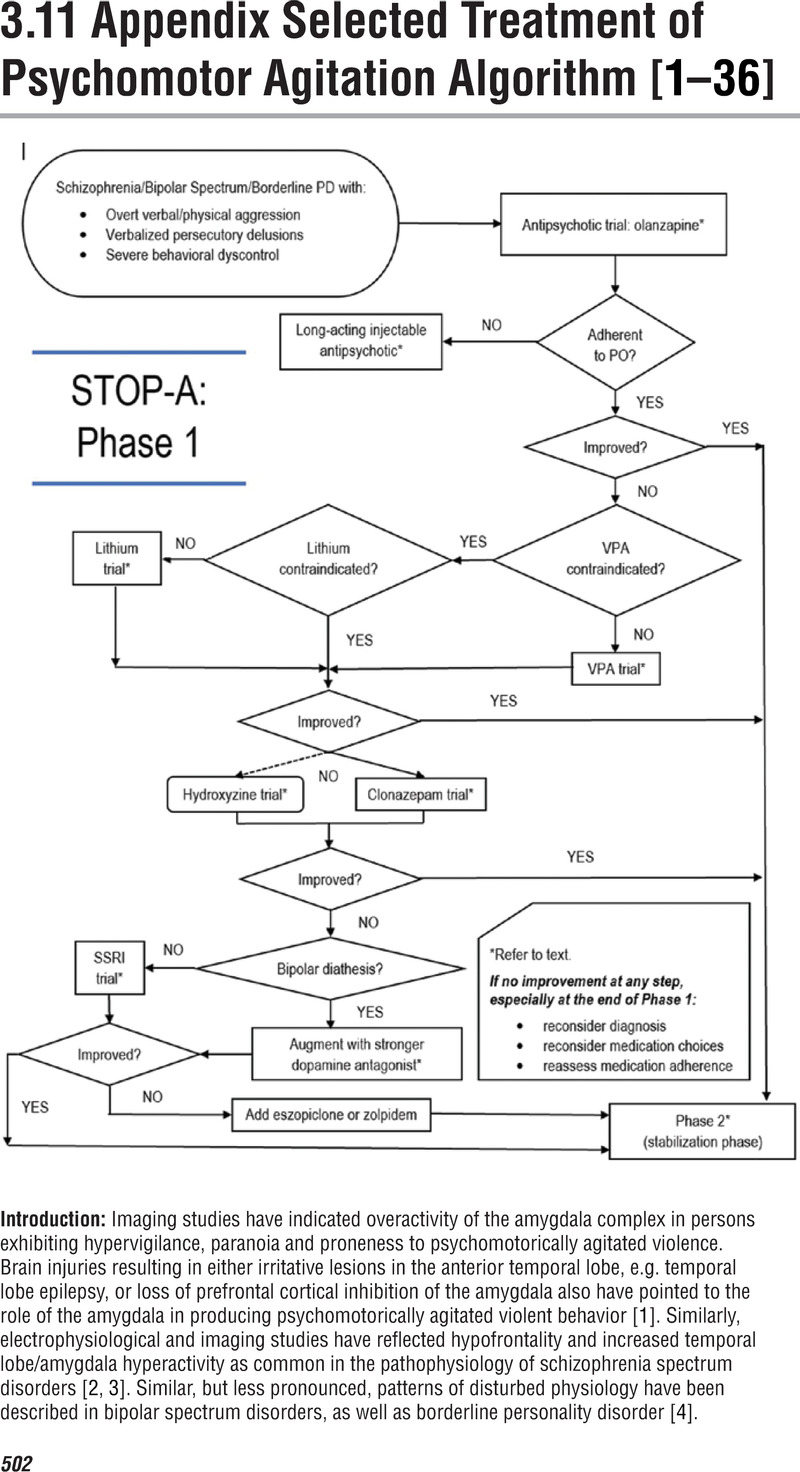
3.11 Appendix - Selected Treatment of Psychomotor Agitation Algorithm [–]
from Appendices
Published online by Cambridge University Press: 19 October 2021
- Management of Complex Treatment-Resistant Psychotic Disorders
- Management of Complex Treatment-Resistant Psychotic Disorders
- Copyright page
- Contents
- Contributors
- Acknowledgements
- Abbreviations
- List of Icons
- Introduction
- Part I Treatment Strategies
- Part II Medication Reference Tables
- Appendices
- 3.01 Appendix Optimal Antipsychotic Plasma Concentration Ranges [–]
- 3.02 Appendix Optimal Mood Stabilizer Plasma Concentration Ranges [, ]
- 3.03 Appendix Formulas for Correcting QT Interval [, ]
- 3.04 Appendix Common Cytochrome P450 Inducers and Inhibitors [, ]
- 3.05 Appendix Management of Constipation [, ]
- 3.06 Appendix Child-Pugh Hepatic Function Scoring [, ]
- 3.07 Appendix Loading of Lithium and Valproic Acid [–]
- 3.08 Appendix Treatment of Prolactin Elevation [–]
- 3.09 Appendix A Select List of Foods High in Tyramine [–]
- 3.10 Appendix Medications That Present Risk for Serotonin Syndrome When Combined with Monoamine Oxidase Inhibitor [–]
- 3.11 Appendix Selected Treatment of Psychomotor Agitation Algorithm [–]
- Index
- References
Summary
- Type
- Chapter
- Information
- Management of Complex Treatment-resistant Psychotic Disorders , pp. 502 - 507Publisher: Cambridge University PressPrint publication year: 2021