184 results
Natural Language Processing (NLP) Accurately Identifies LTCF Exposure from Clinical Notes: A Proof-of-Principle Study
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 4 / Issue S1 / July 2024
- Published online by Cambridge University Press:
- 16 September 2024, pp. s13-s14
-
- Article
-
- You have access
- Open access
- Export citation
CLABSIs aren’t just for inpatients: the need to identify CLABSI burden among outpatients
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 4 / Issue 1 / 2024
- Published online by Cambridge University Press:
- 12 September 2024, e132
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Chlorhexidine gluconate skin levels and organism decolonization: what we know and what we don’t know
-
- Journal:
- Infection Control & Hospital Epidemiology , First View
- Published online by Cambridge University Press:
- 08 August 2024, pp. 1-2
-
- Article
- Export citation
Healthcare personnel opinions regarding the feasibility of a risk-tailored approach to contact precautions for methicillin-resistant Staphylococcus aureus in the acute care setting
-
- Journal:
- Infection Control & Hospital Epidemiology , First View
- Published online by Cambridge University Press:
- 22 April 2024, pp. 1-3
-
- Article
- Export citation
A multi-center validation of the electronic health record admission source and discharge location fields against the clinical notes for identifying inpatients with long-term care facility exposure
-
- Journal:
- Infection Control & Hospital Epidemiology , First View
- Published online by Cambridge University Press:
- 18 April 2024, pp. 1-6
-
- Article
- Export citation
Research agenda for transmission prevention within the Veterans Health Administration, 2024–2028
-
- Journal:
- Infection Control & Hospital Epidemiology , First View
- Published online by Cambridge University Press:
- 11 April 2024, pp. 1-10
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Factors associated with patient-to-healthcare personnel (HCP) and HCP-to-subsequent patient transmission of methicillin-resistant Staphylococcus aureus
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 45 / Issue 5 / May 2024
- Published online by Cambridge University Press:
- 18 January 2024, pp. 583-589
- Print publication:
- May 2024
-
- Article
- Export citation
Alcohol-based decontamination of gloved hands: A randomized controlled trial
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 45 / Issue 4 / April 2024
- Published online by Cambridge University Press:
- 23 November 2023, pp. 467-473
- Print publication:
- April 2024
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
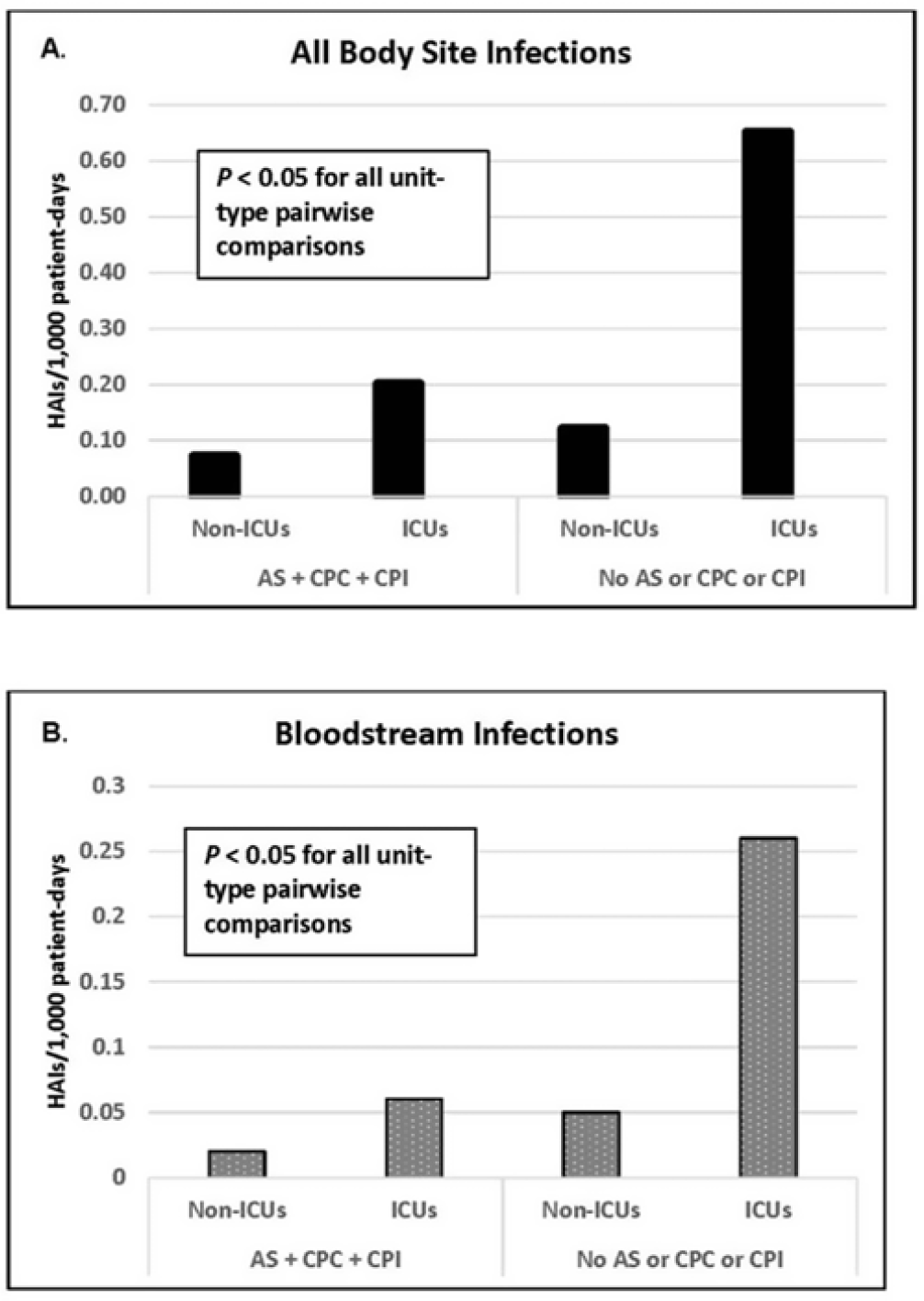
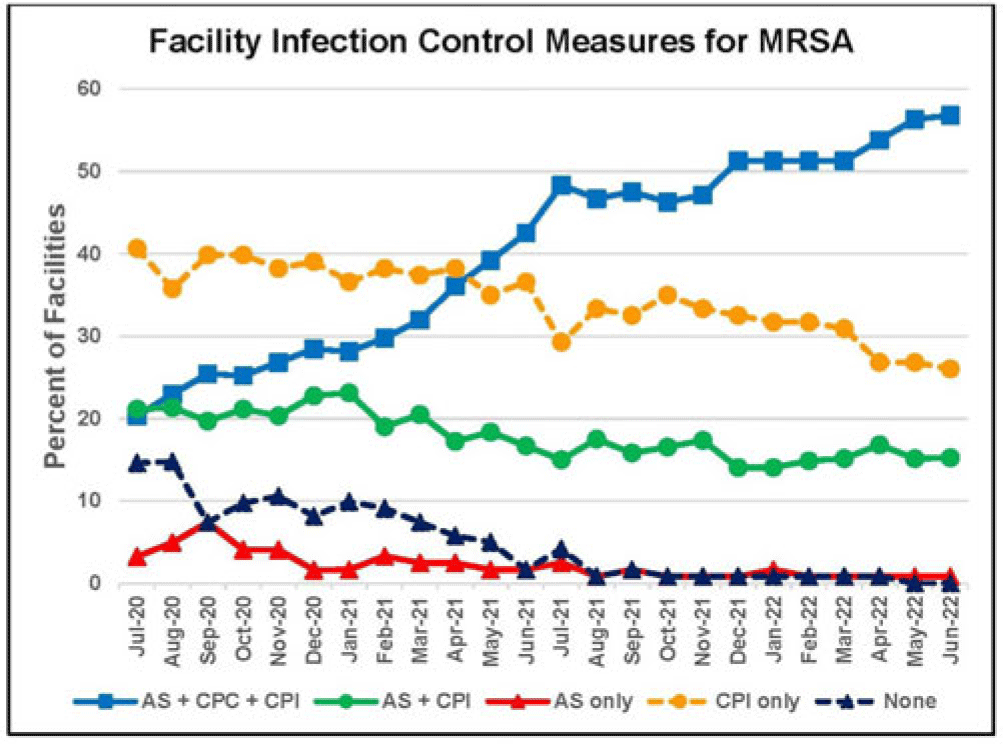
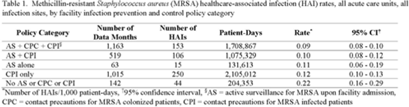
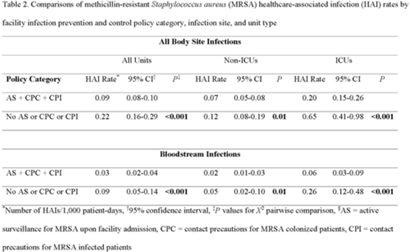
Active surveillance and contact precautions for preventing MRSA healthcare-associated infections during the COVID-19 pandemic
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 3 / Issue S2 / June 2023
- Published online by Cambridge University Press:
- 29 September 2023, pp. s117-s118
-
- Article
-
- You have access
- Open access
- Export citation
Evidence of housing instability identified by addresses, clinical notes, and diagnostic codes in a real-world population with substance use disorders
-
- Journal:
- Journal of Clinical and Translational Science / Volume 7 / Issue 1 / 2023
- Published online by Cambridge University Press:
- 04 September 2023, e196
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Developing a diagnosis calculator to estimate the probability of bacterial pneumonia
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 3 / Issue 1 / 2023
- Published online by Cambridge University Press:
- 07 August 2023, e137
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Efficacy of a continuously active disinfectant wipe on the environmental bioburden in the intensive care unit: A randomized controlled study
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 44 / Issue 12 / December 2023
- Published online by Cambridge University Press:
- 03 July 2023, pp. 2036-2043
- Print publication:
- December 2023
-
- Article
- Export citation
SHEA/IDSA/APIC Practice Recommendation: Strategies to prevent methicillin-resistant Staphylococcus aureus transmission and infection in acute-care hospitals: 2022 Update
- Part of
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 44 / Issue 7 / July 2023
- Published online by Cambridge University Press:
- 29 June 2023, pp. 1039-1067
- Print publication:
- July 2023
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Comparison of two swab types for recovery of Staphylococcus aureus and Candida auris from gloves and gowns
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 44 / Issue 11 / November 2023
- Published online by Cambridge University Press:
- 04 May 2023, pp. 1870-1872
- Print publication:
- November 2023
-
- Article
- Export citation
Diagnostic stewardship to support optimal use of multiplex molecular respiratory panels: A survey from the Society for Healthcare Epidemiology of America Research Network
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 44 / Issue 11 / November 2023
- Published online by Cambridge University Press:
- 02 May 2023, pp. 1823-1828
- Print publication:
- November 2023
-
- Article
- Export citation
Contact precautions for the control of endemic pathogens: Finding the middle path
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 3 / Issue 1 / 2023
- Published online by Cambridge University Press:
- 24 March 2023, e57
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Infection prevention and antibiotic stewardship program needs and practices in 2021: A survey of the Society for Healthcare Epidemiology of America Research Network
- Part of
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 44 / Issue 6 / June 2023
- Published online by Cambridge University Press:
- 14 March 2023, pp. 948-950
- Print publication:
- June 2023
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Comorbidities associated with 30-day readmission following index coronavirus disease 2019 (COVID-19) hospitalization: A retrospective cohort study of 331,136 patients in the United States
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 44 / Issue 8 / August 2023
- Published online by Cambridge University Press:
- 03 October 2022, pp. 1325-1333
- Print publication:
- August 2023
-
- Article
- Export citation
Molecular concordance of methicillin-resistant Staphylococcus aureus isolates from healthcare workers and patients
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 44 / Issue 4 / April 2023
- Published online by Cambridge University Press:
- 30 September 2022, pp. 578-588
- Print publication:
- April 2023
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Social Networks among Indigenous Peoples in Mexico
-
- Journal:
- Latin American Research Review / Volume 45 / Issue 2 / 2010
- Published online by Cambridge University Press:
- 05 September 2022, pp. 49-67
-
- Article
-
- You have access
- Export citation