Psychiatry requires highly specialised clinical skills that are necessary to evaluate individual-level abnormalities in experiences and behaviours, and interpret these as core symptomatology to guide diagnosis and treatment. Unlike the majority of other medical specialties, the challenge in psychiatry is to make such evaluations based on observation of these behaviours and experiences alone, given the absence of clinically relevant biological measures in psychiatry. In this editorial I will first discuss how neuroimaging methodologies can identify measures of neural circuitry that support cognitive and emotional processes known to be dysfunctional in psychiatric disorders, and how such methodologies can provide insight into neural mechanisms that may underlie the development of different psychiatric disorders across the lifespan. I will then highlight how these methodologies, by identifying measures of abnormal neural circuitry in individuals with a given psychiatric disorder, have potential to: (1) aid in differential diagnosis in otherwise difficult clinical contexts, for example distinguishing between bipolar and unipolar depression; (2) help provide information regarding likely future risk of developing psychiatric illnesses in at-risk populations; and (3) help identify individuals with a given psychiatric disorder who are most likely to respond to a specific treatment. I will then discuss how machine learning, in combination with different neuroimaging methodologies, can provide clinically useful measures of neural structure and function at the individual level, that have potential to be translated into clinical practice.
Neuroimaging: identifying ‘neural profiles’ of major psychiatric disorders
Early neuroimaging studies in psychiatry included technologies employing radioligand techniques (e.g. positron emission tomography and single-photon emission tomography) to measure neurotransmitter receptor binding potential and quantify regional density of receptors of a given type, and receptor binding displacement during pharmacological or physiological challenge, to quantify endogenous neurotransmitter release. These techniques can also quantify metabolism or blood flow in different neural regions. The expense and exposure to radioligands inherent in these techniques limits their use to specialised neuroimaging centres, although they continue to have utility in psychiatry, particularly in quantification of regional receptor density and synaptic function. Reference Otte1
Magnetic resonance imaging (MRI) includes well-established neuroimaging methodologies that have been developed to examine the functional and structural integrity of whole brain and regional neural circuitry. Functional MRI (fMRI) and structural MRI are probably the most widely used of these methodologies. Functional MRI examines changes in blood oxygen level-dependent (BOLD) signal, a proxy measure of neural activity, and is used to measure the functional integrity of neural circuitry. Structural MRI measures brain and regional grey and white matter volumes. Diffusion tensor imaging measures at the macroscopic level the extent of myelination of white matter fibres Reference Mori and Zhang2 using fractional anisotropy, a measure of the degree and directionality of diffusion of water molecules. More recent advances in diffusion tensor imaging include deterministic Reference Tournier, Mori and Leemans3 and global probabilistic Reference Jeurissen, Leemans, Jones, Tournier and Sijbers4 tractography, quantitative and more probabilistic measures respectively, of connectivity between reconstructed white matter fibres. Resting-state connectivity is another emerging neuroimaging technology that measures low-frequency (<∼0.1 Hz) BOLD fluctuations in distant, but apparently functionally related, grey matter regions at rest. Reference Biswal, Yetkin, Haughton and Hyde5 Arterial spin labelling is a non-invasive perfusion MRI methodology used to quantify cerebral blood flow. Reference Liu, Uh and Lu6 Importantly, these different MRI techniques can all provide information about the functional and structural integrity of neural circuitry – ‘neural profiles’ – in healthy and psychiatrically unwell individuals. For example, an increasingly large literature highlights how combinations of these different techniques can help identify specific functional, grey matter volumetric and white matter connectivity abnormalities in neural circuitry supporting emotion processing and regulation in individuals with unipolar depression, bipolar disorder and schizophrenia. Reference Phillips, Ladouceur and Drevets7,Reference Taylor, Kang, Brege, Tso, Hosanagar and Johnson8 Other studies indicate abnormal resting-state functional connectivity in the self-referential processing ‘default mode network’ in different psychiatric disorders, including unipolar depression; Reference Sheline, Price, Yan and Mintun9 and abnormal resting perfusion in emotion regulation neural regions, measured with arterial spin labelling, in mood disorders. Reference Duhameau, Ferre, Jannin, Gauvrit, Verin and Millet10
Limitations and newer approaches to address clinically important challenges
There are several limitations of neuroimaging studies in psychiatry. These include the fact that the majority of such studies were conducted with small sample sizes, and have inconsistent findings; many focused on directly comparing a single psychiatric population with a healthy population rather than differentiating between psychiatric populations that are difficult to distinguish clinically; and the lack of quantitative measures provided by these studies for use in clinical practice. Thus, it has not been possible for findings from these studies to be translated easily into psychiatric practice, where clinical challenges regarding diagnosis, risk assessment and treatment decisions are myriad. Three very promising approaches in psychiatric neuroimaging are beginning to bring developments in neuroimaging methodologies into clinical practice to meet these challenges.
The first approach is the use of neuroimaging to help differentiate between individuals with different, but similarly presenting, psychiatric illnesses, for example unipolar v. bipolar depression. Recent studies reported that measures of functional and white matter integrity of emotion regulation neural circuitry can differentiate adults with unipolar depression from those with bipolar depression. Reference Almeida, Versace, Mechelli, Hassel, Quevedo and Kupfer11,Reference Versace, Almeida, Quevedo, Thompson, Terwilliger and Hassel12 These findings suggest that neuroimaging measures may be able to distinguish types of depression that are often extremely difficult to differentiate in clinical practice, especially in the absence of a clear history of mania.
The second approach is to use neuroimaging to help identify measures that predict the future development of psychiatric disorders. Unfortunately, there are no known biological measures that accurately predict the future development of psychiatric disorders in at-risk individuals, including children, adolescents and adults who are at genetic risk of future psychiatric disorders. Magnetic resonance imaging studies in at-risk populations are beginning to identify neuroimaging measures shared with affected relatives, which in turn may denote likely future risk of illness in these – and independent groups of – at-risk individuals. For example, studies suggest that neuroimaging methodologies can be used to clinically stage progression towards schizophrenia and illness severity. Reference Wood, Yung, McGorry and Pantelis13 Other findings indicate that healthy child and adolescent offspring of parents with bipolar disorder have patterns of white matter connectivity in key tracts implicated in emotion regulation Reference Versace, Ladouceur, Romero, Birmaher, Axelson and Kupfer14 that parallel patterns shown by adults with bipolar disorder. Reference Versace, Almeida, Quevedo, Thompson, Terwilliger and Hassel12
A third approach is the evaluation of the extent to which neuroimaging measures may predict, moderate and mediate differential treatment response. This approach allows identification of biologically relevant measures reflecting underlying neural mechanisms of illness that are antecedents of eventual outcome, and has promise to provide measures that, together with clinical information, are likely to be more accurate predictors of future treatment response than use of clinical measures alone. Studies have, for example, shown that measures of function in key neural regions supporting emotion regulation may be accurate predictors of response to selective serotonin reuptake inhibitor (SSRI) antidepressants in unipolar depression. Reference Pizzagalli15
These findings suggest that neuroimaging measures, either alone or in combination with clinical measures, may prove to be more accurate than clinical measures alone in differentiating different psychiatric disorders, identifying at-risk individuals at greatest future risk of psychiatric illness, and predicting future treatment response, although further studies are clearly needed to directly examine the extent to which this is the case.
Machine learning
Although studies adopting these three approaches are limited by small sample sizes, use primarily of only one neuroimaging technology (predominantly fMRI), and by the inability to test findings in independent groups of individuals, findings from these studies nonetheless represent an extremely important first stage towards employing neuroimaging methodologies to help address key clinical challenges in psychiatry. In addition to addressing these limitations, if psychiatric neuroimaging studies are to be of clinical use, their findings also need to translate into clinical practice at an individual, case-by-case level. An exciting approach that has potential to do just this is the employment of machine learning, together with different neuroimaging methodologies. Machine learning techniques, such as support vector machine learning, use pattern recognition to classify individuals, case by case, into different groups based on multivariate data-sets.
For example, studies reported that patterns of whole brain neural activity to emotional faces can help differentiate, at the individual level, individuals with unipolar depression from those who were healthy, Reference Fu, Mourao-Miranda, Costafreda, Khanna, Marquand and Williams16 and individuals with bipolar depression from those with unipolar depression. Reference Mourao-Miranda, Almeida, Hassel, de Oliveira, Versace and Marquand17 Machine learning and fMRI measures of whole brain activity to neutral faces also discriminated healthy low-risk adolescents from healthy adolescents genetically at-risk for mood and anxiety disorders, by virtue of having a parent with bipolar disorder, at 75% accuracy. Exploratory analyses revealed that those at-risk individuals who were more confidently classified as belonging to the at-risk group, were more likely to develop a psychiatric disorder up to 4 years later. Reference Mourao-Miranda, Oliveira, Ladouceur, Marquand, Brammer and Birmaher18 Future studies can thus take advantage of the very promising opportunities afforded by employing combinations of machine learning and MRI methodologies to help improve individual-level diagnosis, identify individual-level risk of future psychiatric disorder, and ultimately determine individual-level likelihood of responding to a given treatment (Fig. 1).
The next steps for neuroimaging studies employing machine learning and other techniques clearly involve replication of findings in independent testing samples across different laboratories and scanners to identify the most robust paradigms and measures to meet the above clinical challenges. Critically, given the high prevalence and related societal cost of psychiatric illnesses worldwide, Reference Collins, Patel, Joestl, March, Insel and Daar19 the increased financial cost of including neuroimaging assessments in clinical settings may be more than offset by the significant improvements in mental health and related reductions in longer-term healthcare costs brought by neuroimaging assessments that meet these clinical challenges.
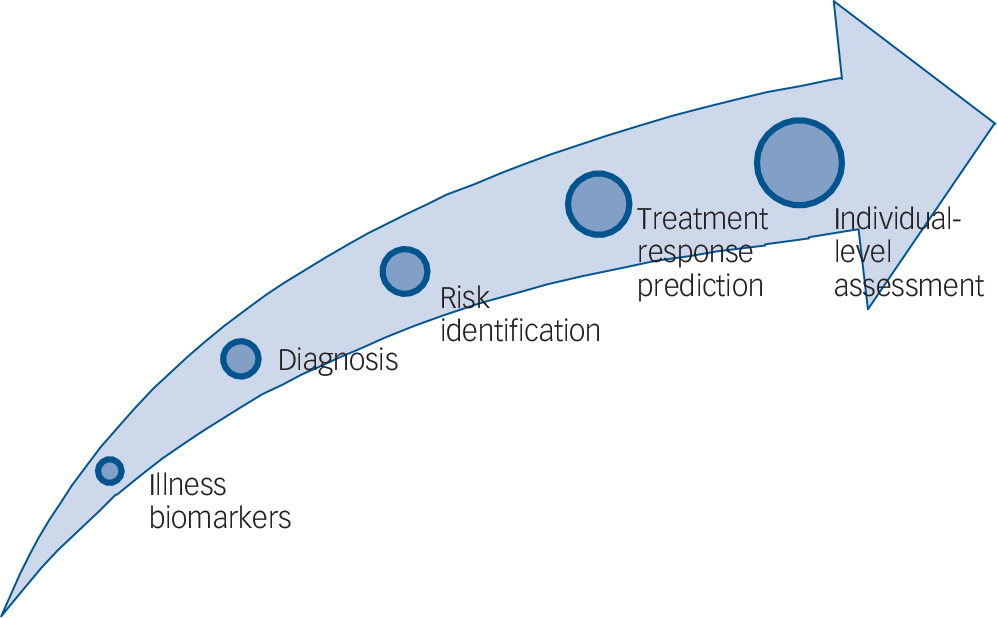
FIG. 1 Emerging clinical applications of neuroimaging methodologies in psychiatry.
Promising new findings highlight the potential of neuroimaging methodologies to be employed not only to identify biomarkers reflecting underlying illness mechanisms, but also to help identify neuroimaging measures that can help in the future with diagnosis, prediction of future risk for development of psychiatric disorders, and prediction of treatment response.
Conclusions
The absence of established biological measures to guide diagnosis, at-risk assessment and treatment choice leads to many challenges in psychiatric practice. Although maintaining high levels of training in psychiatric clinical skills remains crucial to clinical excellence, neuroimaging methodologies should be considered as useful tools to identify biological measures reflecting underlying illness mechanisms that in turn can help address major clinical challenges in psychiatry.




eLetters
No eLetters have been published for this article.