Introduction
Stroke is associated with significant morbidity and mortality. In Canada, approximately 46,500 people are hospitalized for stroke each year. It is the third leading cause of death, a significant cause of long-term disability, and exacts a significant cost to the economy. In 2012, the estimated cost of stroke in Canada was $3.6 billion. 1 Interventions that reduce the risk of stroke and improve outcomes in stroke patients are certainly of great importance.
The pharmacist has become an integral member of the multidisciplinary team providing clinical patient care in various healthcare settings. A meta-analysis evaluated the effects of pharmacist interventions in outpatient, inpatient, and emergency department settings. There was improvement in control of modifiable risk factors (blood pressure, cholesterol, hemoglobin A1C [HbA1C], and blood glucose) and reduced hospitalizations and mortality. Safety outcomes included a reduction in adverse drug events and medication errors.Reference Chisholm-Burns, Kim Lee and Spivey 2 It is reasonable to infer that pharmacist interventions may benefit patients with cerebrovascular disease. However, minimal literature has been published evaluating the role of the pharmacist in caring for this population. The objective of the present systematic review was to summarize the available evidence evaluating the impact of pharmacist interventions on outcomes in stroke patients.
Methods
Literature Search
A systematic search was performed using the following databases: Embase (1974 to March of 2015), International Pharmaceutical Abstracts (1970 to January of 2014), Medline (1948 to March of 2015), and Medline In-Process & Other Non-Indexed Citations (1948 to March of 2015). Disease-related search and MeSH terms included: transient ischemic attack, stroke, cerebral infarction, cerebrovascular accident, brain ischemia, ischemic stroke, cerebral hemorrhage, hemorrhagic stroke, and intracranial hemorrhage. Provider-related terms included: pharmacist, pharmacy student, and pharmacy resident. No limits were applied.
Study Selection
Studies were identified and duplicates removed. One author (JB) independently screened all of the titles and abstracts, identifying relevant articles for potential inclusion. Two authors (JB and MP) independently reviewed all the remaining abstracts and full-text articles (if available) for eligibility. Discrepancies were resolved by reviewer discussion. If consensus could not be reached, two of the authors (TM and KGP) were consulted. To be eligible, the abstracts/articles had to contain an intervention by a pharmacist, pharmacy resident, or pharmacy student, and the study population had to comprise patients with an acute stroke or TIA or a history of stroke or TIA. Studies where a portion of the population had an acute stroke or TIA or a history of a stroke or TIA were included if the results pertaining to that population were reported separately. Studies were excluded if: they were not written in English; when the pharmacist intervention was inconsistent, not clearly defined, or limited to drug distribution; if the article was a review, case report, or descriptive study; or where no objective outcomes were reported. Studies in which the main intervention was anticoagulation management were also excluded, as this area of pharmacy practice is well-established in previous literature.
Data Extraction
Two authors (JB and MP) independently performed data extraction using a standardized data collection form. The following data were collected from each abstract or full-text article: (1) study characteristics (including study design, sample size, duration of follow-up); (2) patient care setting (including location and patient population); and (3) characteristics of provided care (including collaboration, degree of patient interaction, mode of patient interaction, hours of service, type of intervention, and provision of follow-up). All study outcomes were recorded.
Data Analysis
A qualitative analysis was performed. The results are presented in a descriptive manner. A risk-of-bias assessment was not completed because of a lack of randomized trials and the limited number of full-text articles.
Results
A total of 894 articles were identified from the literature search, 20 of which were included in this systematic review (Figure 1). A total of 10 were published as full text and the remainder only as abstracts. The included studies consisted of four randomized controlled trials, one nonrandomized controlled trial, nine prospective observational studies, and six retrospective observational studies. Seven of the studies included patient-important outcomes such as patient satisfaction, adherence to or independence with medication, health-related quality of life (HRQoL), and readmission rates. The remainder (13) looked at such surrogate outcomes as number of drug therapy problems, changes in blood pressure or lipid panels, or medication prescription rates. The most common direct patient care activity implemented was medication counseling. While nine additional studies were included initially, they were removed after further discussion, as the intervention provided by the pharmacist within the team was unclear.Reference Bellolio, Finley and Flemming 3 - Reference McAlister, Grover and Padwal 11 The characteristics of the included studies are outlined in Table 1.
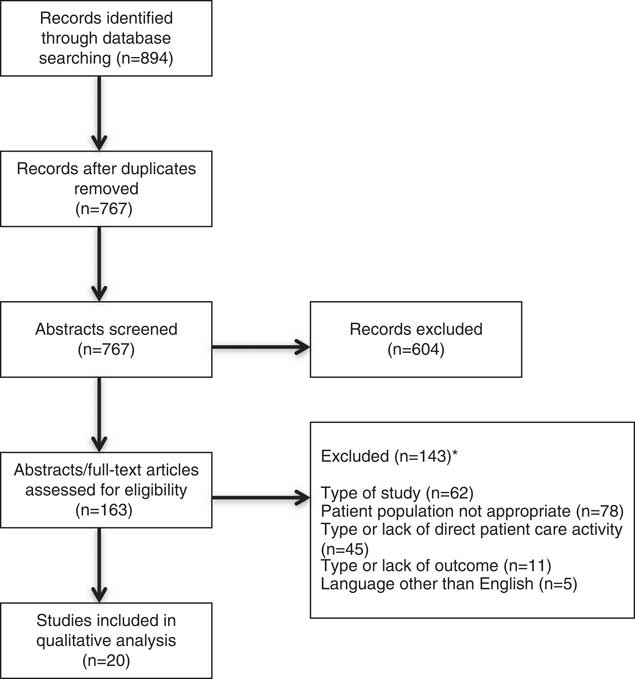
Figure 1 Study flow diagram. *More than one reason of exclusion could be selected for each study.
Table 1 Characteristics of included studies
DRP=drug-related problem; HCP=healthcare provider; LDL=low-density lipoprotein; LTC=long-term care, TIA=transient ischemic attack.
*Full-text article. † Number of evaluations. ‡ Number of patient encounters. § Number of stroke patients.
Emergency Department
One abstract (Brandon et al.Reference Brandon, Kramer and Mulawka 12 ) described pharmacist participation with stroke patients in the emergency department (ED). It demonstrated that addition of a pharmacist to the stroke pager team, as well as participation in assessment, dose verification, and patient education, resulted in a reduction of decision-to-needle thrombolytic administration times.
Inpatient Setting
Nine studies involved a pharmacist practicing in an inpatient setting.Reference Hohmann, Neumann-Haefelin, Klotz, Freidank and Radziwill 13 - Reference Scott, Sampson and D’Amato 21 Hohmann et al.Reference Hohmann, Neumann-Haefelin, Klotz, Freidank and Radziwill 13 demonstrated that a pharmacist completing medication reconciliation and participating in stroke team rounds resulted in identification of drug therapy problems in 68% of the patients, with an average of 1.8 problems per patient. In an another abstract by Hohmann et al.,Reference Hohmann, Klotz and Radziwill 14 the stroke unit pharmacist identified an average of 1.9 drug therapy problems per patient and resolved over 95% of the problems identified. Khalil et al.Reference Khalil, Li and Hua 15 found that 83% of stroke inpatients who received a medication management review by a pharmacist were on antihypertensive agents, compared to 59% of patients not reviewed by a pharmacist (p=0.005); 92% were on antithrombotic agents, in contrast to 77% of patients not reviewed by a pharmacist (p=0.025); while the difference in percentage of patients who were on lipid-lowering agents between the two groups was not significant. Barnett et al.Reference Barnett and Parmar 16 found that telephone referral from the hospital to a community pharmacist increased the proportion of patients receiving follow-up within 4 weeks of discharge from 1.5 to 32%. Two studies evaluated the impact of pharmacist intervention on medication adherence postdischarge. Hedegaard et al.Reference Hedegaard, Kjeldsen, Pottegard, Bak and Hallas 17 randomized TIA and stroke patients to a multifaceted intervention by a pharmacist compared to usual care (no pharmacist) and demonstrated no significant difference in adherence to or persistence with secondary stroke prevention medications. Conversely, Hohmann et al.Reference Hohmann, Neumann-Haefelin, Klotz, Freidank and Radziwill 18 found that a letter communicating medication changes sent from an inpatient pharmacist to a patient’s primary care provider at hospital discharge after a stroke or TIA increased medication adherence from 83 to 91% at 3 months postdischarge (p=0.01) when compared to the control group, who had medication lists included in the discharge letter by the neurologist, as before. Tsai et al.Reference Tsai, Leu, Lin and Lu 19 suggested that recommendations by clinical pharmacists improved stroke guideline performance indicators. SreenivasanReference Sreenivasan 20 found that patient satisfaction with stroke educational sessions improved when an interdisciplinary team including pharmacists presented the program. Scott et al.Reference Scott, Sampson and D’Amato 21 reported that a self-medication program that included pharmacist medication teaching resulted in 78.1% of stroke patients achieving independence with their medications.
Outpatient Setting
Seven studies reported outcomes associated with pharmacist interventions in outpatient settings.Reference Lindblad and Howorko 22 - Reference Lee, Graham, Silliman and Merino-Juarez 28 Lindblad et al.Reference Lindblad and Howorko 22 found that a pharmacist in a stroke prevention clinic was able to make an average of 2.8 interventions per patient encounter. McAlister et al.Reference McAlister, Majumdar and Padwal 23 compared pharmacist-led and nurse-led case management of stroke patients in a randomized controlled trial. The control group received monthly follow-up from a nurse, who provided lifestyle advice, measured blood pressure and lipid levels, and faxed the results to their primary care physician. Patients in the intervention group were managed by a pharmacist with prescribing authority, and they received the same follow-up as the control group, as well as initiation/titration of antihypertensives and/or lipid-lowering therapy. After 6 months, 43% of patients managed by a pharmacist met both systolic blood pressure and low-density lipoprotein (LDL) goals, and 31% of patients managed by a nurse met both goals (number needed to treat=8, p=0.03). In another randomized controlled trial, Chiu et al.Reference Chiu, Wu, Lee, Huang, Tan and Chang 24 evaluated the effect of monthly pharmacist education compared with usual care on modifiable risk factors. In the pharmacist intervention group, there was no significant difference in blood glucose control at the end of the study, but 83% of patients had adequately controlled blood pressure (compared to 40% at baseline, p≤0.001) and 40% of patients had adequately controlled lipids (compared to 13% at baseline, p=0.01). In contrast, the control group had nonsignificant differences in all three endpoints. Similarly, Nguyen et al.Reference Nguyen, Poon, Tokuda, Sayers, Wallis and Dergalust 25 recruited patients from a stroke prevention clinic and randomized them to pharmacist intervention or usual care. The pharmacist intervention group received telephone follow-up at 3 and 6 months to evaluate medication adherence, provide education, and reassess stroke prevention goals. Patients in the pharmacist intervention group were more likely to achieve blood pressure, cholesterol, and blood glucose goals at 6 months than those in the control group, and these improvements were maintained at 1 year. Hooker et al.Reference Hooker and Evans 26 evaluated the impact of a stroke bridge clinic involving a pharmacist, nurse practitioner, and nurse navigator on hospital readmission rates. Patients visited the clinic a week after discharge for education on risk factors and stroke prevention, medication reconciliation, and individualized treatment plans. Hospital readmission rates decreased from 14.5 to 2.2%. Similarly, Bruner et al.Reference Bruner 27 reviewed pharmacist participation in stroke clinics, addressing drug therapy problems and providing medication education, noting that the clinics had a positive effect on 30-day hospital readmission rates. Lee et al.Reference Lee, Graham, Silliman and Merino-Juarez 28 found a non-statistically-significant improvement in patients’ knowledge of their current drug therapy after pharmacist medication counseling.
Community Pharmacy
There were two studiesReference Hohmann, Klotz, Radziwill, Jacobs and Kissel 29 , Reference Fincham, Wallace and Ivory 30 conducted in a community pharmacy setting. Hohmann et al.Reference Hohmann, Klotz, Radziwill, Jacobs and Kissel 29 evaluated the impact of pharmaceutical care on the HRQoL of patients with a TIA or stroke who were discharged home. The pharmacist provided medication reviews and education, and resolved drug therapy problems. HRQoL was assessed using a scale validated in stroke patients. In the pharmacist intervention group, HRQoL remained stable, with only one of the HRQoL scales significantly decreased from baseline; in contrast, the control group had decreases in seven of eight scales. Fincham et al.Reference Fincham, Wallace and Ivory 30 found that community pharmacist intervention reduced the average number of days patients were late for ticlopidine prescription pickup from 11 to 2.
Long-Term Care
Only one study was performed in a long-term care setting. Horning et al.Reference Horning, Hoehns and Doucette 31 found that the difference in stroke guideline adherence between patients receiving active pharmacist disease state management consultation services compared to traditional pharmacist drug review was not statistically significant (p=0.096).
Discussion
Stroke patients interact with healthcare providers at many points throughout the course of their disease management. Diagnosis is often made in the ED, patients are admitted to acute-care hospitals, and, following discharge, stroke outpatient clinics assist patients with transition to the community and with chronic disease management. In the community, stroke patients seek medication and health-related advice from their primary care providers and may also require care in a long-term care facility. Our systematic review provides evidence that stroke patients benefit from pharmacist interventions in multiple care settings.
The available full-text studies suggest that pharmacists can positively impact stroke patient care in inpatient and outpatient settings with increased use of evidence-based therapies, medication adherence, risk-factor target achievement, and maintenance of HRQoL. The best available evidence demonstrates improvement in surrogate endpoints, and the cumulative evidence is positive for both surrogate and patient important outcomes. While providing fewer details, the reviewed abstracts largely support these studies and previously published literature supporting the value of pharmacists in several of these settings.
The acute treatment of stroke involves emergent administration of thrombolytic agents to reduce the risk of disability and death.Reference Wardlaw, Murray, Berge and del Zoppo 32 Current guidelines recommend thrombolytic therapy within 4.5 hours of symptom onset, with a door-to-needle goal time of 60 minutes.Reference Jauch, Saver and Adams 33 , Reference Lindsay, Gubitz and Bayley 34 In the ED, a pharmacist’s assessment of patient eligibility and appropriateness of thrombolytic orders decreases time to administration, increases thrombolytic administration within the goal time, and improves order accuracy. Previous studies have shown that pharmacists in the ED add value through identification of medication errors, optimization of drug therapy, improvement of medication utilization, and increasing adherence to evidence-based practices.Reference Marconi and Claudius 35 - Reference Cesarz, Steffenhagen, Svenson and Hamedani 38 Our systematic review provides further evidence in support of pharmacists working within the ED, with an emphasis on the subset of patients with suspected or confirmed stroke.
Organized inpatient (stroke unit) care is described as “focusing of care for stroke patients in hospital under a multidisciplinary team who specialize in stroke management.” 39 When compared to care provided on a general ward, stroke unit care is associated with reductions in mortality, requirement for institutionalized care, and dependency. Pharmacists use their drug-focused therapeutic knowledge and medication management expertise to make valuable contributions to inpatient stroke care teams. A systematic review by Kaboli et al.Reference Kaboli, Hoth, McClimon and Schnipper 40 discussed the benefits provided by clinical inpatient pharmacists, including less adverse drug events, increased accuracy of medication and allergy information, shorter lengths of stay, and reductions in hospital costs. Our systematic review further suggests that stroke patients may also benefit from having pharmacists integrated into inpatient stroke care in order to perform these evidence-based activities.
The period of time following hospital discharge can be difficult for the patients and their family members. Previous studiesReference Stading, Herrmann, Walters, Destache and Chock 41 - Reference Cording, Engelbrecht-Zadvomy, Pettit, Eastham and Sandoval 43 have demonstrated that pharmacist interventions in the outpatient setting are associated with significant improvements in management of modifiable risk factors, including reductions in HbA1C, blood pressure, and lipid levels. Our review found that outpatient pharmacists provide patient education and risk-factor modification, which results in reduced readmission and stroke recurrence rates. In conjunction with previous literature, the results from this systematic review provide support for pharmacists in the care of stroke patients in the outpatient setting.
Despite the available evidence, there remains a significant gap between research and practice in the care of stroke patients. Until recently, national stroke guidelines in North AmericaReference Casaubon and Suddes 44 did not include pharmacists on the list of recommended members of a stroke team. Interventions should be made in an effort to close this gap and ensure that pharmacists are active members of stroke teams in all settings.
Limitations of the Study
This review has limitations that warrant discussion. The quality and consistency of the research literature supporting integration of pharmacists into the stroke setting are limited. A search for unpublished literature was not performed. Studies with negative results may not be published, and this could lead to publication bias and an overestimation of the benefit of pharmacists in stroke care. Another limitation is that 50% of the studies included have not been published in full-text version, and abstracts provide limited information.
Conclusions
Pharmacists provide care to stroke patients in multiple settings. Supporting existing literature in other patient types, our review suggests that pharmacists improve the use of evidence-based therapies, reduce stroke risk through control of modifiable risk factors, and improve patient adherence in stroke-specific populations as well. Pharmacists should be considered an integral provider in the care of stroke patients.
Acknowledgments
We are grateful to Drs. Brian Buck and Mark Makowsky for their thoughtful reviews of this manuscript.
Statement of Authorship
All four authors meet the criteria set out by the International Committee of Medical Journal Editors—namely, having had substantial contributions to the conception, design, analysis, and interpretation of the work; drafting and revising the paper; final approval of the attached version; and agreement to be accountable for all aspects of the work.
Disclosures
Jade E. Basaraba, Michelle Picard, Kirsten George-Phillips, and Tania Mysak hereby declare that they have no conflicts of interest to disclose.



