173 results
A causal roadmap for generating high-quality real-world evidence
-
- Journal:
- Journal of Clinical and Translational Science / Volume 7 / Issue 1 / 2023
- Published online by Cambridge University Press:
- 22 September 2023, e212
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
A new era for the negative symptoms of schizophrenia
-
- Journal:
- The British Journal of Psychiatry / Volume 223 / Issue 1 / July 2023
- Published online by Cambridge University Press:
- 10 July 2023, pp. 269-270
- Print publication:
- July 2023
-
- Article
-
- You have access
- HTML
- Export citation
Socioeconomic differences in antibiotic use for common infections in pediatric urgent-care centers—A quasi-experimental study
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 44 / Issue 12 / December 2023
- Published online by Cambridge University Press:
- 29 June 2023, pp. 2009-2016
- Print publication:
- December 2023
-
- Article
-
- You have access
- HTML
- Export citation
Appropriateness of antibiotic prescribing varies by clinical services at United States children’s hospitals
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 44 / Issue 11 / November 2023
- Published online by Cambridge University Press:
- 12 April 2023, pp. 1711-1717
- Print publication:
- November 2023
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
In defense of the personal/impersonal distinction in moral psychology research: Cross-cultural validation of the dual process model of moral judgment
-
- Journal:
- Judgment and Decision Making / Volume 6 / Issue 3 / April 2011
- Published online by Cambridge University Press:
- 01 January 2023, pp. 186-195
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Tricuspid atresia and common arterial trunk: a rare form of CHD
-
- Journal:
- Cardiology in the Young / Volume 33 / Issue 7 / July 2023
- Published online by Cambridge University Press:
- 06 December 2022, pp. 1192-1195
-
- Article
- Export citation
Characteristics of antifungal utilization for hospitalized children in the United States
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 2 / Issue 1 / 2022
- Published online by Cambridge University Press:
- 02 December 2022, e190
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
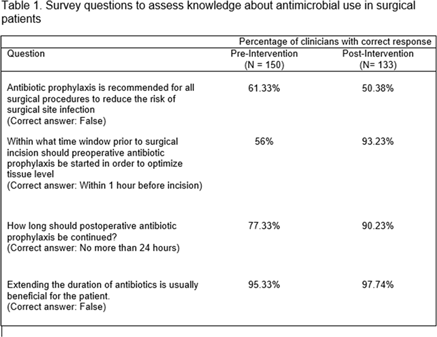
Novel expansion of a well-established antimicrobial stewardship program: Enhancing program efficiency and reach
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 44 / Issue 6 / June 2023
- Published online by Cambridge University Press:
- 30 August 2022, pp. 869-874
- Print publication:
- June 2023
-
- Article
- Export citation
Large-Format Direct Detection Camera for Cryo-EM at 100 keV
-
- Journal:
- Microscopy and Microanalysis / Volume 28 / Issue S1 / August 2022
- Published online by Cambridge University Press:
- 22 July 2022, pp. 1172-1173
- Print publication:
- August 2022
-
- Article
-
- You have access
- Export citation
Variation in ampicillin dosing for lower respiratory tract infections and neonatal bacterial infections in US children’s hospitals
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 2 / Issue 1 / 2022
- Published online by Cambridge University Press:
- 23 May 2022, e85
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
The utility of a structured, interactive cardiac anatomy teaching session for resident education
-
- Journal:
- Cardiology in the Young / Volume 33 / Issue 2 / February 2023
- Published online by Cambridge University Press:
- 22 April 2022, pp. 208-212
-
- Article
- Export citation
Reptamsassia n. gen. (Amsassiaceae n. fam.; calcareous algae) from the Lower Ordovician (Floian) of western Newfoundland, and the earliest symbiotic intergrowth of modular species
-
- Journal:
- Journal of Paleontology / Volume 96 / Issue 3 / May 2022
- Published online by Cambridge University Press:
- 28 January 2022, pp. 715-728
-
- Article
- Export citation
Hippocampal volume and volume asymmetry prospectively predict PTSD symptom emergence among Iraq-deployed soldiers
-
- Journal:
- Psychological Medicine / Volume 53 / Issue 5 / April 2023
- Published online by Cambridge University Press:
- 22 November 2021, pp. 1906-1913
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Outpatient antimicrobial stewardship programs in pediatric institutions in 2020: Status, needs, barriers
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 43 / Issue 10 / October 2022
- Published online by Cambridge University Press:
- 22 October 2021, pp. 1396-1402
- Print publication:
- October 2022
-
- Article
- Export citation
Amsassia (calcareous alga) from the Lower Ordovician (Tremadocian) of western Newfoundland, and the biologic affinity and geologic history of the genus
-
- Journal:
- Journal of Paleontology / Volume 96 / Issue 1 / January 2022
- Published online by Cambridge University Press:
- 21 September 2021, pp. 1-18
-
- Article
- Export citation
Alpha-blockade during congenital heart surgery admissions: analysis from national database
- Part of
-
- Journal:
- Cardiology in the Young / Volume 32 / Issue 7 / July 2022
- Published online by Cambridge University Press:
- 17 September 2021, pp. 1136-1142
-
- Article
- Export citation
Revealing the Relation between Star Formation Activity of Jellyfish Galaxies and Ram Pressure Stripping
-
- Journal:
- Proceedings of the International Astronomical Union / Volume 17 / Issue S373 / August 2021
- Published online by Cambridge University Press:
- 09 June 2023, pp. 132-135
- Print publication:
- August 2021
-
- Article
- Export citation
Promoting Antimicrobial Stewardship Education Among Pediatricians Through a Maintenance of Certification Part 4 Quality Impro
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 1 / Issue S1 / July 2021
- Published online by Cambridge University Press:
- 29 July 2021, p. s29
-
- Article
-
- You have access
- Open access
- Export citation
Quality Indicators for Older Persons’ Transitions in Care: A Systematic Review and Delphi Process
-
- Journal:
- Canadian Journal on Aging / La Revue canadienne du vieillissement / Volume 41 / Issue 1 / March 2022
- Published online by Cambridge University Press:
- 03 June 2021, pp. 40-54
-
- Article
-
- You have access
- HTML
- Export citation
39901 Breaking down silos to synergize clinical trial development and initiation: The Clinical Research Support Center, University of Minnesota
-
- Journal:
- Journal of Clinical and Translational Science / Volume 5 / Issue s1 / March 2021
- Published online by Cambridge University Press:
- 30 March 2021, pp. 108-109
-
- Article
-
- You have access
- Open access
- Export citation