136 results
Importance, motivation and confidence of eating healthily whilst at university and barriers UK students face to eating well at university
-
- Journal:
- Proceedings of the Nutrition Society / Volume 82 / Issue OCE5 / 2023
- Published online by Cambridge University Press:
- 08 January 2024, E347
-
- Article
-
- You have access
- HTML
- Export citation
Extensive dickitization of the permo-triassic fluvial sandstones from the eastern Iberian Range, Spain
-
- Journal:
- Clays and Clay Minerals / Volume 55 / Issue 5 / October 2007
- Published online by Cambridge University Press:
- 01 January 2024, pp. 481-490
-
- Article
- Export citation
Guide to assembling a successful K99/R00 application
-
- Journal:
- Journal of Clinical and Translational Science / Volume 7 / Issue 1 / 2023
- Published online by Cambridge University Press:
- 29 September 2023, e215
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Dementia as a presentation of motor neurone disease: a case report
-
- Journal:
- European Psychiatry / Volume 66 / Issue S1 / March 2023
- Published online by Cambridge University Press:
- 19 July 2023, p. S753
-
- Article
-
- You have access
- Open access
- Export citation
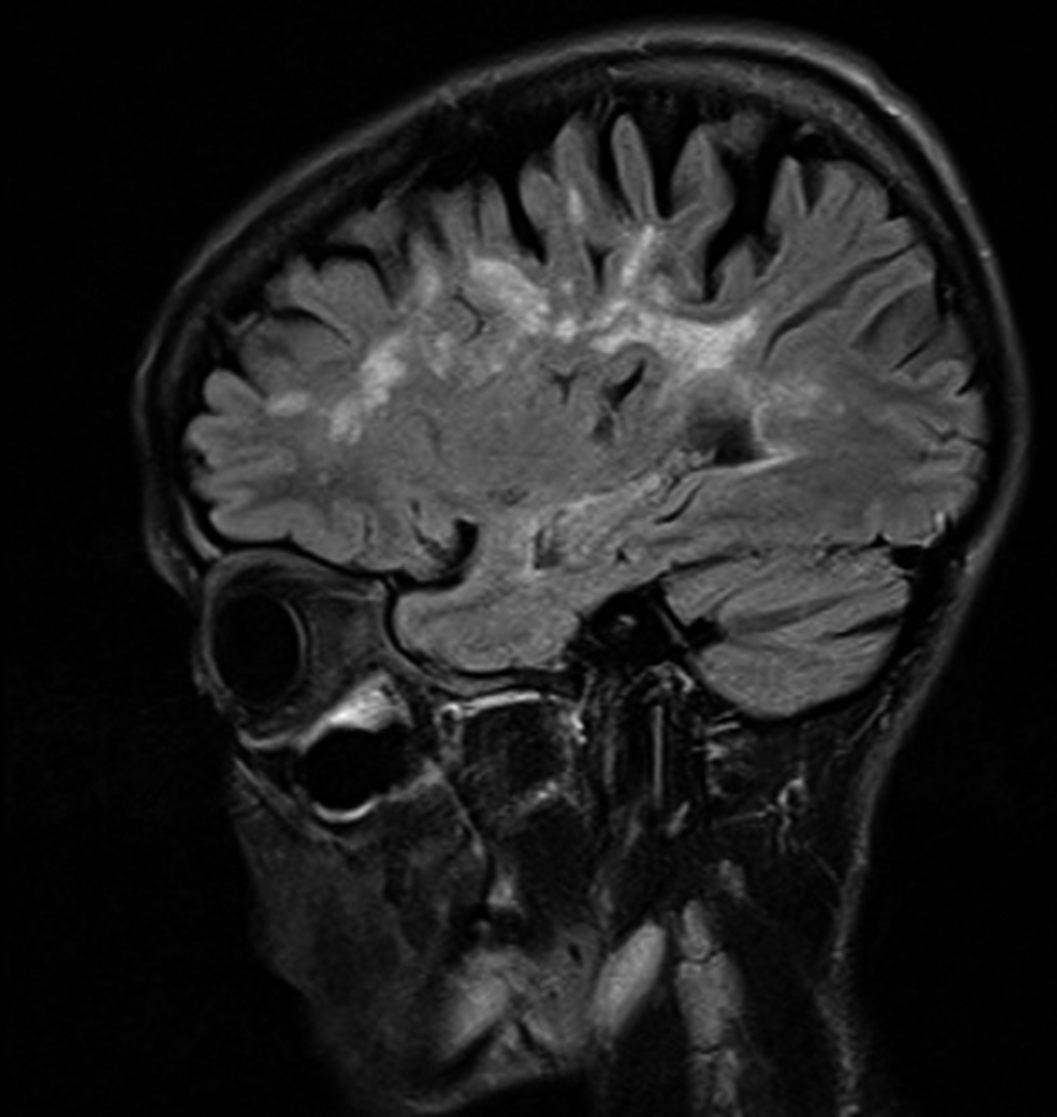
Cyclothymia, bipolar disorder and multiple sclerosis: A case report
-
- Journal:
- European Psychiatry / Volume 66 / Issue S1 / March 2023
- Published online by Cambridge University Press:
- 19 July 2023, pp. S703-S704
-
- Article
-
- You have access
- Open access
- Export citation
Blue justice: A review of emerging scholarship and resistance movements
-
- Journal:
- Cambridge Prisms: Coastal Futures / Volume 1 / 2023
- Published online by Cambridge University Press:
- 26 January 2023, e15
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Biomarkers of sepsis in pigs, horses and cattle: from acute phase proteins to procalcitonin
-
- Journal:
- Animal Health Research Reviews / Volume 23 / Issue 1 / June 2022
- Published online by Cambridge University Press:
- 07 July 2022, pp. 82-99
-
- Article
- Export citation
Validating a risk assessment tool in United Kingdom and Irish paediatric cardiac catheterisation practice
- Part of
-
- Journal:
- Cardiology in the Young / Volume 32 / Issue 9 / September 2022
- Published online by Cambridge University Press:
- 14 October 2021, pp. 1407-1414
-
- Article
- Export citation
Impacts of social distancing during the covid19 pandemic on the development of children with autism in Brazil
-
- Journal:
- European Psychiatry / Volume 64 / Issue S1 / April 2021
- Published online by Cambridge University Press:
- 13 August 2021, pp. S262-S263
-
- Article
-
- You have access
- Open access
- Export citation
Glucagon-like peptide-1 receptor agonists in patients treated with antipsychotics
-
- Journal:
- European Psychiatry / Volume 64 / Issue S1 / April 2021
- Published online by Cambridge University Press:
- 13 August 2021, p. S775
-
- Article
-
- You have access
- Open access
- Export citation
Creating enriched training sets of eligible studies for large systematic reviews: the utility of PubMed's Best Match algorithm
- Part of
-
- Journal:
- International Journal of Technology Assessment in Health Care / Volume 37 / Issue 1 / 2021
- Published online by Cambridge University Press:
- 18 December 2020, e7
-
- Article
- Export citation
Clinical Factors as Predictors on Functional Impairment in Bipolar Disorder
-
- Journal:
- European Psychiatry / Volume 24 / Issue S1 / January 2009
- Published online by Cambridge University Press:
- 16 April 2020, 24-E603
-
- Article
-
- You have access
- Export citation
P0157 - Why clinicians maintain antidepressants in some patients with acute mania? Hints from a large, observational study (EMBLEM)
-
- Journal:
- European Psychiatry / Volume 23 / Issue S2 / April 2008
- Published online by Cambridge University Press:
- 16 April 2020, p. S238
-
- Article
-
- You have access
- Export citation
Functioning in patients with recently diagnosed vs. chronic schizophrenia treated with paliperidone ER
-
- Journal:
- European Psychiatry / Volume 26 / Issue S2 / March 2011
- Published online by Cambridge University Press:
- 16 April 2020, p. 1285
-
- Article
-
- You have access
- Export citation
Tolerability and treatment response in patients with recently diagnosed vs. chronic schizophrenia treated with paliperidone ER
-
- Journal:
- European Psychiatry / Volume 26 / Issue S2 / March 2011
- Published online by Cambridge University Press:
- 16 April 2020, p. 1503
-
- Article
-
- You have access
- Export citation
P0179 - Prospective, multicenter, open-label, observational study of sexual function in patients beginning aripiprazole treatment
-
- Journal:
- European Psychiatry / Volume 23 / Issue S2 / April 2008
- Published online by Cambridge University Press:
- 16 April 2020, pp. S133-S134
-
- Article
-
- You have access
- Export citation
Tolerability and treatment response in patients with recently diagnosed vs. chronic schizophrenia treated with paliperidone ER
-
- Journal:
- European Psychiatry / Volume 26 / Issue S2 / March 2011
- Published online by Cambridge University Press:
- 16 April 2020, p. 1502
-
- Article
-
- You have access
- Export citation
EPA-1549 - A Randomized, Active-controlled Rater-blinded 2-year Study of Paliperidone Palmitate Versus Investigators’ Choice of Oral Antipsychotic Monotherapy in Patients with Schizophrenia (prosipal)
-
- Journal:
- European Psychiatry / Volume 29 / Issue S1 / 2014
- Published online by Cambridge University Press:
- 15 April 2020, p. 1
-
- Article
-
- You have access
- Export citation
EPA-0330 – Ilex Paraguariensis use and Affective Symptoms: ¿is There an Association?
-
- Journal:
- European Psychiatry / Volume 29 / Issue S1 / 2014
- Published online by Cambridge University Press:
- 15 April 2020, p. 1
-
- Article
-
- You have access
- Export citation
P-201 - Effectiveness of Quetiapine xr Vs. Sertraline in Acute Bipolar Depression as Add-on Therapy to Previous Mood Stabilizer Treatment: a Pilot Study
-
- Journal:
- European Psychiatry / Volume 27 / Issue S1 / 2012
- Published online by Cambridge University Press:
- 15 April 2020, p. 1
-
- Article
-
- You have access
- Export citation