196 results
Advancing health equity through action in antimicrobial stewardship and healthcare epidemiology
- Part of
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 45 / Issue 4 / April 2024
- Published online by Cambridge University Press:
- 14 February 2024, pp. 412-419
- Print publication:
- April 2024
-
- Article
-
- You have access
- HTML
- Export citation
Impact of primary care triage using the Head and Neck Cancer Risk Calculator version 2 on tertiary head and neck services in the post-coronavirus disease 2019 period
-
- Journal:
- The Journal of Laryngology & Otology , First View
- Published online by Cambridge University Press:
- 22 January 2024, pp. 1-6
-
- Article
- Export citation
Variations in implementation of antimicrobial stewardship via telehealth at select Veterans Affairs medical centers
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 3 / Issue S2 / June 2023
- Published online by Cambridge University Press:
- 29 September 2023, p. s38
-
- Article
-
- You have access
- Open access
- Export citation
Susceptibility results discrepancy analysis between NHSN antimicrobial resistance (AR) Option and NEDSS Base System in Tennessee, July 2020–December 2021
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 3 / Issue S2 / June 2023
- Published online by Cambridge University Press:
- 29 September 2023, p. s104
-
- Article
-
- You have access
- Open access
- Export citation
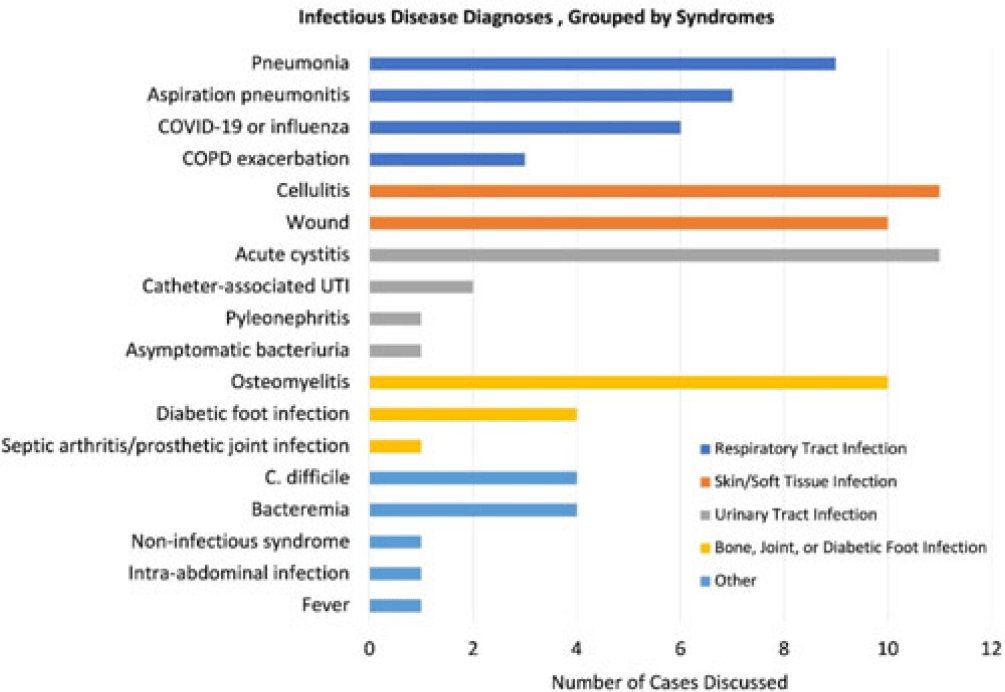
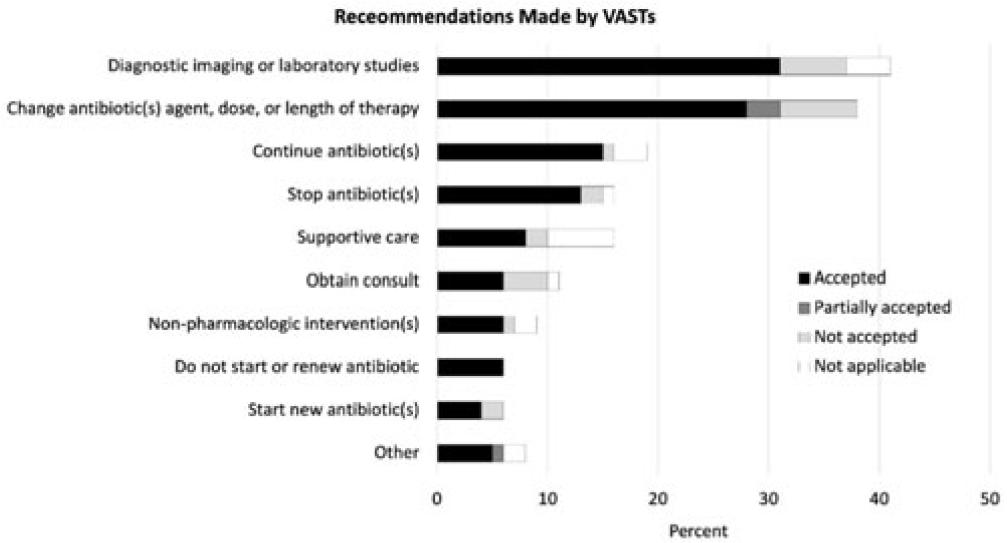
Using telehealth to support antimicrobial stewardship at four rural VA medical centers: Interim analysis
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 3 / Issue S2 / June 2023
- Published online by Cambridge University Press:
- 29 September 2023, p. s110
-
- Article
-
- You have access
- Open access
- Export citation
Determining trends of respiratory tract infections in a long-term care facility pilot surveillance project
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 3 / Issue S2 / June 2023
- Published online by Cambridge University Press:
- 29 September 2023, p. s24
-
- Article
-
- You have access
- Open access
- Export citation
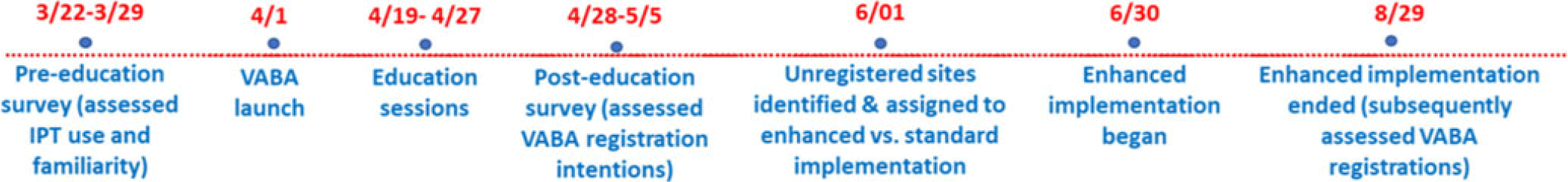
Increasing Registration for a VA Multidrug-Resistant Organism Alert Tool
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 3 / Issue S2 / June 2023
- Published online by Cambridge University Press:
- 29 September 2023, pp. s124-s125
-
- Article
-
- You have access
- Open access
- Export citation
Dense pasts: settlement archaeology after Fox's The archaeology of the Cambridge region (1923)
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Volatility, Realignment, and Electoral Shocks: Brexit and the UK General Election of 2019
-
- Journal:
- PS: Political Science & Politics / Volume 56 / Issue 4 / October 2023
- Published online by Cambridge University Press:
- 10 August 2023, pp. 537-545
- Print publication:
- October 2023
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Incidence and risk factors for clinically confirmed secondary bacterial infections in patients hospitalized for coronavirus disease 2019 (COVID-19)
-
- Journal:
- Infection Control & Hospital Epidemiology / Volume 44 / Issue 10 / October 2023
- Published online by Cambridge University Press:
- 15 May 2023, pp. 1650-1656
- Print publication:
- October 2023
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
No effects of synchronicity in online social dilemma experiments: A registered report
-
- Journal:
- Judgment and Decision Making / Volume 16 / Issue 4 / July 2021
- Published online by Cambridge University Press:
- 01 January 2023, pp. 823-843
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Chapter 5 - Financing Health Care
- from Section 1 - Analyzing Health Systems: Concepts, Components, Performance
-
-
- Book:
- Making Health Systems Work in Low and Middle Income Countries
- Published online:
- 08 December 2022
- Print publication:
- 29 December 2022, pp 67-82
-
- Chapter
- Export citation
The Evolutionary Map of the Universe Pilot Survey – ADDENDUM
-
- Journal:
- Publications of the Astronomical Society of Australia / Volume 39 / 2022
- Published online by Cambridge University Press:
- 02 November 2022, e055
-
- Article
- Export citation
Examining the Scope of Nuclear Weapons-Related Activities Covered under the Environmental Remediation Obligation of the Treaty on the Prohibition of Nuclear Weapons
-
- Journal:
- Asian Journal of International Law / Volume 13 / Issue 2 / July 2023
- Published online by Cambridge University Press:
- 22 September 2022, pp. 365-390
- Print publication:
- July 2023
-
- Article
- Export citation
A Three-Dimensional Reconstruction Algorithm for Scanning Transmission Electron Microscopy Data from a Single Sample Orientation
-
- Journal:
- Microscopy and Microanalysis / Volume 28 / Issue 5 / October 2022
- Published online by Cambridge University Press:
- 24 June 2022, pp. 1632-1640
- Print publication:
- October 2022
-
- Article
- Export citation
Increased carbapenemase testing following implementation of national VA guidelines for carbapenem-resistant Enterobacterales (CRE)
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 2 / Issue 1 / 2022
- Published online by Cambridge University Press:
- 02 June 2022, e88
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Susceptibility results discrepancy analysis between NHSN Antibiotic Resistance (AR) Option and laboratory instrument data
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 2 / Issue S1 / July 2022
- Published online by Cambridge University Press:
- 16 May 2022, p. s66
-
- Article
-
- You have access
- Open access
- Export citation
Effect of the COVID-19 pandemic on Tennessee hospital antibiotic use
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 2 / Issue S1 / July 2022
- Published online by Cambridge University Press:
- 16 May 2022, p. s20
-
- Article
-
- You have access
- Open access
- Export citation
Determining the effect of COVID-19 on antibiotic use in long-term care facilities across Tennessee
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 2 / Issue S1 / July 2022
- Published online by Cambridge University Press:
- 16 May 2022, pp. s21-s22
-
- Article
-
- You have access
- Open access
- Export citation
Effects of antibiotic suppression on three healthcare systems’ National Healthcare Safety Network Antibiotic Resistance Option data
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 1 / Issue 1 / 2021
- Published online by Cambridge University Press:
- 10 November 2021, e47
-
- Article
-
- You have access
- Open access
- HTML
- Export citation