2044 results
Moderate and Deep Sedation in Clinical Practice
- Coming soon
-
- Expected online publication date:
- December 2024
- Print publication:
- 30 November 2024
-
- Book
- Export citation
Reflecting on Armenians in Ottoman Historiography
-
- Journal:
- Review of Middle East Studies , First View
- Published online by Cambridge University Press:
- 24 September 2024, pp. 1-10
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Social security and retirement around the world: lessons from a long-term collaboration
-
- Journal:
- Journal of Pension Economics & Finance , First View
- Published online by Cambridge University Press:
- 19 September 2024, pp. 1-23
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
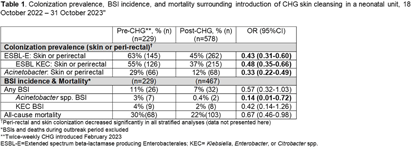
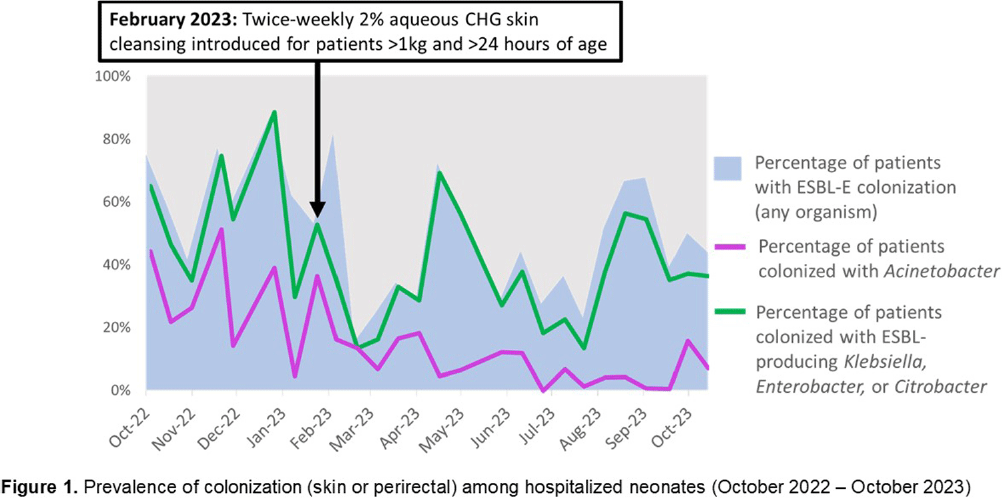
Temporal decreases in pathogen colonization and infection among hospitalized neonates following routine skin antisepsis with chlorhexidine gluconate: Botswana 2022 – 2023
-
- Journal:
- Antimicrobial Stewardship & Healthcare Epidemiology / Volume 4 / Issue S1 / July 2024
- Published online by Cambridge University Press:
- 16 September 2024, p. s12
-
- Article
-
- You have access
- Open access
- Export citation
Detecting suicide risk among U.S. servicemembers and veterans: a deep learning approach using social media data
-
- Journal:
- Psychological Medicine , First View
- Published online by Cambridge University Press:
- 09 September 2024, pp. 1-10
-
- Article
-
- You have access
- HTML
- Export citation
Development and initial evaluation of a clinical prediction model for risk of treatment resistance in first-episode psychosis: Schizophrenia Prediction of Resistance to Treatment (SPIRIT)
-
- Journal:
- The British Journal of Psychiatry , FirstView
- Published online by Cambridge University Press:
- 05 August 2024, pp. 1-10
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Ectoparasite and bacterial population genetics and community structure indicate extent of bat movement across an island chain
-
- Journal:
- Parasitology , First View
- Published online by Cambridge University Press:
- 24 May 2024, pp. 1-14
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Interactive visualization tool to understand and monitor health disparities in diabetes care and outcomes
-
- Journal:
- Journal of Clinical and Translational Science / Volume 8 / Issue 1 / 2024
- Published online by Cambridge University Press:
- 17 May 2024, e102
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Diagnostic criteria and core outcome set development for necrotising otitis externa: the COSNOE Delphi consensus study
-
- Journal:
- The Journal of Laryngology & Otology , First View
- Published online by Cambridge University Press:
- 22 April 2024, pp. 1-8
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Laxative use in adults with intellectual disabilities: development of prescribing guidelines
-
- Journal:
- BJPsych Open / Volume 10 / Issue 3 / May 2024
- Published online by Cambridge University Press:
- 18 April 2024, e84
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
VaTEST III: Validation of eight potential super-earths from TESS data
-
- Journal:
- Publications of the Astronomical Society of Australia / Volume 41 / 2024
- Published online by Cambridge University Press:
- 11 April 2024, e030
-
- Article
-
- You have access
- HTML
- Export citation
Querying ‘Global’ Music History: Significant Geographies between Goswami Pannalal and Queen Victoria
-
- Journal:
- Royal Musical Association Research Chronicle ,
- Published online by Cambridge University Press:
- 05 April 2024, pp. 1-12
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
569 Investigating the Role of FOXA2 During the Transition to Neuroendocrine Prostate Cancer
- Part of
-
- Journal:
- Journal of Clinical and Translational Science / Volume 8 / Issue s1 / April 2024
- Published online by Cambridge University Press:
- 03 April 2024, pp. 148-149
-
- Article
-
- You have access
- Open access
- Export citation
Head and Neck Cancer: United Kingdom National Multidisciplinary Guidelines, Sixth Edition
-
- Journal:
- The Journal of Laryngology & Otology / Volume 138 / Issue S1 / April 2024
- Published online by Cambridge University Press:
- 14 March 2024, pp. S1-S224
- Print publication:
- April 2024
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Astrobiological applications of μ-mapping X-ray fluorescence spectrometry
-
- Journal:
- International Journal of Astrobiology / Volume 23 / 2024
- Published online by Cambridge University Press:
- 04 March 2024, e8
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Trajectory of adjustment difficulties following disaster: 10-year longitudinal cohort study
-
- Journal:
- BJPsych Open / Volume 10 / Issue 2 / March 2024
- Published online by Cambridge University Press:
- 04 March 2024, e57
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
The Natural Occurrence of Eta-Alumina (η-Al2O3) in Bauxite
-
- Journal:
- Clays and Clay Minerals / Volume 44 / Issue 5 / October 1996
- Published online by Cambridge University Press:
- 28 February 2024, pp. 658-664
-
- Article
-
- You have access
- Export citation
Analytical Electron Microscopy in Clays and Other Phyllosilicates: Loss of Elements from a 90-nm Stationary Beam of 300-keV Electrons
-
- Journal:
- Clays and Clay Minerals / Volume 46 / Issue 3 / June 1998
- Published online by Cambridge University Press:
- 28 February 2024, pp. 301-316
-
- Article
-
- You have access
- Export citation
Hisingerite: A Ferric Kaolin Mineral with Curved Morphology
-
- Journal:
- Clays and Clay Minerals / Volume 46 / Issue 4 / August 1998
- Published online by Cambridge University Press:
- 28 February 2024, pp. 400-413
-
- Article
-
- You have access
- Export citation
Tohdite (5Al2O3 · H2O) in Bauxites from Northern Australia
-
- Journal:
- Clays and Clay Minerals / Volume 42 / Issue 4 / August 1994
- Published online by Cambridge University Press:
- 28 February 2024, pp. 485-488
-
- Article
-
- You have access
- Export citation