Machines may soon replace healthcare workers in some aspects of their traditional roles
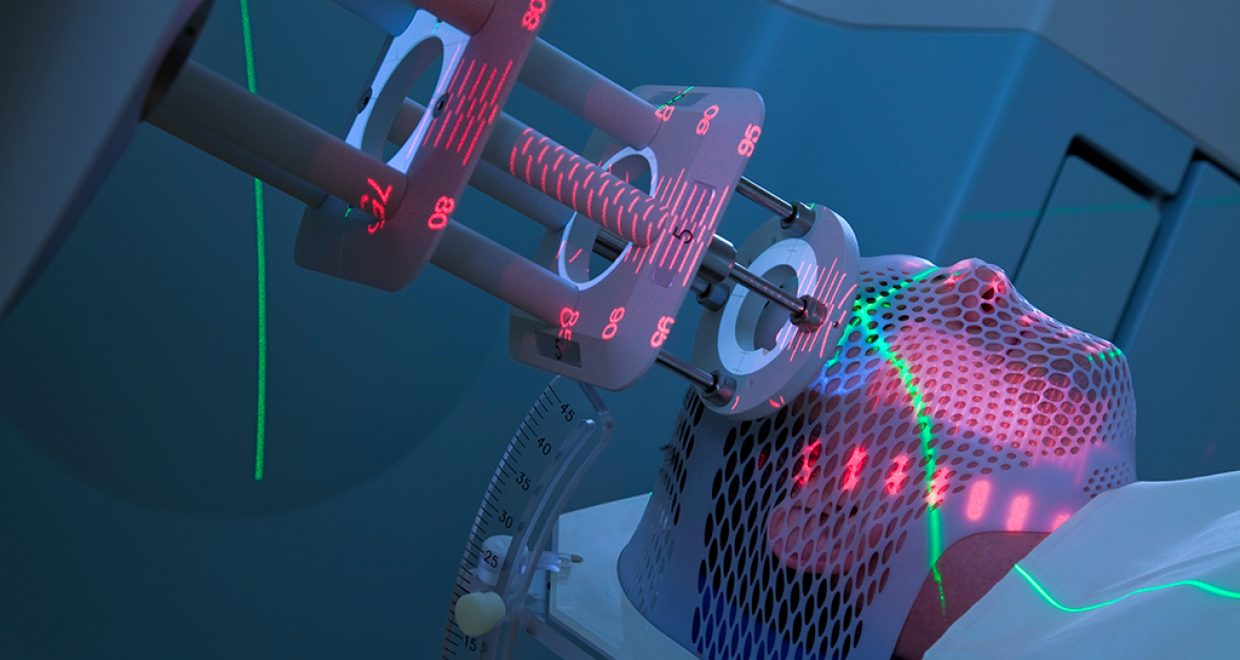
Machines may soon replace healthcare workers in some aspects of their traditional roles. Artificial intelligence (AI) is increasingly mastering rule-based tasks, and acting as a powerful decision-making tool and monitoring system to support clinicians. Providers in Radiation Medicine are becoming familiar with the ways in which AI could both augment care and necessitate a shift in professional roles
While related innovations could create major efficiencies and improvements in care, it could lead to job loss and to ethical and legal risks for those working alongside AI. Some healthcare professions are convening task groups and putting out calls to action to highlight the role that must be taken by the professions to define their own future within an AI-enabled practice environment (1,2). Those at the front lines are beginning to acknowledge the increasing hype in the lay media about job loss risk, no longer limited to grocery clerks and truck drivers, but extending now to lawyers, doctors, and others whose main capital is knowledge.
Radiation Medicine is a valuable AI testing ground. It is adept at adapting to novel technologies, being heavily reliant on both computer software systems and large and complex medical machines to provide care. Examples of automation and machine learning in radiation medicine have emerged in recent years. Providers are becoming familiar with the ways in which AI could both augment care and necessitate a shift in professional roles (3). This provided a useful environment to get a sense of front line perspectives on the fears, opportunities, and needs in preparing for AI. The results of a series of professional focus groups were published in the Journal of Radiotherapy in Practice in the fall of 2018 (4).
From the paper’s abstract: “Staff trained in the absence of these tools form complex views on their value and impact…. It is important to consider how professionals perceive AI to be proactive in informing change, as gains in quality and efficiency will require new workflows, skills, and education.” Insight such as that gleaned in this paper can provide valuable guidance to healthcare administrators, regulatory bodies, and academic training programs, suggesting where efforts might best be directed to prepare professionals to practice in an AI-enabled world.
There are a number of considerations, not explored in this paper and not unique to healthcare that will require attention moving forward, including policy, regulation, and health human resource (HHR) issues. Policy considerations require bringing together actors in healthcare and in technology, with accompanying regulatory initiatives that have not caught up with recent commercial advances, all further complicated by the fact that AI is not a single technology or discovery, but rather a series of advancements with diverse origins and political and social implications, well beyond healthcare.
AI strategies have immense potential to standardize and improve care in many domains, and yet there are considerations that must be addressed to ensure strategies are implemented responsibly and that HCP are equipped and protected. It is hoped that in the near future, many more empirical studies, policy analyses, and implementation science projects will emerge to inform best practice in this area.
The paper “Professional implications of introducing artificial intelligence in healthcare: an evaluation using radiation medicine as a testing ground” is published by the Journal of Radiotherapy in Practice and is available free for a month.
- Thompson, R.F., et al. (2018). Artificial intelligence in radiation oncology: a specialty-wide disruptive transformation? Radiotherapy & Oncology, 129(3): 421-426.
- Tang, A., Tam, R., Cadrin-Chenevert, A., Guest, W., Chong, J., Barfett, J., Chepelev, L., Cairns, R., Mitchell, R., Cicero, M.D., Poudrette, M.G., Jaremko, J.L., Reinhold, C., Gallix, B., Gray, B., Geis, R., for the Canadian Association of Radiologists (CAR) Artificial Intelligence Working Group. (2018). Canadian Association of Radiologists White Paper on Artificial Intelligence in Radiology. Canadian Association of Radiologists Journal, 69; 120-135.
- Purdie, T.G., Dinniwell, R.E., Letourneau, D., Hill, C., Sharpe, M.B. (2011). Automated planning of tangential breast intensity-modulated radiotherapy using heuristic optimization. International Journal of Radiation Oncology*Biology*Physics, 81(2):575-583
- Gillan, C., Milne, E., Harnett, N., Purdie, T.G., (2018). Professional implications of introducing artificial intelligence in healthcare: an evaluation using radiation medicine as a testing ground. J Radiotherapy in Practice. https://doi.org/10.1017/S1460396918000468