Psychotic symptoms in frontotemporal dementia: a diagnostic dilemma?
The April International Psychogeriatrics Article of the Month is entitled “Psychotic symptoms in frontotemporal dementia: a diagnostic dilemma?” by Maria Landqvist Waldö, Lars Gustafson, Ulla Passant and Elisabet Englund.
Despite all attempts to develop clinical diagnostic criteria with high specificity and sensitivity early diagnosis in FTD remains a challenge, even for the experienced clinician. The patients may present with a wide range of symptoms that often mimic other psychiatric disorders and initial psychiatric diagnoses are common. Psychotic symptoms are known to be prominent symptoms in several neurodegenerative diseases including AD and DLB, and have previously been thought to be quite rare in FTD. There are indications that a high prevalence of psychotic symptoms seems to be associated with specific molecular and genetic subgroups of FTD, but as this has not been adequately studied we examined prevalence of psychotic symptoms and possible correlations to brain pathology in FTD. Furthermore we evaluated clinical diagnostic accuracy as well as family history in our cohort of 97 neuropathologically diagnosed FTD cases.
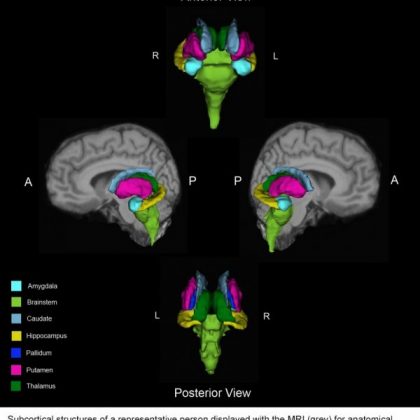
We found that psychotic symptoms were present at some time during the course of dementia in 32% of our cases. There were no significant differences in gender, age at onset or disease duration between patients with and without psychotic symptoms. The most common type of psychotic symptoms was paranoid ideas (20.6%) followed by hallucinations and delusions (17.5%) in equal measure. There was a strong significant correlation between psychotic symptoms and predominantly right-sided brain degeneration.
We could see a trend with more frequent psychotic symptoms in tau-negative cases, however not statistically significant. Psychotic symptoms were particularly common in the cases with FUS pathology and in those without identified brain protein pathology.
The majority of patients received other first diagnoses than FTD, often psychiatric diagnoses. The patients with an initial psychiatric diagnosis were significantly younger than patients with other first diagnoses. About 80% patients where subsequently diagnosed with FTD and among these the median time from symptom onset until diagnosis was 4 years with median disease duration of 7.5 years, however with large variations. A clinical diagnosis of psychosis was almost exclusively given to tau-negative cases.
This is one of the largest studies aimed at assessing the prevalence of psychotic symptoms in FTD and relating them to neuropathology. Compared to many other studies we found a higher prevalence of psychotic symptoms. A correlation between psychotic symptoms and right-sided predominant pathology has been suggested earlier, but to our knowledge never shown in such a large neuropathological study. Although previous studies have found differences in the prevalence of psychotic symptoms between tau-positive and tau-negative cases, we did not find any significant differences between the groups. We identified two groups with particular high prevalence of psychotic symptoms: the FUS pathology cases and those with no identified protein pathology. Our FUS cases share many features with previous reports of this specific group such as young age at onset, no heredity for dementia and prominent neuropsychiatric symptoms. Interestingly, the cases from the group without specific protein pathology also display prominent psychiatric symptoms.