Orcs vs. Trolls: Decisions, Divisions, and Disease
We are living in a world of increasing social divisions that shape the way we interact with one another. Do these social divisions also affect our health? After all, from children eating cake sprinkled with a bit of saliva from an over exuberant birthday boy to fans exchanging jeers and airborne particles at the championship game, our social behaviors are regularly seized on by pathogens as opportunities to infect new hosts. Beyond potential fodder for gossip on local message boards, the way that we interact with our neighbors may determine how infectious diseases spread between us. In our new paper Social divisions and risk perception drive divergent epidemics and large later waves, we develop a mathematical model to show how group differences in risk perception and behavior can transform how outbreaks unfold.
In our model, individuals adopt protective behaviors that reduce transmission (e.g., wearing a mask or getting vaccinated) as they become aware of severe disease-linked outcomes like deaths. This kind of feedback between disease and behavior may change the shape of an epidemic (Arthur et al., 2021; Weitz et al., 2020), or increase the level of protective behavior necessary to prevent outbreaks (Herrera-Diestra & Meyers, 2019). Awareness-based models generally assume that awareness is either global, based on disease impacts across the full population, or local, based on disease impacts in one’s social network (Funk et al., 2010). Here, we focus on an intermediate level of awareness based on population subgroups. We also introduce the concept of awareness separation, which describes when members of one group are more responsive to disease-linked mortality in their own group versus other groups.
We start out by splitting the population into two groups. Let’s call one of them trolls and the other one orcs. Trollsstart out at a disadvantage, as the pathogen starts spreading in this group. On top of awareness separation, we consider mixing separation, or more contact with one’s own group versus the opposite group (Figure 1). When mixing is uniform individuals interact with members of their own group and the opposite group at equal rates. The epidemics in both groups are identical because the pathogen spreads quickly from trolls to orcs.
When mixing is separated (i.e., contacts are primarily within one’s own group), it takes longer for the pathogen to reach the orcsand awareness separation becomes important. If awareness is uniform, the orcs areaware of the initial troll deathsand adopt protective measures early, reducing the size of their epidemic. For opposite reasons, the trollsexperience an even larger epidemic. When awareness is separated, the orcs have little awareness of troll deaths. Orcs ignore the early warning to their own peril, winding up with the same total and peak infection prevalence as the trolls despite having more time to protect themselves.
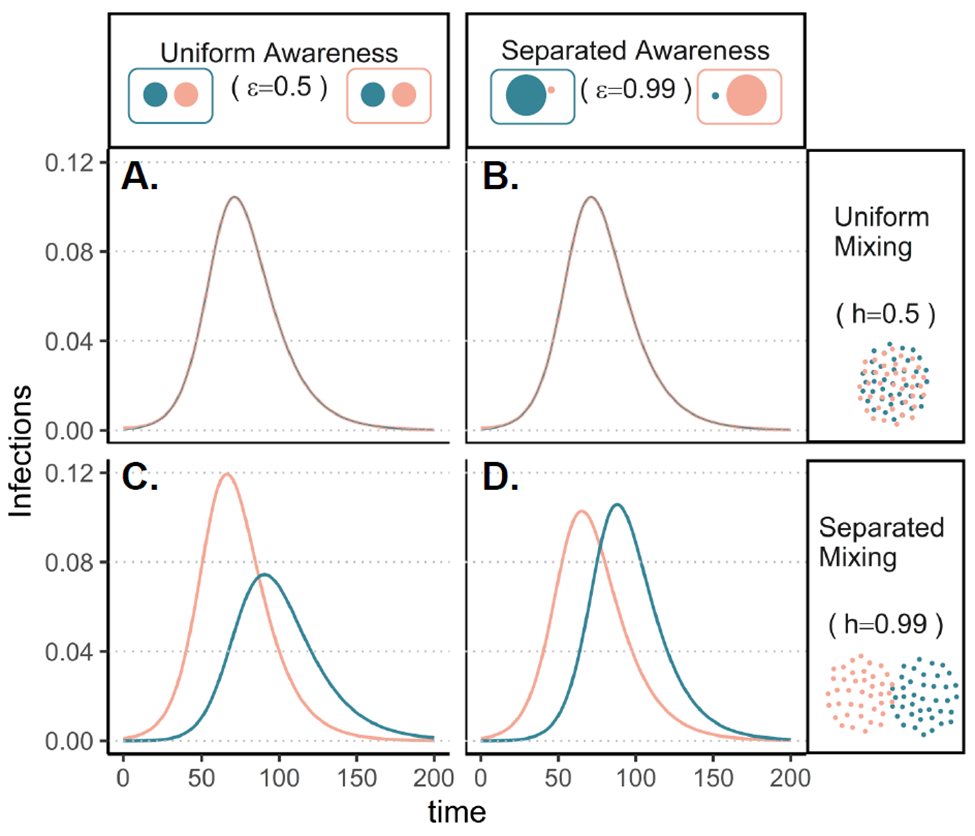
Figure 1: Awareness and mixing separation interact to determine epidemic shape and size. Each panel shows infections over time in trolls (pink) and orcs (green) assuming the pathogen first emerges in trolls only. We consider uniform mixing (top row), separated mixing (bottom row), uniform awareness (left column), and separated awareness (right column). Note that the groups experience basically identical epidemics under uniform mixing (top row), so the lines overlap.
Eventually, orcs and trolls (and even humans) may get tired of being protective. After all, non-pharmaceutical interventions can be uncomfortable or costly to maintain. So we incorporate fatigue, or the gradual abandonment of protective measures over time, into the model. As protective behavior prevalence drops, transmission increases again, leading to two more epidemic waves. When awareness is separated, the later waves are smaller than the initial wave.
When awareness is uniform, the orcs can experience later waves thatare actually larger than the first wave (Figure 2). Protective behavior helped the orcs avoid a large initial wave, but that means that many orcs remain susceptible as transmission picks back up. Compounding the problem, orcsunderestimate their own risk because of their awareness of the trolls, who have much smaller later waves.
Stepping back from trolls and orcs, our model qualitatively resembles trends from the first years of the Covid-19 pandemic in the United States. Some states experienced one large early outbreak and then low transmission for the rest of the year, while other states had a smaller initial wave and larger summer and winter waves. Lots of factors probably contributed to these patterns, including climate and public health ordinances, so these simulations cannot establish causation. However, protective behavior based on risk perception may help to explain complicated epidemic dynamics observed in real life.
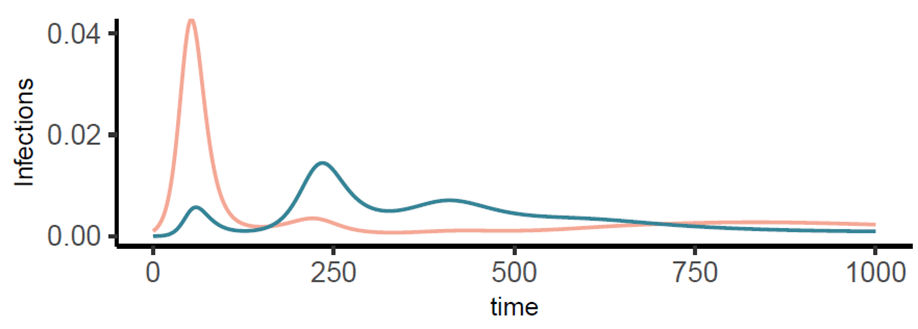
Figure 2: As protective behavior is abandoned, orcs can experience second and third waves that exceed the first wave in size. Infections over time given uniform awareness and separated mixing in orcs (green) and trolls (pink).
Finally, we consider awareness-based vaccine uptake. Trollsstart out at a disadvantage again, but this time they are twice as likely to die from an infection compared to orcs. Trollsrespond to their greater risk by becoming vaccinated at a greater rate. Although risk-based behavior reduces the gap between the two groups, it does not eliminate the difference. This suggests that health equity may not be achieved by individual behavior alone, underscoring the importance of interventions targeted at addressing root causes of health disparities.
Our model also shows how interactions between behavior and immunity can lead to counterintuitive outcomes. We assume that immunity from infection or vaccination provides long-term protection against mortality but waning protection against infection. At high levels of immune protection, cumulative infections actually increase with better immunity, even when immunity protects against infection. This is because better immune protection reduces mortality, leading to lower perceived risk and lower vaccine uptake.
Through simulations, we have shown how group differences in risk perception can fundamentally alter epidemic dynamics. An exciting next step is to link this theoretical model with data on how people actually make decisions based on their disease awareness and group membership. Accounting for social divisions and human behavior may help us better understand how humans are affected by and respond to infectious diseases.
Our model can be explored further using an interactive website developed by undergraduate researcher Kimberly Cardenas.
Mallory Harris is a PhD candidate in the Mordecai lab in the Stanford Department of Biology and an ARCS Foundation Scholar. Mallory uses quantitative methods to study the interplay between human behavior and infectious diseases.
Works Cited
Arthur, R. F., Jones, J. H., Bonds, M. H., Ram, Y., & Feldman, M. W. (2021). Adaptive social contact rates induce complex dynamics during epidemics. PLOS Computational Biology, 17(2), e1008639. https://doi.org/10.1371/journal.pcbi.1008639
Funk, S., Salathé, M., & Jansen, V. A. A. (2010). Modelling the influence of human behaviour on the spread of infectious diseases: A review. Journal of The Royal Society Interface, 7(50), 1247–1256. https://doi.org/10.1098/rsif.2010.0142
Herrera-Diestra, J. L., & Meyers, L. A. (2019). Local risk perception enhances epidemic control. PLOS ONE, 14(12), e0225576. https://doi.org/10.1371/journal.pone.0225576
Weitz, J. S., Park, S. W., Eksin, C., & Dushoff, J. (2020). Awareness-driven behavior changes can shift the shape of epidemics away from peaks and toward plateaus, shoulders, and oscillations. Proceedings of the National Academy of Sciences, 117(51), 32764–32771. https://doi.org/10.1073/pnas.2009911117






