Introduction
Body-focused repetitive behaviours (BFRBs) encompass a range of behaviours including skin picking, hair pulling, nail-biting or lip-cheek biting (Grant et al., Reference Grant, Stein, Woods and Keuthen2012; Houghton et al., Reference Houghton, Alexander, Bauer and Woods2018) and the corresponding disorders are subsumed under the section obsessive-compulsive and related disorders in the DSM-5 (American Psychiatric Association, 2013).
BFRBs are more common than previously thought (Sampaio and Grant, Reference Sampaio and Grant2018). In fact, most people engage in subclinical forms of nail biting (up to 64%) and skin picking (up to 92%), while lip-cheek biting occurs in approximately 40% of the population; habitual hair pulling is observed less often at only 10% (Houghton et al., Reference Houghton, Alexander, Bauer and Woods2018). Prevalence rates vary largely depending on criteria/instruments applied and often diminish to less than 5% if harm (e.g. bleeding in skin picking, bald spots in trichotillomania) or severe interference are included as mandatory criteria (Houghton et al., Reference Houghton, Alexander, Bauer and Woods2018). BFRBs are ‘hidden disorders’, particularly due to shame, and are thus under-diagnosed and under-treated (Najera, Reference Najera2022; Sampaio and Grant, Reference Sampaio and Grant2018). Currently, only skin picking and trichotillomania are recognized as distinct diagnoses in the DSM-5. Classification of pathological lip-cheek biting (cavitadaxia), for example, is scattered across several codes in diagnostic manuals (Moritz et al., Reference Moritz, Müller and Schmotz2020). For some behaviours (e.g. bruxism and joint cracking), status as BFRBs remains controversial.
Comorbidity across BFRBs is high. In a large sample of college students, the majority (71.8%) reported at least one BFRB; 53% of those with subclinical forms had more than one BFRB (Houghton et al., Reference Houghton, Alexander, Bauer and Woods2018). Similar results emerged in a study by our research group on 113 individuals with BFRBs, where 53.1% reported more than one BFRB and 16.8% disclosed at least three BFRBs (Moritz et al., Reference Moritz, Penney, Ahmed and Schmotz2021). In a recent study of 52 children with BFRBs, 39% displayed more than one BFRB (Selles et al., Reference Selles, La Buissonnière Ariza, McBride, Dammann, Whiteside and Storch2018).
Previous research suggests that BFRBs share important similarities in terms of phenomenology and course of illness, as well as with respect to certain etiological, genetic and maintaining factors, whereby the evidence base is most robust for skin picking and trichotillomania (Hartmann et al., Reference Hartmann, Staufenbiel, Bielefeld, Buhlmann, Heinrichs, Martin, Ritter, Kollei and Grocholewski2020; Johansson et al., Reference Johansson, Grant, Kim, Odlaug and Götestam2009; Monzani et al., Reference Monzani, Rijsdijk, Harris and Mataix-Cols2014; Odlaug et al., Reference Odlaug, Lust, Schreiber, Christenson, Derbyshire and Grant2013; Roberts et al., Reference Roberts, O’Connor and Bélanger2013; Snorrason et al., Reference Snorrason, Belleau and Woods2012a; Stein et al., Reference Stein, Flessner, Franklin, Keuthen, Lochner and Woods2008). Transdiagnostic research across the spectrum of obsessive-compulsive and related disorders (OCRD) suggests a distinct higher-order factor, which includes skin picking and trichotillomania and correlates with a second factor including obsessive-compulsive disorder, hoarding disorder and body dysmorphic disorder (Snorrason et al., Reference Snorrason, Beard, Peckham and Björgvinsson2021). This is also in line with Maraz et al. (Reference Maraz, Hende, Urbán and Demetrovics2017) who provide evidence for a single grooming factor behind skin picking, trichotillomania and nail biting. The current evidence thus supports BFRB as a distinct category of behaviours that share phenomenological and etiological similarities.
A trans-symptomatic scale for adults with BFRBs currently does not exist. Such an instrument, however, is needed in view of the aforementioned high co-morbidity and similarities across various BFRBs that appear to qualify it as a distinct diagnostic entity (Maraz et al., Reference Maraz, Hende, Urbán and Demetrovics2017; Snorrason et al., Reference Snorrason, Beard, Peckham and Björgvinsson2021). A trans-symptomatic scale has advantages over symptom-specific scales. For example, it may allow comparison of symptom profiles, pathogenetic mechanisms or treatment effects in different BFRB populations (e.g. skin picking vs trichotillomania). Current symptom-specific scales do not only differ with respect to target symptoms, but also to criteria (e.g. consideration of visible impairment due to BFRB). The wording of response options thus affects psychometric properties and sensitivity to change. As a result, the same treatment may appear more effective in one BFRB than in another simply due to differences in measurement. Moreover, a generic BFRB scale saves time relative to the administration of multiple disorder-specific scales.
The present study
This study explored the psychometric properties of the Generic BFRB Scale-8 (GBS-8), a newly developed transdiagnostic scale which was inspired by the Skin-Picking Scale-Revised in terms of item formulation (SPS-R; Snorrason et al., Reference Snorrason, Ólafsson, Flessner, Keuthen, Franklin and Woods2012b), and the Yale-Brown Obsessive Compulsive Scale (Y-BOCS; Goodman et al., Reference Goodman, Price, Rasmussen, Mazure, Delgado, Heninger and Charney1989). We specifically assessed the factor structure, test–retest reliability and stability of the GBS-8 (we also examined the number of BFRBs as a potential moderator), and examined its concurrent validity against the Repetitive Body Focused Behavior Scale (RBFBS, slightly adapted for self-report in adults; Selles et al., Reference Selles, La Buissonnière Ariza, McBride, Dammann, Whiteside and Storch2018) as well as divergent validity against scales measuring depression symptoms and quality of life. We expected weak correlations with quality of life and depression scales (divergent validity) and strong correlations with the RBFBS (concurrent validity). Finally, we also explored whether psychometric properties were worse in individuals with more BFRBs.
Method
Sample
The study was advertised as an unguided treatment study for individuals with BFRBs (different manifestations were described). Inclusion criteria were to be between 18 and 75 years of age, with at least one current self-reported BFRB. The final analyses included data from 279 participants. A diagnosis of schizophrenia, suicidal ideation, refusal to provide informed consent and poor command of the English language represented exclusion criteria. The study is part of a larger randomized controlled trial comparing a wait-list control group with an experimental group receiving a self-help manual entitled ‘Free from BFRB’ (Moritz et al., in preparation).
Invitation, baseline and follow-up
The study was conducted online using the Questback/Unipark® survey platform and was advertised on English-speaking Facebook forums targeting people with BFRBs (e.g. forums on nail-biting, skin picking and BFRB in general) as well as on our website (www.uke.de/decoupling). Incentives for participation included free access to self-help manuals and a smartphone application (see www.uke.de/cogito_app). The landing page described the study aims and inclusion criteria, and was followed by an electronic informed consent form (mandatory precondition for participation). Questions on age and gender followed. We then asked whether individuals had ever (i.e. lifetime prevalence) suffered from skin picking, nail biting, hair pulling (trichotillomania), biting at/of the skin (or mouth). Moreover, visible consequences of the behaviour (e.g. severely bitten nails), and impairment in social, professional, and/or other important areas of life due to the behaviour were assessed. The same questions were then posed again after six weeks but with the time frame confined to the last two weeks. This was followed by questions regarding medical history (e.g. other psychiatric diagnoses; current pharmacological treatment). The GBS-8, the adapted version of the RBFBS, the WHO Quality of Life-BREF global item (WHOQOL-BREF; Skevington et al., Reference Skevington, Lotfy and O’Connell2004) and the Patient Health Questionnaire-9 (PHQ-9; Kroenke et al., Reference Kroenke, Spitzer and Williams2001) were then administered (see below). Following this, participants were asked whether they had answered all questions truthfully (yes/no; participants were excluded from the study in the event of a ‘no’ response). Afterwards, participants were asked to provide an email address that would not identify them (or to create one for the purpose of the study), and were then automatically randomized to one of two conditions. Six weeks after the baseline assessment, all participants were automatically invited via email to take part in a follow-up assessment. Participants were asked to re-enter the email address they had used before, and were then requested to respond to the same psychological scales administered at baseline, this time all referring to the last week.
Generic Body-Focused Repetitive Behavior Scale-8 (GBS-8)
BFRBs were measured with the Generic Body-Focused Repetitive Behavior Scale-8 (GBS-8). The scale builds upon the items of the Skin Picking Scale (SPS; Keuthen et al., Reference Keuthen, Deckersbach, Wilhelm, Engelhard, Forker, O’Sullivan, Jenike and Baer2001) in its revised 8-item form (SPS-R; Snorrason et al., Reference Snorrason, Ólafsson, Flessner, Keuthen, Franklin and Woods2012b). The SPS-R has good reliability, which has been corroborated for the German version (Cronbach’s alpha = .93; Gallinat et al., Reference Gallinat, Keuthen and Backenstrass2016); the convergent validity was confirmed with the Skin Picking Impact Scale (Mehrmann et al., Reference Mehrmann, Hunger and Gerlach2017). Similar to the Y-BOCS (Goodman et al., Reference Goodman, Price, Rasmussen, Mazure, Delgado, Heninger and Charney1989), which requests a joint rating for different OCD symptoms (e.g. a pooled estimate for washing, checking and other symptoms), we revised the scale to capture different forms of BFRBs by asking for a joint rating in the event that participants suffered from various BFRBs. We modelled the GBS-8 on the SPS-R rather than the RBFBS, described below, as the RBFBS has been developed for children and unlike SPS-R does not assess important diagnostic criteria such as avoidance and damage.
The GBS-8 instruction was as follows: ‘For each item, pick the one answer which best describes the past week. If you have been having ups and downs, try to estimate an average for the past week. Please be sure to read all answers before making your choice’. In situations where the context is less clear, we advise researchers to add the following introduction: ‘The following scale asks about symptoms related to body-focused repetitive behaviour disorder (BFRB). Individuals with BFRB feel an urge to repeatedly engage in dysfunctional activities that involve their body, such as nail biting, skin picking, hair pulling, or lip-cheek biting, and repeatedly try to stop these activities’. Every item had to be scored on a 5-point Likert scale ranging from 0 to 4. The time frame was set to the past week for both the baseline and post-assessment. The following items were assessed (see Appendix in Supplementary material for exact wording; items and response options are abbreviated): (1) frequency of the urge to perform BFRB, from 0 (no urges) to 4 (extreme); (2) intensity of the urge to perform BFRB, from 0 (minimal or none) to 4 (extreme); (3) time spent on BFRB, from 0 (none) to 4 (extreme); (4) control over BFRB, from 0 (complete control) to 4 (no control); (5) emotional distress because of BFRB, from 0 (no emotional distress) to 4 (extreme); (6) interference with social or work life because of BFRB, from 0 (none) to 4 (extreme); (7) avoidance because of BFRB, from 0 (not at all) to 4 (extreme); and (8) damage because of BFRB, from 0 (none) to 4 (extreme). In line with the factor structure of the SPS-R obtained in the original study (Snorrason et al., Reference Snorrason, Ólafsson, Flessner, Keuthen, Franklin and Woods2012b), we calculated a total score as well as symptom severity subscale (items 1–4) and an impairment subscale (items 5–8).
Repetitive Body Focused Behavior Scale (RBFBS; concurrent validity)
The RBFBS (Selles et al., Reference Selles, La Buissonnière Ariza, McBride, Dammann, Whiteside and Storch2018) is a 12-item scale originally assessing parents’ observations of their child’s BFRBs. Parents first endorse whether or not a specific BFRB is present in their child. If absent, parents proceed to rate the next BFRB. If a BFRB is present, the behaviour is rated on three criteria (time spent, interference, and distress) using a 5-point Likert scale ranging from none (0) to extreme (4) for the past week. The item contains descriptions to facilitate ratings. Total severity scores are calculated for each BFRB scale. Internal consistency of the parent version is good to excellent (α = .86–.93). An unpublished self-report scale also exists for children to rate their symptoms on the same items. For the present study, we adapted the self-report scale for use with adults (e.g. we assessed problems at school or the workplace instead of school only and inquired about possible problems with family rather than fights with family).
Other scales (divergent validity)
The WHO Quality of Life-BREF (WHOQOL-BREF; Skevington et al., Reference Skevington, Lotfy and O’Connell2004) global item (‘How would you assess your quality of life?’) was used as an index of quality of life (QoL) for the prior two weeks [response options: very poor (1) to very good (5)].
The Patient Health Questionnaire-9 (PHQ-9; Kroenke et al., Reference Kroenke, Spitzer and Williams2001) is a self-report instrument to measure depression, derived from the Primary Care Evaluation of Mental Disorders. Its nine items capture the core diagnostic criteria of depression. Symptoms are rated on a 4-point scale ranging from not at all (0) to almost daily (3). Its psychometric properties are good (Gilbody et al., Reference Gilbody, Richards, Brealey and Hewitt2007). Items referred to the last two weeks.
Strategy of data analysis
We entered the eight GBS items into a varimax-rotated exploratory factor analysis and verified the solution using oblique rotation. Concurrent validity was tested against the RBFBS, while divergent validity was tested against the PHQ-9 and global WHOQOL-BREF item. For test–retest reliability, we correlated baseline and post scores from the wait-list control group only given expected strong variability of symptoms in the intervention group.
Results
Baseline characteristics are reported in Table 1. All information relies on self-report. The majority of participants were female in their early thirties. Most had an additional diagnosis with two out of five being diagnosed with anxiety and depression. Skin picking was the most prevalent lifetime and current BFRB. Trichotillomania was reported the least.
Table 1. Baseline characteristics of the sample
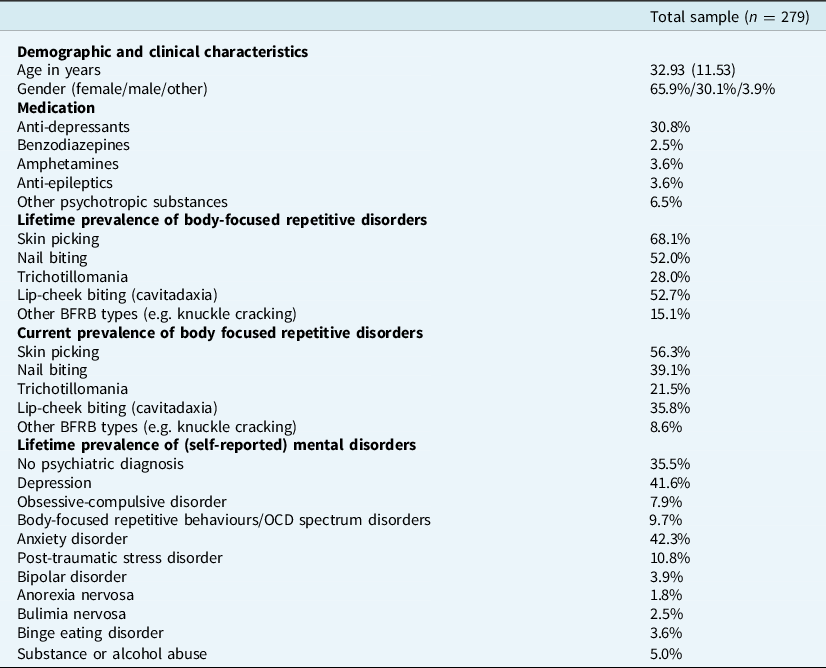
Values are means (standard deviations) and frequencies.
The Bartlett test (p<.001) and Kaiser-Meyer-Olin measure (.817) of the factor analysis were satisfactory. Two factors emerged from the varimax-rotated solution both after adopting the Kaiser-Guttmann criterion (explained variance: 64%) and scree plot inspection. Items 1–4 loaded on the first factor called symptom severity (frequency of urge: .86; time: .80; intensity of urge: .76; control: .54; loadings on factor 2 <.29). Items 5–8 loaded on factor 2, labelled impairment (avoidance: .86; interference: .83; damage: .74; emotional distress: .69; loadings on factor 1 <.34). Similar results emerged when an oblique rotation was sought (explained variance: 63.57%; items 1–4 loaded on one factor, loading: >.49: 17.00% explained variance; items 5–8 loaded on another factor, loading >.66, 46.57%; loadings of items on the respective other factor were always lower than |.2|.
The GBS-8 total score significantly correlated with the RBFBS scales at r = .74 (p<.001; GBS-8 impairment: r = .67, p<.001; GBS-8 symptom severity: r = .60, p<.001). The test–retest reliability of the GBS-8 was r = .72 (p<.001; impairment: r = .67, p<.001; symptom severity: r = .73, p<.001; results refer to participants in the wait-list control group with less fluctuations). Similar test–retest reliability was observed for the PHQ-9 (r = .76, p<.001) and the global WHOQOL-BREF item (r = .69, p<.001). Divergent validity of the GBS-8 was tested against the PHQ-9 and QoL; correlations were modest (baseline: PHQ-9, r = .39, p<.001; QoL, r = –.30, p<.001) and far lower than with the RBFBS (i.e. concurrent validity). A test for correlational differences was significant in both cases (p<.001). Internal consistency of the GBS-8 was good (total score: Cronbach’s α = .84; symptom severity: α = .77; impairment: α = .82).
We also explored whether psychometric properties were worse in individuals with more BFRBs (at least 3) versus those with two or less. If true, this would speak to problems in integrating different BFRBs into a single score, which was not the case (participants with at least three BFRBs: Cronbach’s alpha = .80; test–retest reliability: r = .75, p<.001; participants with two or fewer BFRBs: Cronbach’s alpha = .84; test–retest reliability: r = .67, p<.001).
Discussion
Similar to the SPS-R, from which the newly developed GBS-8 was derived, two dimensions emerged following factor analysis: symptom severity (items 1–4) and impairment (items 5–8). The GBS-8 and its subscales showed high internal consistency and satisfactory test–retest reliability, comparable to other established scales. Convergent validity, tested against the RBFBS, was good, while there was significantly less correlation with measures of general psychopathology/well-being (i.e. depression/quality of life), thus supporting divergent validity. Psychometric properties were similar for people with few or several BFRBs, indicating that participants can apply the items to their behaviours even if multiple BFRBs are present. Yet, results should be considered as preliminary until independent replication.
We recommend usage of the GBS-8 as a complement to symptom-specific BFRB scales in clinical trials. A transdiagnostic scale is important given the high co-morbidity of BFRBs, its functional, symptomatic, and potential genetic similarities, as well as growing evidence for the usefulness of the BFRB construct as a superordinate diagnostic entity. The GBS-8 can inform researchers, for example, about discrepant effects in terms of efficacy of the same treatments for various BFRBs, for example if Habit Reversal Training is more efficient in those with predominant nail biting than in those with predominant skin picking. As mentioned, varying effects of the same treatment techniques in different BFRBs may not always reflect real differences but could in part be due to divergent psychometric properties of symptom-specific scales and item content (e.g. a scale with an emphasis on visible consequences that manifest only over longer durations may be less sensitive to change than a scale measuring momentary severity).
Some caveats need to be acknowledged. A self-report scale like the GBS-8 is limited with respect to its objectivity. Scales such as the original RBFBS are superior in this regard as they gather information from both the individual with BFRB (i.e. child) and an outside observer (i.e. the child’s parent). However, many adults with BFRBs are reluctant to disclose their problem to others or seek support due to feelings of shame (Gallinat et al., Reference Gallinat, Moessner, Haenssle, Winkler, Backenstrass and Bauer2019; Weingarden and Renshaw, Reference Weingarden and Renshaw2015) which limits the availability/feasibility of external ratings. Future research should also test whether a paper-and-pencil format of the GBS-8 provides comparable results as an online version (see Carlbring et al., Reference Carlbring, Brunt, Bohman, Austin, Richards, Öst and Andersson2007; Vallejo et al., Reference Vallejo, Jordán, Díaz, Comeche and Ortega2007). Our results await replication using confirmatory factor analysis.
While the GBS-8 is a useful global outcome measure, scales such as the RBFBS that provide indexes for different BFRBs can inform researchers to what extent a treatment is effective for the target BFRB only, or whether it also impacts other BFRBs (i.e. generalized positive effects versus ‘displacement’/adverse events on other BFRB subtypes). We are currently testing such a multi-dimensional scale (e.g. Schmotz, Reference Schmotz2021), which may help to elucidate discrepant effects (e.g. worsening in one but improvement in another BFRB). Such a scale may also decrease the effort to pool scores in the event of concurrent BFRBs. We also need to acknowledge that the RBFBS was a modification of the original scale and only represented the self-report section. Finally, replication in other samples is recommended, as, for example our sample was restricted to help-seeking individuals and consisted mainly of females. Investigations in subclinical (general population) samples are also needed to test the robustness and generalizability of the two-factor solution.
To conclude, the GBS-8 is a brief, reliable and valid scale. Its total score may serve as a global primary outcome in trials on BFRBs, while its subscales can inform about specific aspects of BFRB.
Supplementary material
To view supplementary material for this article, please visit: https://doi.org/10.1017/S1352465822000327
Data availability statement
Data are available on request from the corresponding author.
Acknowledgments
The authors wish to thank all who participated in this study.
Author contributions
Steffen Moritz: Conceptualization (equal), Data curation (equal), Formal analysis (equal), Investigation (equal), Methodology (equal), Project administration (equal); Christina Gallinat: Validation (equal), Writing – review & editing (equal); Sarah Weidinger: Conceptualization (equal), Formal analysis (equal), Investigation (equal); Alina Bruhns: Conceptualization (equal), Formal analysis (equal), Writing – original draft (equal), Writing – review & editing (equal); Despina Lion: Methodology (equal), Writing – original draft (equal), Writing – review & editing (equal); Ivar Snorrason: Formal analysis (equal), Methodology (equal), Writing – original draft (equal), Writing – review & editing (equal); Nancy Keuthen: Formal analysis (equal), Methodology (equal), Writing – original draft (equal), Writing – review & editing (equal); Stella Schmotz: Formal analysis (equal), Methodology (equal), Project administration (equal), Writing – original draft (equal), Writing – review & editing (equal); Danielle Penney: Conceptualization (equal), Formal analysis (equal), Methodology (equal), Project administration (equal), Supervision (equal), Writing – original draft (equal), Writing – review & editing (equal).
Financial support
The authors received no financial support for the research, authorship, and/or publication of this article.
Conflicts of interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical standards
The trial was registered with the German Clinical Trials Register (DRKS00024525). Ethical approval was obtained from the local ethics committee for psychologists at the University Hospital of Hamburg-Eppendorf (Germany, LPEK-0254). Following the guidelines of the European General Data Protection Regulation, participants’ IP addresses were not stored.



Comments
No Comments have been published for this article.