Introduction
CHD remains the most common among birth defects, with prevalence estimated at 9.4 per 1000 live births. Reference Liu, Chen and Zühlke1 The majority of these lesions are mild or isolated defects. However, significant heart disease can be found in 35% of affected infants. Reference Liu, Chen and Zühlke1 Among these rare lesions is hypoplastic left heart syndrome, accounting for 3% of infants with CHD. Reference Liu, Chen and Zühlke1 Total anomalous pulmonary venous return is even more infrequent, accounting for a separate 1.5% of infants with CHD. Reference Liu, Chen and Zühlke1 In isolation, these defects are fatal without surgical intervention, and particularly for hypoplastic left heart syndrome, successful single ventricle palliation depends on an adequate pulmonary circuit. While there are few reported cases of single ventricle physiology associated with total anomalous pulmonary venous return, it is accepted that those affected have a higher degree of surgical complexity and likely decreased odds of survival. Reference Robinson, Forbess, Slack, Moss and Chaves2 Complete tracheal ring deformities, which are rare formations of excessive cartilage surrounding the trachea, also cause a significant degree of airway stenosis in affected patients. To our knowledge, there is only one reported case of a patient with a concomitant single ventricle defect and tracheal ring deformity. Reference Kawahito, Takano and Egawa3 Here, we present a case of a neonate with hypoplastic left heart syndrome, total anomalous pulmonary venous return, complete tracheal ring deformity, and extracardiac airway malformations.
Case
A 30-year-old healthy multiparous woman underwent routine fetal anatomy ultrasound at 20 weeks and 3 days. Her pregnancy was uncomplicated. Imaging was notable for a markedly abnormal 4-chamber fetal heart view with an abnormal ductal arch and newly noted fetal growth restriction. Subsequent fetal echocardiograms confirmed hypoplastic left heart syndrome with mitral and aortic atresia, an open atrial septum, and qualitatively good single right ventricle function. The coronary sinus was dilated with all visualised pulmonary veins draining into a confluence along the posterior left atrium. Prenatal counselling emphasised the complexity of the cardiac anomalies, along with the additional risk of the fetus’ significant growth restriction. Prenatal neonatal intensive care and cardiothoracic surgery consults were recommended, which the family declined. Fetal growth was tracked on a biweekly basis. By 38 weeks gestation, there was minimal interval growth on repeated scans, so a decision was made to proceed with induction of labour.
A 2.542 kg female neonate was born via uncomplicated spontaneous vaginal delivery at 38 weeks and 2 days completed gestational age. By 2 hours of life, the infant developed respiratory distress and bradycardic arrest lasting less than 60 s. Post-arrest, she had no immediate neurologic sequelae. She was emergently taken for cardiac catheterisation where she was found to have anomalous pulmonary venous return with a tortuous decompressing vein draining to the coronary sinus in addition to a restrictive atrial communication (Fig 1). Multiple attempts at balloon atrial septostomy yielded a small septal defect, which was unsuccessful in achieving adequate decompression. She ultimately underwent placement of an interatrial stent via a hybrid surgical approach. She had improvement in her haemodynamics and oxygen saturations following stent placement, so pulmonary artery banding was deferred. Postoperative echocardiogram demonstrated a mean gradient of 5 mmHg across the stent.
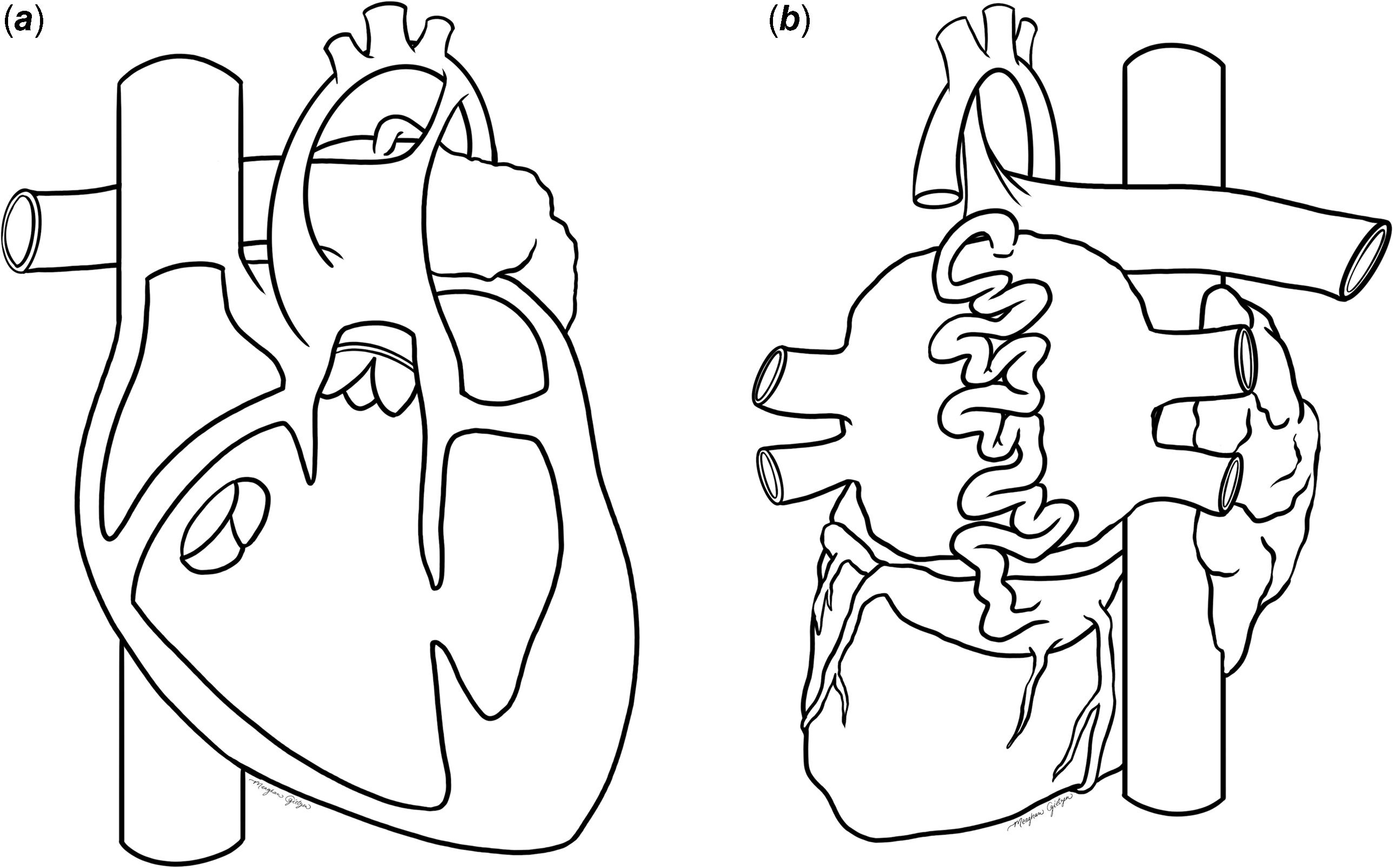
Figure 1. Postnatal cardiac anatomy of affected patient ( a ). Anterior view showing hypoplastic left heart with mitral and aortic atresia, atresia of the left pulmonary artery, patent ductus arteriosus, and marked hypoplasia of the ascending, transverse, and proximal descending aorta ( b ). Posterior view depicting pulmonary venous return into a common confluence with a complex, highly tortuous decompressing vein, with marked dilation of the coronary sinus. Illustrator credited by Meaghan Gietzen.
Despite successful decompression of pulmonary venous return, the infant remained difficult to ventilate, prompting the anaesthesia team to attempt re-intubation with significant resistance. Given ongoing difficulty, she underwent intraoperative bronchoscopy, which revealed tracheal stenosis with multiple complete tracheal rings inferior to the cricoid. Median sternotomy views during the hybrid case raised concern for congenital aplasia of the left bronchus and lung.
Postoperatively, she was admitted to the paediatric cardiothoracic ICU and maintained on vasoactive and inotropic support and prostaglandin E1 for her severely hypoplastic aortic arch. Congenital aplasia of the left bronchus and lung was confirmed by CT (Fig 2). Genetic testing was performed, with a normal postnatal chromosomal microarray. She also underwent screening ultrasonography of the head and abdomen, which were normal. Continuous video electroencephalography monitoring was notable for excessive discontinuity for age, consistent with neurologic dysfunction of an unspecified aetiology.
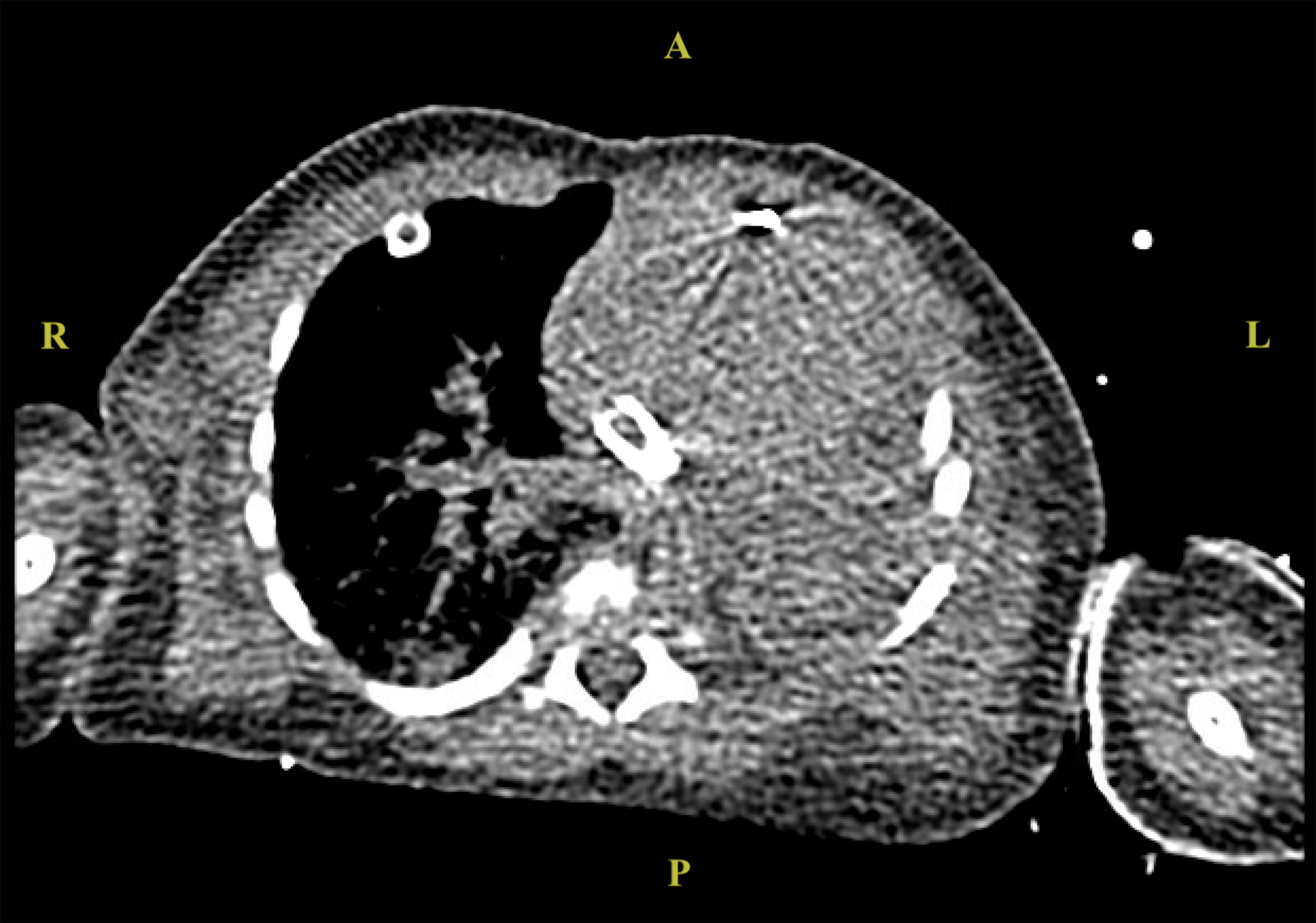
Figure 2. Initial chest computed tomography scan demonstrating absence of left bronchus and lung.
Her case was discussed in our cardiothoracic surgical conference, and she was deemed a potential surgical candidate for hybrid Norwood palliation. However, given the constellation of low birth weight with single ventricle and single lung physiology, she was considered extremely high risk. Her respiratory status remained tenuous with multiple episodes of bronchospasm with respiratory and bradycardic arrests. Her family opted to transition to comfort care, and she died on day of life 8.
Conclusions
In summary, the triad of hypoplastic left heart, pulmonary venous obstruction, and airway malformations poses a lethal constellation. While the single previously reported patient with a combination of single ventricle disease and tracheal pathology survived initial palliation (bidirectional cavo-pulmonary shunt in conjunction with slide tracheoplasty), he had reportedly normal pulmonary venous return. Reference Kawahito, Takano and Egawa3 The ability of the airway to maintain flow is lowest in early infancy; as such, any single ventricle palliation places significant stress on the cardiopulmonary mechanics in patients with CHD. Reference An, Choi and Kwon4 This is further exacerbated by concomitant pulmonary venous obstruction and anatomic airway anomalies. Though our institution has previously performed slide tracheoplasty in conjunction with CHD biventricular repair, our surgeons prefer to reserve this option for patients with a weight greater than 4 kg.
While prenatal imaging yielded crucial information prior to delivery, the extent of cardiac and airway malformations present in this case was not fully appreciable without the advanced imaging performed postnatally. This detailed information allowed for more thorough and specific treatment planning, prognostication, and family counselling, all of which significantly impacted the course of a complex and critically ill patient while striving to determine the extent of medical benefit versus futility. Should this triad be identified in future patients, clearly communicating the expected clinical course in addition to elucidation of the family’s understanding and goals can provide a guide in light of the significant postnatal risk. Early incorporation of multidisciplinary expertise as a routine practice, rather than an opt-in consultation, would also benefit families and medical teams alike.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Competing interests
None.





