Given that survival rates following even complex paediatric cardiac surgery are excellent, there is greater focus on the optimisation of longer-term functional outcomes. Children with CHD who undergo cardiac surgery face an elevated risk of neurological injury and developmental delays for a wide range of reasons, and it is challenging to delineate these complex and often inter-related factors as separate entities. Reference Mebius, Kooi, Bilardo and Bos1 Aetiological mechanisms include genetics, Reference Gaynor, Wernovsky and Jarvik2 abnormalities of brain perfusion before birth, Reference Ruiz, Cruz-Lemini and Masoller3,Reference Masoller, Sanz-Cortés and Crispi4 brain immaturity, Reference Andropoulos, Hunter and Nelson5,Reference Licht, Shera and Clancy6 low oxygen levels, poor condition after birth, Reference Mulkey, Swearingen and Melguizo7 complex heart conditions, Reference Gunn, Beca and Hunt8 a difficult post-operative course after cardiac surgery, Reference Newburger, Wypij and Bellinger9,Reference Read, Ridout and Johnson10 and socio-economic factors. Reference Bucholz, Sleeper and Sananes11 Then in many previous studies, a down-stream neurodevelopmental outcome may be attributed to a range of these different and inter-related factors. Reference Dimitropoulos, McQuillen and Sethi12–Reference Sterken, Lemiere, Vanhorebeek, Van den Berghe and Mesotten14
We previously undertook a prospective multi-centre study in five of the ten paediatric cardiac centres in the UK, in which we monitored children after 3090 consecutive cardiac surgeries Reference Brown, Ridout and Pagel15 and diagnosed post-operative morbidities based on defined criteria. Reference Brown, Pagel and Brimmell16 We used the term morbidity to characterise these post-operative clinical conditions, which were extracorporeal life support, acute neurological event, unplanned re-intervention, feeding problems, major adverse event, prolonged pleural effusion, post-surgical infection morbidity, renal support, and necrotising enterocolitis, because we recognise that although they may be referred to as complications, the causal pathway involves a combination of pre-, intra-, and post-operative variables. A clinically important morbidity (or complication), that is potentially linked to elevated rates of neurodevelopmental delay amongst paediatric cardiac surgery patients, is acute neurological event, when a newly acquired brain injury is identified after surgery. Our wider research study, which involved a prospective monitoring process and data collection, enabled us to undertake this separate sub-study to focus specifically on the diagnosis and characterisation of acute neurological events that came to light in the immediate post-operative period, within the post-operative hospitalisation. In this sub-study, we aimed to describe the incidence of acute neurological event in the complex setting of paediatric cardiac surgery, to describe the association of acute neurological event with other important post-operative morbidities (or complications), and to explore clinical risk factors linked with the study outcome of acute neurological event.
Methods
Design
This is a secondary analysis of a prospectively collected dataset pertaining to a United Kingdom cohort of children who underwent paediatric cardiac surgery. 17
Data collection
As described previously, Reference Brown, Ridout and Pagel15 patients were monitored prospectively following cardiac procedures for the occurrence of defined nine morbidities (or complications) Reference Brown, Pagel and Brimmell16 each of which was assigned to an index preceding cardiac procedure. These were extracorporeal life support, acute neurological event, unplanned re-intervention, feeding problems, major adverse event, prolonged pleural effusion, post-surgical infection morbidity, renal support, and necrotising enterocolitis (See Supplementary Materials Table A). Each of these complications was prospectively diagnosed in the same hospitalisation, excluding unplanned re-operation which was identified within one month and mediastinitis which was diagnosed as linked to the preceding surgery by the operating surgeon. The ascertainment of each complication was undertaken locally, and discrepancies or complex cases were discussed in monthly team meetings involving study team members from all centres, with decisions being made by consensus.
Patient population
All children aged 17 years and below who underwent open, closed, and hybrid cardiac surgery across 5 United Kingdom centres between 01/10/2015 – 30/06/2017 were included. Exclusions were premature babies undergoing patent ductus arteriosus ligation and children having cardiothoracic transplants/tracheal procedures. Participating centres were Great Ormond Street Hospital for Children, Evelina London Children’s Hospital, Birmingham Children’s Hospital, Bristol Royal Children’s Hospital, and the Royal Hospital for Children in Glasgow.
Outcome
Primary outcome
The primary outcome of this study was the complication of acute neurological event occurring as a new finding post-operation within the same hospitalisation as cardiac surgery, defined as 17 “any occurrence of the following: seizures, focal neurological deficit, intracranial haemorrhage, stroke, brain death, hypoxic ischaemic encephalopathy, spinal cord ischaemia, basal ganglia damage, or brainstem injury.”
The acute neurological events were identified by prospective evaluation and clinical scrutiny daily per the study protocol by a dedicated research nurse and clinician for the study. However, the measurement methods were intended for future routine use, and therefore, investigation with electroencephalogram and cross-sectional imaging was only undertaken when there were clinical concerns for an acute neurological event. Children considered to be at high risk of acute neurological event based on clinical history and or emerging clinical signs such as focal neurological signs, altered consciousness not explained by therapies including brain death, seizures, and abnormal movement disorders underwent brain scan (CT or MRI) and electroencephalogram as per usual clinical care. It was recognised that when patients were extremely ill and on life support and sedative medications prior to surgery, exclusion of pre-operative neurological injury is challenging; however, patients who were deemed at risk of this were assessed prior to surgery following local protocols. All detected acute pre-operative neurological injuries and long-standing neurological comorbidities were captured in the study dataset.
Secondary outcomes
Secondary outcomes of the study were length of hospital stay and 6-month survival rates.
Case-mix variables
The candidate variables collected on our study cohort were sex, age band (neonate, infant, child), patient weight, cardiac diagnosis, functionally univentricular heart (yes/no), specific procedure type category, operation type (bypass, non-bypass or hybrid), bypass time, urgency of operation, acquired comorbidity, congenital comorbidity excluding Down syndrome, Down syndrome, additional cardiac risk factors, prematurity, and a pre-operative requirement for critical care supports (severity of illness indicator). For the variables of cardiac diagnosis and cardiac surgical procedure, we noted that there were many variables leading to some categories being sparsely populated. Therefore, these two variable groups were collapsed further to help with clinical interpretation (See Supplementary Table B). Reference Brown, Ridout and Pagel15 All risk variables and sub-categorisations were selected with reference to empiric data on risk of early mortality. Reference Pagel, Rogers and Brown18–Reference Rogers, Brown and Franklin22
Descriptive analysis
We describe the criteria by which acute neurological event was first diagnosed, and we describe the associations between acute neurological events and other complications such as need for extracorporeal life support. We describe the study population by the stated case-mix variables by presence of acute neurological event.
Risk factor selection for statistical analysis
We considered the number of acute neurological events, which was 66 out of the population of 3090, and as such we planned to analyse risk variables involving 7-10 degrees of freedom. Reference Riley, Ensor and Snell23 We considered related literature on risks for neurodevelopmental problems in paediatric cardiac surgery Reference Mebius, Kooi, Bilardo and Bos1–Reference Newburger, Wypij and Bellinger9 as well as the clinical importance of both patient-related and procedure-related factors before selecting risk variables as predictors. We used the following risk variables in our statistical analyses: CHD complexity based on category A-C (more complex diagnoses) versus D–E Reference Brown, Ridout and Pagel15 (less complex diagnoses), neonatal age versus non-neonatal age, critical illness at the time of surgery based on presence or not of a severity of illness factor (ventilation, inotropes or mechanical support), 24 no or short bypass versus bypass time > 90 minutes, and elective surgery versus all types of urgent surgery (urgent, emergency or salvage operations). 24
Primary outcomes
The distribution of each risk variable was evaluated with a Chi-squared analysis. Analysis of risk variables was carried out at procedure level for the complication of acute neurological event (yes or no). Both, a univariate and a multivariable logistic regression, were used to analyse the relationship of prespecified risk variables to acute neurological event.
Secondary outcomes
We undertook univariate comparisons of the secondary outcomes by presence of acute neurological event. Length of hospital stay was analysed as a median with a Kruskal-Wallis statistic. Six-month mortality was assessed at patient level with univariate odds ratio.
Analysis was carried out using Stata.v.16.
Results
The study population
In total, 3090 index cardiac procedures met the inclusion criteria. We noted and excluded 10 misclassified procedures, 63 planned procedures occurring within one month and 143 unplanned reoperations within one month as reported previously. Reference Brown, Ridout and Pagel15,Reference Dorobantu, Ridout and Brown25 The 3090 included procedures included 2861 patients, with 2648 undergoing one procedure, 197 undergoing 2 and 16 having 3 procedures. The median age at procedure was 228 days with an interquartile range of patients in the study of 77–1390 days, and 1671 (54.1%) of the patients were male. The incidence of complications was 675 (21.8%) of which 197 (6.4%) were multiple complications. Acute neurological event was the rarest complication, with total incidence 66 (2.1%). The other complications had overall rates as follows (any occurrence): pleural effusion (6.5%), feeding problems (6.0%), unplanned re-intervention (5.2%), renal support (4.6%), major adverse event (4.3%), post-surgical infection (2.8%), and necrotising enterocolitis (2.4%).
Missing data
Nine patients discharged from hospital alive lacked 30-day life status information, and a further seven patients had missing 6-month life status information. Seven patients had missing length of hospital stay data. Four patients had missing surgery urgency data, and nine patients had missing weight information. All other variables were complete.
Criteria by which acute neurological event was initially diagnosed
There were missing acute neurological event details in four patients. The criteria by which acute neurological event was diagnosed were clinical features in 26/62 including seizures and abnormal movements in 14/62, abnormal electroencephalogram in 23/62, abnormal CT scan in 29/62, abnormal MRI in 24/62. In addition to this, 26 were treated with anticonvulsants. None of the patients in our study met the criteria for brain death. Of the 66 children with acute neurological event, 18 patients had 1 of these features, 19 had 2, 18 had 3, 2 had 4, 3 had 5, and 2 had 6. Of note, cranial ultrasound findings were not in our dataset, although this modality is widely used in the UK.
Association of acute neurological event with other morbidities
There were only 14 (0.5%) acute neurological events that occurred as an isolated complication (Fig. 1) and 52 (1.6%) occurred with multiple complications (18 patients had two, 13 had three, 11 had 4, 7 had 5 and 3 had 6 complications).
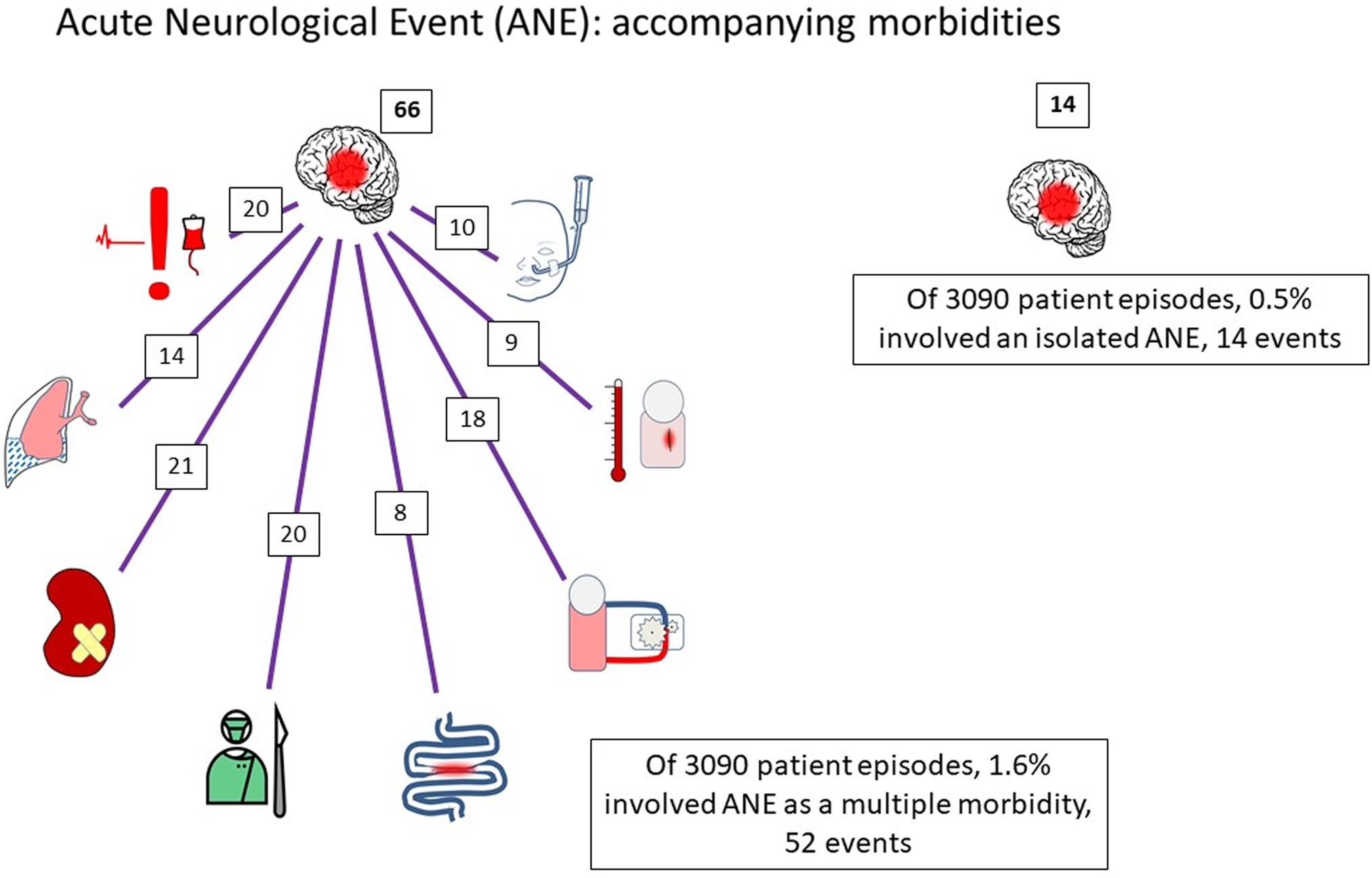
Figure 1. There were only 14 of 66 (0.5%) ANE that occurred as an isolated morbidity and 52 (1.6%) occurred as part of a multiple morbidity. The figure shows the co-occurrence of ANE with ECLS in 18, major adverse event in 20, feeding problems in 10, necrotising enterocolitis in 8, renal support in 21, prolonged pleural effusion in 14, surgical site infection in 9, and unplanned re-operation in 20.
Acute neurological event patient features
The features of patients by presence of acute neurological events are shown in Table 1, and here we focus on the most obvious differences between the two groups. Acute neurological event patients were younger than non-event patients with many more in the neonatal age category (39% versus 16.3%, p < 0.001). Congenital heart conditions were more complex in acute neurological event patients, with a higher proportion having the most severe diagnosis category A (16.7% versus 8.8%, p < 0.001). Acute neurological event patients were more likely to be critically ill prior to surgery: 18 (27.3%) versus 356 (11.8%) of the non-event patients (p < 0.001). Longer cardiopulmonary bypass times were seen in patients who developed acute neurological events with 71.1% having bypass > 90 minutes versus only 41.4% in those without acute neurological events. Of acute neurological event patients, 21 (31.8%) had elective procedures, 37 (56.1%) urgent, 8 (12.1%) emergency or salvage whereas non-event patients were more likely to be elective 2046 (67.7%) with only 897 (29.7%) urgent and 77 (2.6%) emergency or salvage procedures (p < 0.001).
Table 1. Demographic, diagnostic, and surgical variables related to case mix by occurrence of acute neurological event.
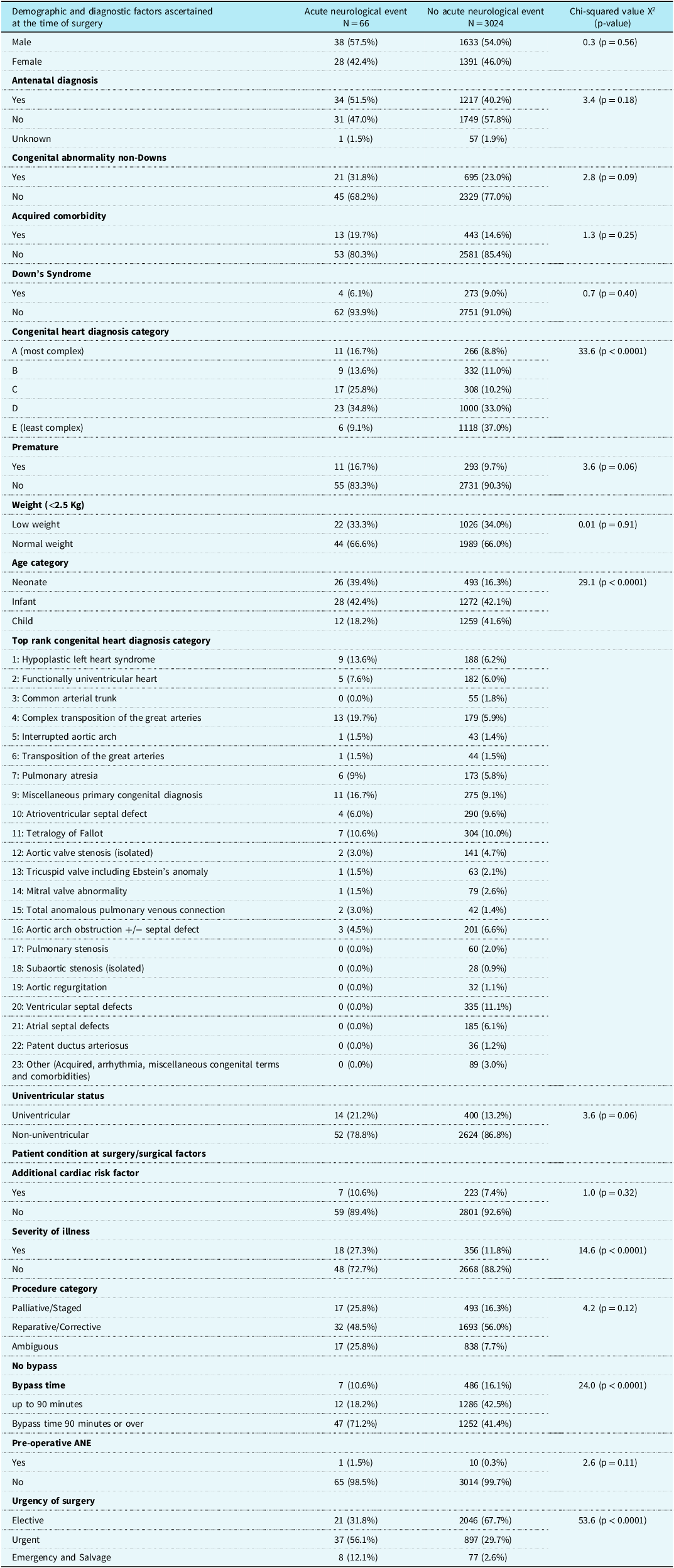
Missing weight information for nine non-acute neurological event patients (N = 3015), missing urgency information for four non-acute neurological events patients (N = 3020).
Risk factor analysis
Univariate analysis
All of our selected risk variables were associated with the complication outcome of acute neurological event on univariate analysis (See Table 2). Neonatal age increased the risk of acute neurological event compared to older ages, with OR 3.3 (95% CI 2.0–5.4) p < 0.0001. The more complex CHD categories of A to C were linked to higher risk of acute neurological event compared to the less complex CHD categories (D and E), with OR 3.0 (95% CI 1.8–4.9) p < 0.0001. Critical illness at the time of surgery (compared to none) was associated with an increased risk of acute neurological event with OR 2.8 (95% CI 1.6–4.9) p < 0.0001. A cardiopulmonary bypass time over 90 minutes compared to shorter or no bypass was linked to increased risk of acute neurological event, with OR 3.5 (95% CI 2.0–6.0) p < 0.0001 and having urgent / non-elective surgery also increased risk of acute neurological event compared with elective surgery OR 4.5 (95% CI 2.7–7.6) p < 0.0001.
Table 2. Univariate and multivariable risk factor analysis in relation to the occurrence of acute neurological event.
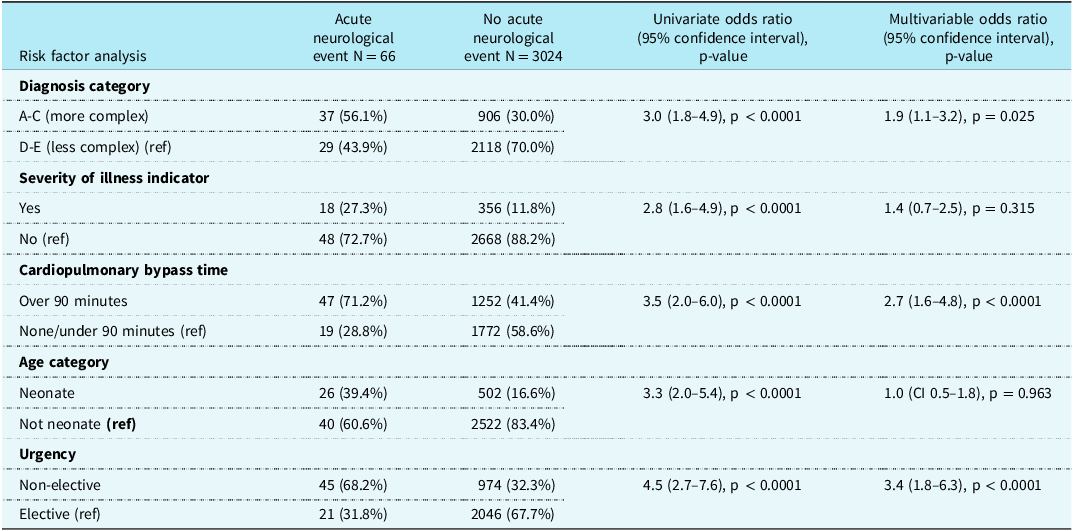
Missing urgency information for four non-acute neurological event patients (N = 3020).
Multiple risk factor analysis
Upon multivariable analysis (See Table 2), after adjustment for other variables, neonatal (compared to older) age (OR 1.0, 95% CI 0.5–1.8, p = 0.963) and critical illness at surgery (OR 1.4, 95% CI 0.7–2.5, p = 0.315) became less important with statistically insignificant results. However, adjusted for other variables in the model, urgent compared to elective surgery (OR 3.4, 95% CI 1.8–6.3, p < 0.0001) and bypass over 90 minutes compared to shorter or no bypass (OR 2.7, 95% CI 1.6–4.8, p < 0.0001) remained very strongly linked to the risk of acute neurological event, and the more complex CHD categories of A-C remained at somewhat higher risk of acute neurological event than less complex conditions (OR 1.9, 95% CI 1.1–3.2, p = 0.025)
Secondary outcomes
Acute neurological event patients had significantly poorer 6-month survival than non-event patients (74.2% versus 97.4%), which equates to an unadjusted odds ratio of 13.0, (95% CI 7.2–23.8, p < 0.001) for acute neurological event. The length of stay for acute neurological event patients was significantly higher than non-event patients (median 35 [IQR 19,44]) days versus 9 (IQR [6,18] days) (p < 0.001).
Discussion
Summary of findings
We used a prospectively collected multi-centre dataset related to 3090 consecutive cardiac operations, and found 66 acute neurological events, providing an incidence rate of 2.1%. Only 14 acute neurological events were isolated post-operative complications, whereas the majority, 52, occurred alongside other types of complication, indicating a very challenging post-operative course. We found that children with acute neurological events were initially detected based on a range of methods (brain scan, electroencephalogram, and clinical assessment), often involving more than one of these at the point of diagnosis. This reflects the complex nature of acute neurological events, which may be clinically challenging to identify in critically ill children, requiring a range of diagnostic tools. Consideration of case complexity for interpretation of our findings was limited given the need to collapse variables (e.g. congenital heart diagnosis), into very broad categories because of small numbers of acute neurological event. Nonetheless, we were interested to note that the most important variables in our multiple risk factor analysis were surgical factors of longer cardiopulmonary bypass time and urgency of the operation. Given our study focuses on the prospective evaluation of post-operative acute neurological event, the specific flagging up of surgical risk factors as most important has face validity. Our study supports the inclusion of acute neurological event as a post-operative metric for paediatric cardiac surgery.
Results in context
There are relatively few studies that specifically explore post-operative acute neurological event as an entity, in part because there are so many other factors implicated in determining neurodevelopmental outcome for children with CHD. Reference Mebius, Kooi, Bilardo and Bos1,Reference Snookes, Gunn and Eldridge13,Reference Sterken, Lemiere, Vanhorebeek, Van den Berghe and Mesotten14,Reference Brunetti, Gaynor and Retzloff26,Reference Ortinau, Smyser and Arthur27 In animal cardiopulmonary bypass models, brain injury was demonstrated with cardiopulmonary bypass-associated hypoxic/ischemic effects on oligodendrocyte precursor cells, and these impacts were worsened by preceding hypoxaemia as compared to normal oxygen levels. Reference Agematsu, Korotcova, Scafidi, Gallo, Jonas and Ishibashi28,Reference Ishibashi, Scafidi and Murata29 These observations are in line with our observational findings in children after paediatric cardiac surgery given the strongest risk factors that we found were urgent heart surgery/longer bypass times. Furthermore, the findings of the Boston Circulatory Arrest Trial demonstrated that prolonged cardiopulmonary bypass times are linked to increased incidence of seizures and additional abnormalities in motor and speech function, as well as cognitive abilities supporting our findings and potentially indicating future sequelae of our patient group. Reference Goldberg, Bove and Devaney30–Reference Gaynor, Nicolson and Jarvik35 In addition to the length of bypass time, the optimal bypass strategy in this patient group is an area of interest when considering measures to reduce post-operative complications. Tadphale et al, identified reduced rates of acute kidney injury with a higher cardiopulmonary bypass flow rate, higher haematocrit target on bypass, higher terminal haematocrit and no reduction in flow rate during hypothermia. Reference Tadphale, Ramakrishnan and Spentzas36 A further study explored the relationship between this bypass strategy and neurological events, but did not find a link perhaps because of the low event rate (0.8%). Reference Chakraborty, Ramakrishnan and Buyukgoz37
The high proportion of children who had acute neurological events that also had other post-operative complications linked to low cardiac output syndrome (e.g. the need for extracorporeal life support and renal support, cardiac arrest, and necrotising enterocolitis) might imply that in some cases, low cardiac output syndrome could be on the causal pathway. This would be supported by data from the single ventricle reconstruction trial, which found that children who had low cardiac output syndrome associated events (extracorporeal life support and cardiac arrest) had worse neurodevelopmental outcomes after adjustment for other factors. Reference Newburger, Sleeper and Bellinger38 A single centre study that reported electroencephalography amongst children who had extracorporeal life support reported that seizures were more common with low cardiac output syndrome. Reference Lin, Banwell and Berg39 Low cardiac output syndrome is more likely with a poorer technical result from surgery and poorer technical results are also linked to worse neurodevelopmental outcome. Reference Nathan, Karamichalis and Liu40,Reference Karamichalis, Barach, Nathan, Henaine, del Nido and Bacha41 Our dataset also demonstrated a 0.45% incidence of post-operative seizures which may be a significant marker for future neurodevelopment of these patients due to established links with poorer developmental outcomes. Reference Goldberg, Bove and Devaney30–Reference Gaynor, Nicolson and Jarvik35,Reference Gaynor, Jarvik and Bernbaum42–Reference Marino, Lipkin and Newburger49 Strokes were observed in small proportion of our patients but is another key predictor of subsequent poor neurodevelopmental and reduced quality of life. Reference Chen, Zimmerman and Jarvik52–Reference Chung, Guilliams and Wilson54
Limitations
Assessment of the brain amongst children requiring cardiac surgery is most challenging in the youngest and sickest children since over and above the inherent difficulties in assessing very young children, they may be sedated and ventilated. In the setting of an imminent urgent cardiac operation, patient evaluation can take advantage of cerebral imaging and electroencephalogram, but none of these modalities is perfect. Reference Brown, Agrawal and Kirschen55 Whilst we prospectively focussed on these assessment challenges, both pre- and post-operative evaluations are not standardised in the UK, hence the assessment will have been imperfect and could have confounded both the pre- and the post-operative evaluation. All participating teams used a dedicated research nurse and physician to assess children prospectively based on the same definition of acute neurological event; however, there was no prospective screening with either electroencephalogram or cross-sectional imaging in all children, in line with routine practice in the UK.
The rarity of acute neurological events and the small number of events in our study mean that the case-mix variables we considered were very broad, which is a particular barrier when trying to understand the inter-relationship between case complexity, the duration of an operation and the occurrence of acute neurological event. We note that children with more complex heart disease require more complex operations, which may require longer periods of cardiopulmonary bypass, and amongst the surgeries that had higher rates of acute neurological event, operations required at neonatal ages dominated. Neonatal operations with an above average rate of acute neurological events in our cohort included: arterial switch 5/85 (6%), complex arterial switch 2/12 (15%), Norwood operation 5/73 (7%), systemic to pulmonary arterial shunt 4/50 (8%), repair of TAPVC 3/43 (7%), and these mixed age operations featured, Rastelli 1/10 (10%), repair of pulmonary atresia 1/18 (6%), repair of anomalous coronary artery from the pulmonary artery 2/14 (14%), and repair of Cor triatriatum 1/10 (10%). The link between acute neurological events and the secondary outcomes of mortality and length of stay will have been influenced by case mix and also by the co-occurrence of other morbidities in 52 of 66 children affected.
Future directions
Our study supports the use of acute neurological event as a post-operative metric for paediatric cardiac surgery and we note that this metric is captured in the Society of Thoracic Surgery and the Paediatric Cardiac Critical Care Consortium (PC4). The definition and evaluation of patients for possible acute neurological events need to be carried out with utmost care and consistency. Additional monitoring methods such as routine use of electroencephalogram Reference McDevitt, Gul, Jones, Scholefield, Seri and Drury56 might improve capture of events. Capture of in-hospital data on acute neurological events may contribute to wider efforts to study neurodevelopment in children with heart disease, including crucially, long-term clinical evaluation.
Conclusions
The study of neurological function and detection of acute neurological event is extremely challenging in the context of paediatric cardiac surgery. Further work is required in order to ensure that this important metric is adequately captured. Prospective monitoring for acute neurological events will be helpful to future quality improvement initiatives in paediatric cardiac surgery.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1047951124000167.
Acknowledgements
We acknowledge with thanks the study data collection at Great Ormond Street Hospital NHS Foundation Trust, Great Ormond Street, London; Evelina London Children’s Hospital, London; Birmingham Children’s Hospital, Birmingham; Bristol Royal Children’s Hospital, Bristol; and Royal Hospital for Children, Glasgow; and we thank the contributing methodologists from Clinical Operational Research Unit, University College London, London.
Financial support
This project was funded by the National Institute for Health Research, Health Services and Delivery Research Program (Project No: 12/5005/06). K. Brown, D. Ridout, and V. Tsang were supported by the National Institute for Health Research Biomedical Research Centre at Great Ormond Street Hospital for Children NHS Foundation Trust and University College London.
Competing interests
None.
Ethical standards
The study has ethical approval from London City Road Research Ethics Committee (14-LO-1442). The views expressed are those of the authors and not necessarily those of the National Health Service, National Institute for Health Research, or Department of Health.






