In patients with CHD requiring right ventricle to pulmonary artery conduit placement, common complications include right ventricular outflow obstruction as well as pulmonary regurgitation. Chronic stenosis, regurgitation, or a combination of the two can lead to right ventricular dysfunction due to the pressure and volume load. Reference Carvalho, Shinebourne and Busst1,Reference Williams, Quaegebeur and Kirklin2 The haemodynamic effects on the right ventricle can lead to diminished functional capacity, left ventricular dysfunction, as well as arrhythmias. Reference Davlouros, Kilner and Hornung3 Reference Valente, Gauvreau and Assenza–5
Transcatheter pulmonary valve replacement for pulmonary regurgitation and pulmonary stenosis offers a successful alternative to surgical replacement of right ventricle to pulmonary artery conduit. Reference Gillespie, Rome and Levi6,Reference Zahn, Hellenbrand and Lock7 Similar to surgical replacement, transcatheter pulmonary valve replacement improves biventricular function and exercise intolerance, while having the additional benefits of avoiding sternotomies and cardiopulmonary bypass. In addition, recent studies have shown biventricular functional improvement and remodelling both in the early stages as well as at mid-term follow-up. Reference Lunze, Hasan and Gauvreau8–Reference Frigiola, Tsang and Bull12
Guidelines for surgical pulmonary valve replacement in patients with post-operative pulmonary regurgitation are generally based on right ventricular volumes assessed by cardiac MRI. Reference Tretter, Friedberg and Wald13–Reference Valente, Cook and Festa16 Indications for transcatheter pulmonary valve replacement have historically followed the indications for surgical pulmonary valve replacement. Reference Tretter, Friedberg and Wald13 Indexed right ventricular end diastolic volumes > 150 ml/m2 by MRI is one of the factors considered when determining eligibility for transcatheter pulmonary valve replacement. Reference Tretter, Friedberg and Wald13 An elevated right ventricular annular tilt of > 20° has been associated with elevated right ventricular end diastolic volumes > 150 ml/m2 by MRI, compared to right ventricular annular tilts that range from 0.1 ± 9.4° in children with structurally and functionally normal hearts. Reference Punn, Behzadian and Tacy17 The acute and long-term effects of transcatheter pulmonary valve replacement on right ventricular annular tilt have not been assessed. This technique would be clinically useful if echocardiographic measures of right ventricular enlargement and dysfunction could be used to evaluate improvement post transcatheter pulmonary valve replacement, particularly in young patients. The purpose of this study was to evaluate the effect on right ventricular annular tilt in the immediate and mid-term follow-up periods, with the hypothesis that right ventricular annular tilt would continue to improve over time and serve as a marker of right ventricular global health. A secondary purpose was to investigate other measures of ventricular performance during the same time course.
Methods
Study subjects and design
We retrospectively collected all patients who underwent transcatheter pulmonary valve replacement at Lucile Packard Children’s Hospital at Stanford between January 1, 2011 and January 1, 2017. We included patients with pre- and post-procedural echocardiograms. All pre-procedural echocardiograms were done within 3 months of the transcatheter pulmonary valve replacement, with 75% of the echocardiograms done within the 7 days of the procedure. Pre-intervention echocardiograms were retrospectively compared to immediate post-procedure echocardiograms, as well as to mid-term follow-up (defined as > 1 year and < 2 years after intervention) evaluations. Adults (greater than 18 years of age) and children participated in this study. The indication for transcatheter pulmonary valve replacement was determined to establish subcategories of the entire cohort.
Catheterisation
Patients underwent cardiac catheterisation under general anaesthesia for transcatheter pulmonary valve replacement. Baseline values for right ventricular pressure, peak gradient across the conduit, and mean right atrial pressures were obtained before and after transcatheter pulmonary valve replacement. Melody transcatheter pulmonary valves (Medtronic Inc., Minneapolis, Minnesota) or Sapien transcatheter pulmonary valves (Edwards Lifesciences LLC., Irvine, California) were used in all patients. Test occlusion was performed, to ensure no coronary artery encroachment with subsequent device deployment based on size.
Echocardiography
We obtained echocardiograms using commercially available equipment, including the Philips iE33 (Philips Medical Systems, Bothell, WA), Philips Epiq (Philips Medical Systems, Bothell, WA), or the Acuson C512 (Siemens Medical Solutions USA, Mountain View, CA). Offline independent measurements were done using the syngoDynamics workstation (Siemens Medical Solutions USA; syngoDynamics Solutions, Ann Arbor, MI) and followed standard recommendations for image acquisition as recommended by the American Society of Echocardiography. Images were stored in a DICOM format for measurements and for offline speckle-tracking strain analysis by Siemens Velocity Vector Imaging version 3.0.1.15 deformation analysis software (Siemens Medical Solutions USA, Mountain View, CA).
Continuous wave Doppler was used to assess degree of pulmonary stenosis across the right ventricle to pulmonary artery conduit. Degree of pulmonary regurgitation was graded according to the American Society of Echocardiography’s Nomenclature and Standards Committee and the Task Force on Valvular Regurgitation Reference Zoghbi, Enriquez-Sarano and Foster18 and was recorded from the official pre-catheterisation echocardiogram report. Pulsed-wave Doppler was used to evaluate mitral valve inflow E and A waves to calculate the E/A ratio. Tissue Doppler velocities were also used to obtain peak S,’ E,’ and A’ waves. Reference Sluysmans and Colan19,Reference Colan, Parness and Spevak20
Functional measurements of the right and left ventricles were also completed. The right ventricular end-diastolic area and end-systolic area were measured and a fractional area change was calculated. In order the evaluate left ventricular function, left ventricular ejection fraction was calculated using end-diastolic and end-systolic volumes derived from the 5/6 area x length method. Reference Sluysmans and Colan19,Reference Lopez, Colan and Frommelt21–Reference Lang, Badano and Mor-Avi23
The highest quality apical four-chamber view images were identified to perform right ventricular annular tilt measurements and strain measurements (Fig. 1A). Right ventricular annular tilt was determined by measuring the angle of the tricuspid valve plane relative to the mitral valve plane at end-diastole in the apical four-chamber view. Reference Punn, Behzadian and Tacy17 Right ventricular systolic strain measurements were used to assess strain along each right ventricular segment after a user-defined tracing along the endocardial borders (Fig. 1B). These manual tracings were done in the apical four chamber view and were adjusted by the user to ensure adequate endocardial tracking. Deformation measurements were obtained from the pre-intervention, immediately post-intervention, and mid-term post-intervention echocardiograms when available. Images were excluded if the endocardial borders were not visible. All measurements were done by a single physician, blinded to patient and timing of study.

Figure 1. A. apical four chamber view of a study patient with the right ventricular annular tilt technique described in Punn, et al. a line is drawn through the mitral valve hinge points (white). a second line is drawn from the tricuspid valve free wall hinge point to the interventricular septum (yellow). the bisecting angle (), is the right ventricular annular tilt. Figure 1B. apical four chamber view of a study patient with right ventricular global strain tracing on the siemens velocity vector imaging version 3.0.1.15 deformation analysis software (Siemens medical solutions USA).
Statistics
All data are expressed as a mean with standard deviation, or median with range as appropriate. Pre- and immediate post-intervention right ventricular function and strain data were compared with paired t-tests, as well as pre versus mid-term, and immediate post versus mid-term. A subanalysis was completed after stratifying the patients based on primary indication for transcatheter pulmonary valve replacement, namely pulmonary stenosis, regurgitation, or mixed presentation. The statistics package of SAS EG 7.2 (SAS Institute, Cary, NC) was used for statistical analysis. P values ≤ 0.05 were considered to indicate statistical significance.
Results
Study subjects
Seventy patients met diagnostic criteria for inclusion constituted the study cohort (median age 13.2 years; range, 3.1–48.1 years); the group with a primary indication for transcatheter pulmonary valve replacement of pulmonary stenosis included 12 patients, pulmonary regurgitation included 21 patients (Table 1). Thirty-two patients had neither criterion, meaning regurgitation and stenosis were less than severe. Sixty-four patients (91%) underwent transcatheter pulmonary valve replacement with a Melody valve; the remainder received a Sapien valve.
Table 1. Patient demographics (n = 70).

Data are expressed as median (range) or number (percentage).
Outcomes in the entire cohort
Table 2 illustrates the significant differences between measures of right ventricular function before and after transcatheter pulmonary valve replacement. There is an abrupt decrease in right ventricular annular tilt suggestive of decreased volume load on the right ventricle. This change remains significant when comparing the immediate post- transcatheter pulmonary valve replacement group and the mid-term group, indicating a continued improvement. Similarly, the tricuspid valve Z-score also decreases immediately post-transcatheter pulmonary valve replacement though it is not maintained into the mid-term follow-up cohort.
Fractional area change measured normally in the pre- transcatheter pulmonary valve replacement group and remains unchanged both immediately and in the mid-term follow-up period after transcatheter pulmonary valve replacement. In comparison, the left ventricular ejection fraction has an immediate statistically significant increase after transcatheter pulmonary valve replacement, though clinically, the function only increases by 2–3%. This change also appears to be transient as the left ventricular ejection fraction at the mid-term follow-up is similar to the pre-intervention state. Interestingly, global strain is not different between the pre- and immediately post-transcatheter pulmonary valve replacement groups; however, there is a statistical improvement between the pre- and mid-term groups. Tricuspid annular plane systolic excursion Z-score, as an additional measure of right ventricular function was abnormal in the pre, immediately-post, and mid-term-post groups with no significant improvement longitudinally. The S’ wave increase immediately post-intervention neared significance (P = 0.057), but there did not appear to be continued change into the mid-term follow-up period.
Table 2. Comparison of right ventricular function before and after TPVR in the entire cohort.
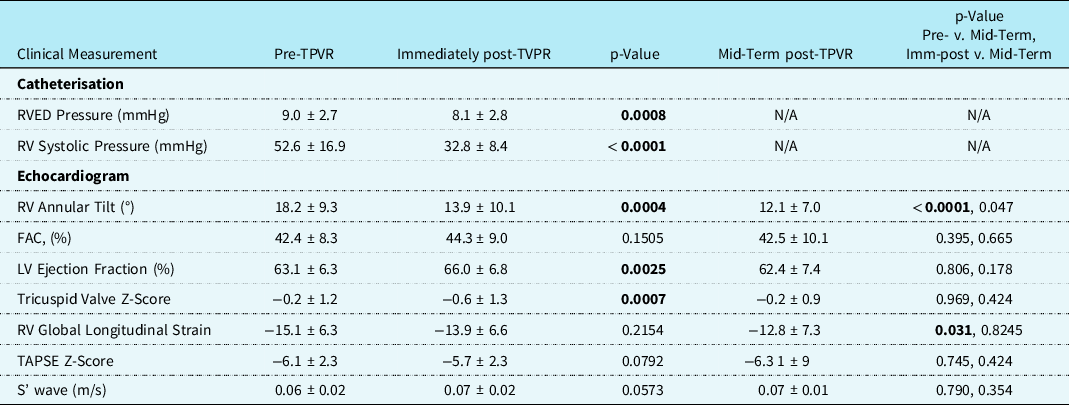
FAC = fractional area change; LV = left ventricle; N/A = not applicable; RV = right ventricle; RVED = right ventricular end diastolic; TAPSE = tricuspid valve annular plane systolic excursion; TPVR = transcatheter pulmonary valve replacement.
Data are expressed as mean ± SD, P-value is bolded if significant.
Comparison between Adults and Children after transcatheter pulmonary valve replacement
The smaller subset of adult patients undergoing transcatheter pulmonary valve replacement were compared to the paediatric patients before and after transcatheter pulmonary valve replacement. These findings are shown in Tables 3 and 4. There were no significant differences between children and adults in the measures of right ventricular size and function prior to transcatheter pulmonary valve replacement. Immediately post-transcatheter pulmonary valve replacement, both adults and children show a significant difference in the right ventricular annular tilt. The gross values of the right ventricular annular tilt are significantly higher in children. The gross values post-intervention are significantly lower in adults, consistent with a more drastic change after transcatheter pulmonary valve replacement. Children also appeared to show a trend towards a decrease in the right ventricular annular tilt at mid-term follow-up, compared to the adults. However, the immediate post-intervention gross right ventricular annular tilt value was already quite low in the adult population, and there was only a small pool of mid-term follow-up patients.
Table 3. Comparison of right ventricular function in children and adults before and after TPVR.

FAC = fractional area change; LV = left ventricle; N/A = not applicable; RV = right ventricle; RVED = right ventricular end diastolic; TAPSE = tricuspid valve annular plane systolic excursion; TPVR = transcatheter pulmonary valve replacement.
Data are expressed as mean ± SD, P-value is bolded if significant.
Table 4. Comparison of right ventricular function in adults and children before and after TPVR.

RV = right ventricle; TPVR = transcatheter pulmonary valve replacement.
Data are expressed as mean ± SD, P-value is bolded if significant.
Discussion
In this retrospective study, we focussed on right ventricular annular tilt as a marker of right ventricular health in patients after transcatheter pulmonary valve replacement. This study found an abrupt decrease in annular tilt values immediately post intervention, indicating an abrupt decrease in right ventricular size when positioning a competent pulmonary valve. Moreover, the tricuspid valve size decreased and left ventricular ejection fraction increased, presumably from the decrease in right ventricular preload. In addition, we showed that the physiological benefits of decreased right ventricular enlargement were maintained at 1-year post-intervention, since the right ventricular annular tilt, left ventricular ejection fraction, and tricuspid valve Z-score remained similar to the immediate post-intervention values.
Right ventricular enlargement plays an important predictor of morbidity and mortality in patients requiring right ventricular to pulmonary artery conduits. Reference Carvalho, Shinebourne and Busst1 Right ventricular enlargement leads to right ventricular failure, ventricular arrhythmias, and sudden death. Reference Davlouros, Kilner and Hornung3–Reference Valente, Gauvreau and Assenza5 Pulmonary valve replacements have been shown to decrease the progression of right ventricular enlargement, and even have the potential to reduce the enlargement through remodelling. Reference Coats, Khambadkone and Derrick9 Reference Coats, Tsang and Khambadkone–11 Right ventricular annular tilt represents a successful method to recognise increased right ventricular volumes in paediatric patients with tetralogy of Fallot, Reference Punn, Behzadian and Tacy17 but the change in annular tilt pre- and post-transcatheter pulmonary valve replacement or as a progression over time has not been evaluated.
In our study, the indications for pulmonary valve replacement include isolated severe pulmonary stenosis, isolated severe pulmonary regurgitation, both severe stenosis and regurgitation, and a combination of non-severe pulmonary regurgitation and stenosis. Only 12 patients underwent transcatheter pulmonary valve replacement for isolated severe pulmonary stenosis, and as expected, the right ventricular pressure decreases with transcatheter pulmonary valve replacement as noted in the catheterisation data. The rest of the groups all had a component of volume overload due to pulmonary regurgitation. The last group was the most common indication, suggesting that the right ventricle is particularly susceptible to both conditions due to a combined pressure and volume load. The right ventricular annular tilt decreased immediately after intervention, suggesting an extremely effective decrease in right ventricular volume after transcatheter pulmonary valve replacement. This abrupt decrease in volume benefited both adults and children when evaluated separately. The difference between right ventricular annular tilt between the immediately post-transcatheter pulmonary valve replacement group and the mid-term transcatheter pulmonary valve replacement group was nearly significant (P = 0.06) with the mean right ventricular annular tilt in the mid-term follow-up group lower than the immediately-post transcatheter pulmonary valve replacement group. This change may indicate ongoing remodelling, but the sample volume was low for mid-term follow-up.
Other measures associated with increased right ventricular volume, like tricuspid valve size, had similar findings. There was a statistically significant decrease in tricuspid valve size between the pre-intervention and immediate-post transcatheter pulmonary valve replacement group, but no ongoing change between the tricuspid valve Z-score in the immediately-post transcatheter pulmonary valve replacement and mid-term follow-up groups. Notably, the tricuspid valve Z-score was not dilated in the pre-intervention state. Pulmonary valve dysfunction may predominantly contribute to right ventricular body and infundibulum dilation and cause corresponding right ventricular shoulder elevation without as obvious of an impact on tricuspid valve size. Right ventricular annular tilt may therefore be more sensitive to changes in right ventricular volume from pulmonary valve dysfunction than tricuspid valve annular size.
Left ventricular ejection fraction is known to be affected by ventriculo-ventricular interactions. Reference Frigiola, Tsang and Bull12 The left ventricular ejection fraction predictably increased immediately after transcatheter pulmonary valve replacement, but did not increase further by 1 year follow-up. The absolute percentage difference in ejection fraction was notably small and could be due to measurement variability. The lack of difference between left ventricular ejection fraction and tricuspid valve Z-score between the immediate and mid-term follow-up periods may signify that the remodelling is immediate and does not continue, or it may be related to the low number of patients in the mid-term follow-up group.
In order to evaluate other markers of right ventricular performance, we analysed variables that assessed right ventricular function. Prior studies have suggested that fractional area change, tricuspid valve annular plane systolic excursion, tissue Doppler derived velocity, and global strain constitute reasonable methods to estimate right ventricular function. Reference Selly, Iriart and Roubertie24–Reference Brown, McElhinney and Araoz26 Interestingly, there was no significant change in fractional area change between any of the groups, with mean values of all three groups in the normal ranges. Function appears to be relatively preserved in these patients despite the volume and pressure overload. This observation is similar to findings of prior studies looking at both echocardiographic and MRI measures of right ventricular function Reference Lurz, Nordmeyer and Giardini27 pre- and post-transcatheter pulmonary valve replacement.
Tricuspid annular plane systolic excursion Z-scores were stably abnormal in the pre-, immediately-post-, and mid-term groups. Tricuspid valve annular plane systolic excursion measures longitudinal motion of the right ventricular body and has been reported at lower values in patients with tetralogy of Fallot than other forms of non-CHD. Reference Mercer-Rosa, Parnell and Forfia28,Reference Bonnemains, Stos and Vaugrenard29 Moreover, prior studies have demonstrated that tricuspid annular plane systolic excursion may not correlate well with assessment of function in tetralogy of Fallot, Reference Mercer-Rosa, Parnell and Forfia28,Reference Koestenberger, Nagel and Ravekes30 perhaps explaining why the values are abnormal while the fractional area change values are normal throughout the study period. Tricuspid annular S’ velocity similarly measures right ventricular longitudinal motion to assess function. The tricuspid annular S’ velocity significantly increased between pre- and immediately-post transcatheter pulmonary valve replacement. These results suggest that there may be subtle improvements in right ventricular function over time that are at least maintained at 1-year post- transcatheter pulmonary valve replacement.
Global right ventricular strain on two-dimensional echocardiographic images has been shown to correlate to right ventricular ejection fraction by MRI, Reference Lee and Park31 and multiple studies have shown that global longitudinal strain detects subtle decreases in ventricular function that are not appreciated by conventional measures. Reference Adamson, Arunamata and Tacy32–Reference Lowenthal, Tacy and Behzadian34 Our results indicated no difference prior to intervention and immediately after intervention; however, right ventricular stain significantly improved between the pre-intervention group and the mid-term follow-up group. Tricuspid annular plane systolic excursion and S’ wave both utilise the longitudinal motion of the right ventricular shoulder and ignore the apex, Reference Mercer-Rosa, Parnell and Forfia28,Reference Bao, Zhang and Chen35 which may make these measures more susceptible to volumetric changes, thereby resulting in an immediate change post-transcatheter pulmonary valve replacement. In contrast, the improvement in right ventricular global strain at mid-term follow-up rather than immediately post-intervention suggests that right ventricular global strain may be less impacted by sudden volume shifts and instead indicate predictably slower right ventricular remodelling.
Limitations and Future Directions
The retrospective nature of the data limits this current study. There is a lack of prospective studies that confirm and correlate the various echocardiographic measures of right ventricular health to MRI and catheterisation-based assessments. In addition, the adult population only made up a small proportion of our total cohort. Thus, the lack of difference between the adult and paediatric patients may represent a Type I error. Lastly, mid-term follow-up data was challenging to obtain, particularly for the adults, due to many of our patients undergoing procedures at our institution and having their general cardiology maintenance at outside centres. While there was a significant immediate decrease to low right ventricular annular tilt post-intervention, it is unclear whether this change was sustained because it had already reached maximal improvement or whether there was insufficient data to assess ongoing decrease in right ventricular annular tilt. Thus, we need prospective studies with larger sample sizes and longer follow-up that may better illustrate the subtle changes in right ventricular remodelling that occur later.
Conclusions
Right ventricular annular tilt appropriately decreases after successful transcatheter pulmonary valve replacement, indicating a decrease in right ventricular volume. In addition, our findings indicate that right ventricular annular tilt correlates with other findings of right ventricular health both in the immediate and mid-term follow-up groups. Right ventricular annular tilt is feasible to incorporate in to the workflow to assess right ventricular volume and has previously been shown to have low interobserver variability. Reference Punn, Behzadian and Tacy17 Right ventricular annular tilt is a simple method to estimate right ventricular volume and also track changes in right ventricular enlargement over time.
Author contribution
Charitha Reddy: Concept/Design, Data Collection, Data Analysis/Interpretation, Drafting Article, Statistics.
Rumi Yokota: Data Collection, Data Analysis, Approval of Article.
Rajesh Punn: Data Analysis/Interpretation, Statistics, Critical Revision of Article, Statistics, Approval of Article.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Competing interests
None.








