The rapid spread and devastating impact of infectious disease outbreaks, such as COVID-19, highlights the critical importance of effective collaborative outcomes in crisis management. The success of these responses depends on the complex interplay between various factors, including emergency preparedness, support and assurance, task difficulty, organizational command, medical treatment, and epidemic prevention and protection. Additionally, collaboration with societal partners such as civil society organizations and community leaders, as well as active community engagement, are essential to ensure a whole-of-society approach, as emphasized in the WHO Strategic Framework for Emergency Preparedness. 1 Importantly, preparedness alone does not guarantee success; outcomes are shaped by various factors, including behavioral factors, such as public compliance with health directives, and structural enablers, such as policy coordination across health, economic, and social sectors. Emerging evidence suggests that these core factors are interdependent: preparedness and support systems can mutually reinforce each other, while high task difficulty could strain both preparedness capacities and support infrastructure.Reference Choudry, Ayub and Badar 2 –Reference Melaku, Zeynudin and Suleman 4 Understanding the roles of these factors, and their mechanisms, is essential for developing strategies to enhance the effectiveness of management efforts and optimize collaborative outcomes during health crises.
Emergency preparedness constitutes the foundation of an efficient response. The knowledge and capacities developed by governments, response and recovery organizations, communities, and individuals to effectively anticipate, respond to, and recover from the impacts of likely, imminent, or current disasters. 5 Preparedness actions are carried out within the context of disaster risk management, with the goal of building the necessary capacities to efficiently manage all types of emergencies and to ensure a smooth transition from response to sustained recovery 5. It has been examined in various contexts,Reference Williams, Jones and Welch 6 and studies have highlighted the importance of developing robust plans, capacities, material preparations, community-based risk communication, and multisectoral coordination systems, and systems to manage potential outbreaks.Reference Chen, Dandan and Juan 7 –Reference Chua, Cosmas and Arsat 9 Support and assurance mechanisms, including financial and logistics resources, as well as partnerships with civil society organizations and local communities, have also been identified as being critical for the implementation of these responses.Reference Lal, Abdalla and Chattu 10
Organizational command—defined as centralized decision-making structures enabling rapid resource allocation and interagency coordination—serves as the operational backbone of outbreak response. For instance, during the 2014–2016 Ebola epidemic, Liberia’s Incident Management System reduced case fatality rates through real-time data integration and adaptive leadership.Reference Brooks, Pinto and Gill 11 Task difficulty, operationalized as challenges stemming from pathogen virulence, health care system fragility, resource scarcity, and sociopolitical constraints, is often influenced by an infectious agent’s nature and outbreak scale, further shaping the response efforts.Reference Gupta, Purcell and Corti 12 Effective organizational command is vital for coordinating cross-sectoral stakeholders, including government agencies, private sectors, and civil society actors, while medical treatment protocols are critical for providing appropriate care to affected individuals. Finally, epidemic prevention and protection measures, including public health education, the provision of protective equipment, implementation of control measures, community-driven interventions, and establishment of management systems, are indispensable for containing the spread of a disease and safeguarding the population.Reference Kabego, Balde and Barasa 13
The interplay between these factors ultimately influences the collaborative outcomes during major infectious disease outbreaks. This can range from successful disease containment and mitigation to overwhelmed health care systems and increased mortality rates. Recent studies underscore that even robust preparedness systems may fail without complementary societal actions—such as community trust in authorities, citizen adherence to preventive measures (e.g., mask-wearing), and alignment of health policies with socioeconomic priorities.Reference Grant 14 For instance, regions with high levels of preparedness but low public compliance experienced prolonged outbreak durations compared to areas with integrated strategies.Reference Bodas, Peleg and Stolero 15 A whole-of-society approach, integrating community participation and leveraging the strengths of civil society organizations, is critical to address gaps in preparedness and response, as outlined in the WHO framework. Despite the extensive research on these individual factors, their collective impact on and the mechanisms through which they affect collaborative outcomes lack comprehensive understanding. This gap in the literature hinders the ability to develop a holistic understanding of collaborative responses to infectious disease outbreaks and identify strategies for improving collaborative outcomes. To address this gap, a comprehensive approach is required that examines the effects and underlying mechanisms of these factors on collaborative outcomes within a unified framework.
Therefore, this study examines the effects and underlying mechanisms of emergency preparedness, support and assurance, task difficulty, organizational command, medical treatment, and epidemic prevention and protection on the collaborative outcomes among medical personnel during major infectious disease outbreaks. By elucidating these relationships, this study provides valuable insights for policymakers and health care professionals to improve collaborative practices within medical teams, ultimately contributing to more effective preparedness and response strategies for future infectious disease outbreaks.
To address the objective, this study formulated the following hypotheses through a comprehensive literature review:
H1: Emergency preparedness has a significant positive impact on organizational command.
H2: Support and assurance have a significant positive impact on organizational command.
H3: Emergency preparedness has a significant positive impact on medical treatment.
H4: Support and assurance have a significant positive impact on medical treatment.
H5: Emergency preparedness has a significant positive impact on prevention and protection.
H6: Support and assurance have a significant positive impact on prevention and protection.
H7: Organizational command has a significant positive impact on collaborative outcomes.
H8: Medical treatment has a significant positive impact on collaborative outcomes.
H9: Prevention and protection have a significant positive impact on collaborative outcomes.
H10: Emergency preparedness and support and assurance have a significant positive mutual impact.
H11: Task difficulty and emergency preparedness have a significant positive mutual impact.
H12: Task difficulty and support and assurance have a significant positive mutual impact.
The study model, illustrated in Figure 1, is a generalized structural equation model (SEM) that conceptualizes the relationships among key variables based on hypotheses derived from the literature. The model integrates emergency preparedness, support and assurance, task difficulty, organizational command, medical treatment, prevention and protection, and collaborative outcomes. It reflects a synthesis of existing theoretical frameworks and empirical studies on emergency preparedness and collaborative outcomes in the context of infectious disease outbreaks. The model serves as the foundation for testing the hypothesized relationships and provides a visual representation of the pathways through which these factors influence collaborative outcomes among medical personnel.
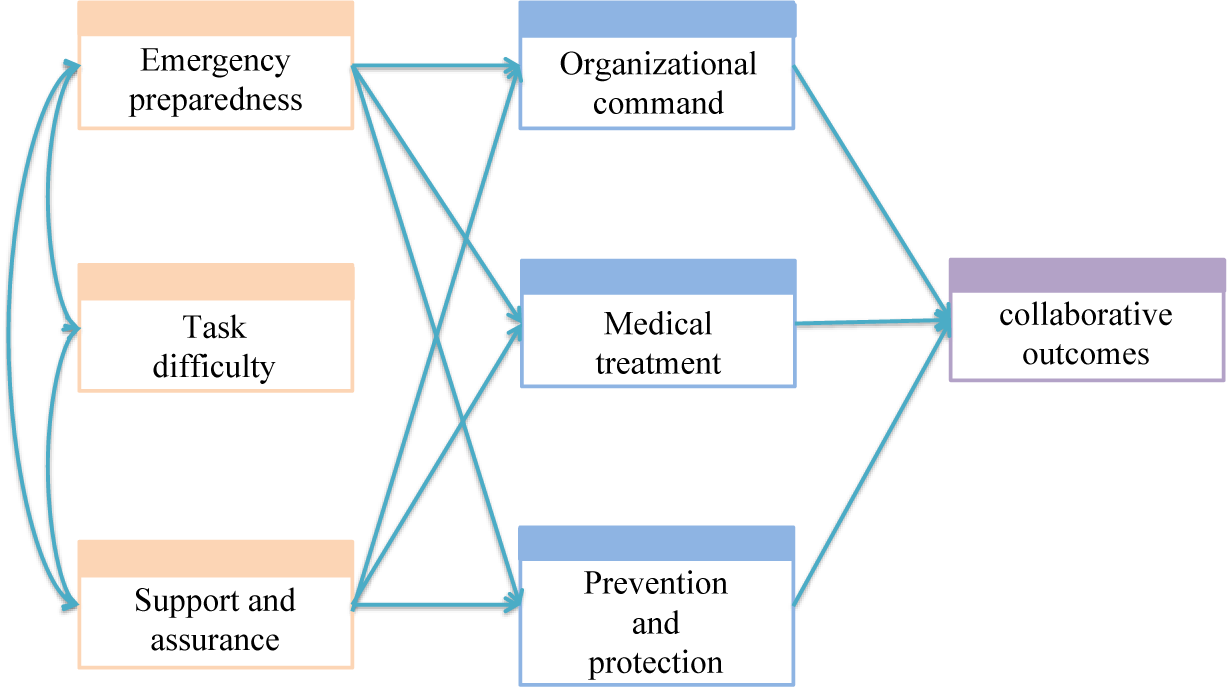
Figure 1. Generalized structural equation model.
This figure illustrates the conceptual model developed for this study, which integrates key variables and their hypothesized relationships. The model is based on a synthesis of existing literature and theoretical frameworks related to emergency preparedness and collaborative outcomes in health care settings. The arrows represent the hypothesized causal pathways, with emergency preparedness, support and assurance, and task difficulty as exogenous variables influencing organizational command, medical treatment, and prevention and protection. These, in turn, are hypothesized to directly impact collaborative outcomes. The model also includes mutual relationships between emergency preparedness, support and assurance, and task difficulty. The SEM framework allows for the simultaneous testing of these relationships, providing a comprehensive understanding of the factors that drive collaborative outcomes among medical personnel during infectious disease outbreaks.
Methods
Questionnaire and Measure
To investigate the key factors’ collective influence on the management of major infectious disease outbreaks, this study designed an online questionnaire that encompassed 8 sections: general information, emergency preparedness, task difficulty, organizational command, medical treatment, epidemic prevention and protection, support and assurance, and collaborative outcomes. All items were rated on a 5-point Likert scale. The questionnaire development was grounded in an extensive review of WHO emergency response frameworks and validated crisis management scales. 1 Through 3 rounds of expert consultation with 15 public health specialists and emergency responders, we established content validity. The instrument encompasses 7 domains that measure critical dimensions of outbreak response. Notably, the “Support and Assurance” section assessed material and systemic backstops through 6 dimensions: physical infrastructure adequacy, pharmaceutical reserves, diagnostic capacity, logistics chain integrity, funding security, and communication systems reliability. The “Task Difficulty” construct evaluated outbreak complexity through 10 validated challenge indicators from the WHO Health Emergency Dashboard, including pathogen virulence, transmission dynamics, antigenic variation frequency, resource scarcity index of the affected region, health care system surge capacity, socio-psychological resilience factors, team coordination coherence, patient adherence metrics, response time window, and technical complexity index.
Sampling and Data Collection
Questionnaires were distributed using an online survey platform. Participants were recruited through WeChat, a widely used social media platform, with recruitment expanded to hospital intranet portals and professional medical associations to diversify the sample pool and reduce geographic bias. Recruitment messages were posted in WeChat groups, “Moments,” and through direct messages to potential participants. The messages contained information about the study, including the purpose, procedures, inclusion criteria, and the voluntary nature of participation. The WeChat recruitment strategy was complemented by snowball sampling; participants were encouraged to share the recruitment message with their contacts who might be eligible for the study. The survey was open for a period of September 14-October 23, 2023. Most of the participants were from Shanghai, Suzhou and Fuzhou. The eligibility for survey participation was contingent on the following criteria: (1) current employment within a hospital setting; (2) direct involvement in the management and response to major infectious disease outbreaks; and (3) able to participate in and complete the questionnaire and provide informed consent. Individuals not employed in the medical profession were excluded. A total of 967 questionnaires were distributed, of which 779 met the inclusion criteria (response rate: 80.56%). Missing data were addressed via listwise deletion after confirming that the missingness was completely at random.
Statistical Analysis
SPSS software was used to perform the statistical analysis. Descriptive statistics were used to summarize the participants’ demographic characteristics, and Cronbach’s α was used to assess the data reliability. The scale’s discriminant validity was assessed using the square root of the average variance extracted (AVE), and its structural validity was assessed using factor loading. An exploratory factor analysis (EFA) was performed to identify the number of factors influencing the observed variables and determine the degree of correlation between each factor and the corresponding variables.
Subsequent to the reliability and validity assessments, this study conducted structural equation modeling (SEM) using AMOS 24.0 to analyze the complex relationships between the variables. Initial model modifications involved adding covariance paths between measurement errors of items with modification indices >10.0, strictly guided by theoretical relevance. This study assessed the SEM model’s fit using the chi-square test per degree of freedom (χ2/df), goodness-of-fit index (GFI), adjusted goodness-of-fit index (AGFI), and root mean square error of approximation (RMSEA). These indices collectively provided insights regarding the model’s fit with the observed data. This study undertook any necessary model modification to enhance the fit, as guided by theoretical considerations and statistical feedback.
Within the SEM, this study employed a path analysis to quantify the direct and indirect effects of the latent variables on each other, thereby identifying the pivotal factors influencing the collaborative outcomes during health crises. This analytical approach allowed for a nuanced examination of the relationships between emergency preparedness, organizational command, medical treatment, task difficulty, epidemic prevention and protection, and support and assurance, and their impact on collaboration outcome effectiveness.
Ethics Approval and Consent to Participate
The Committee on Ethics of Medicine, Navy Medical University, PLA, approved this study. All participants were informed of the study aims and provided informed consent electronically.
Results
Demographic Characteristics
A total of 779 health care professionals participated in this study. Most participants were women (78.8%) with an average age of 33.92 years (33.92 ± 7.37, aged 21-30 years: 39.54%; 31-40 years: 42.75%; and >40 years: 17.71%). Most participants held a bachelor’s degree or higher (86.6%) and an intermediate or higher professional title (58.4%). The participants comprised clinicians (29.1%) and nurses (70.9%). Overall, 20.9% had participated in pandemic response tasks in Hubei and Shanghai, while 79.1% had participated in local pandemic-related tasks. Finally, 65.9% of the participants had no previous experience in dealing with infectious disease outbreaks before the COVID-19 pandemic (Table 1). This aligns with our inclusion criteria, which required participants to have direct involvement in the COVID-19 response but did not exclude those lacking pre-pandemic outbreak experience.
Table 1. Participants’ demographic characteristics
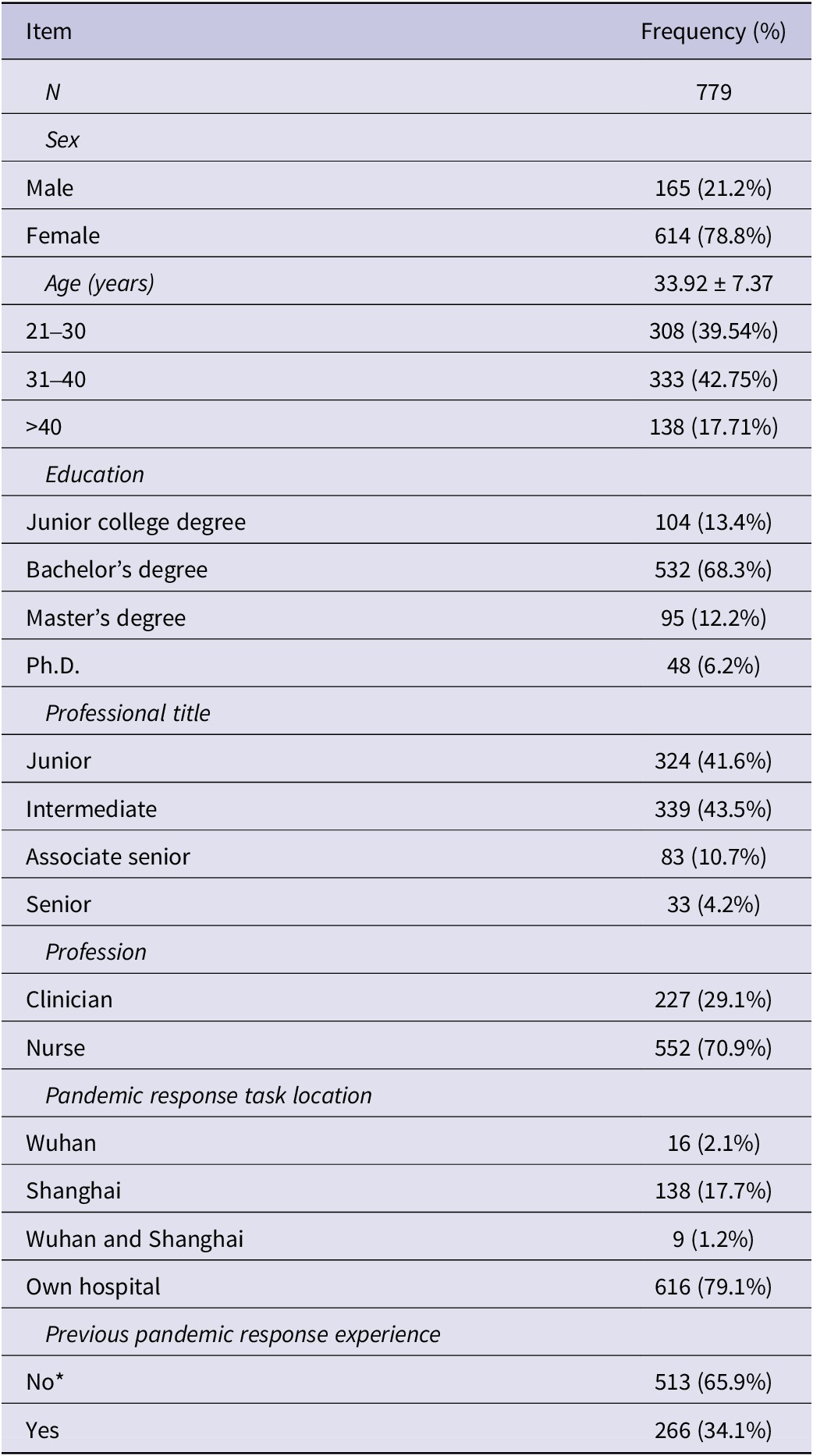
Note: *“No previous pandemic response experience” refers to lack of involvement in managing major infectious disease outbreaks before the COVID-19 pandemic.
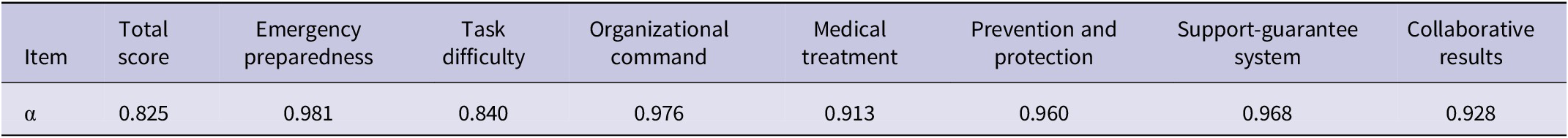
Reliability and Validity Assessment
This study used Cronbach’s α to assess data reliability, reflecting the degree of consistency and stability. An α coefficient value closer to 1 indicates greater reliability; an α coefficient value of 0.7 or higher indicates high internal consistency and reliability. The overall α coefficient value for the sample was 0.825, indicating high reliability (Table 2). The α coefficients for each dimension ranged from 0.840-0.981, with all factors exceeding 0.7. Thus, the scale items demonstrated good internal consistency and high reliability for each factor.
Table 2. Cronbach’s α coefficient values for the scale and its dimensions
The factor analysis revealed strong construct validity across most items, with factor loadings exceeding 0.70 for 32 of 47 indicators, indicating robust alignment with their respective latent variables. Items X8-X13 (emergency preparedness) and X38-X47 (prevention and protection) demonstrated exceptional factor loadings (λ = 0.821-0.933) and high agreement (mean = 4.36-4.57, SD < 0.73), confirming their centrality to the constructs. Organizational command items (X24-X37) showed moderate-to-high loadings (λ = 0.685-0.895), though with slightly greater variability (SD = 0.66-0.84). Key observed indicators included pre-employment training (Item X38: λ = 0.821, M = 4.41, SD = 0.664) and PPE quality/distribution (Item X39: λ = 0.851, M = 4.36, SD = 0.709) (Table S1).
Discriminant Validity
The discriminant validity analysis results revealed that the correlation coefficients between each factor and the other factors were less than the square root of the AVE (Table 3); thus, the scale had good discriminant validity. Emergency preparedness, organizational command, medical treatment, epidemic prevention and protection, support and assurance, and collaborative effectiveness were all positively correlated with each other. However, the relationships between these factors and task difficulty were not significant. The factor loadings of the scale were within the standard range of 0.5-0.95, indicating good construct validity.
Table 3. Correlation coefficient matrix
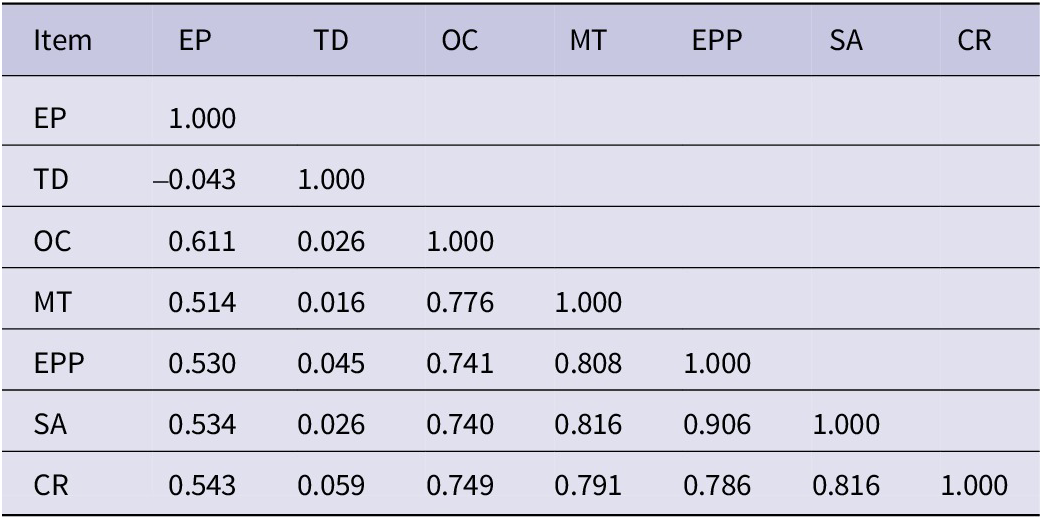
Abbreviations: EP, emergency preparedness; TD, task difficulty; OC, organizational command; MT, medical treatment; EPP, epidemic prevention and protection; SA, support and assurance; CR, collaborative results.
EFA
This study first assessed the data suitability using the Kaiser-Meyer-Olkin (KMO) measure and Bartlett’s test of sphericity. The KMO value was 0.958 (i.e., greater than 0.9), indicating that the sample size was adequate for the EFA. For the Bartlett’s test, the χ2/df was 40,417.231/780 (P<0.001), which led to the rejection of the null hypothesis of independence among the variables and suggested that the data were suitable for the EFA.
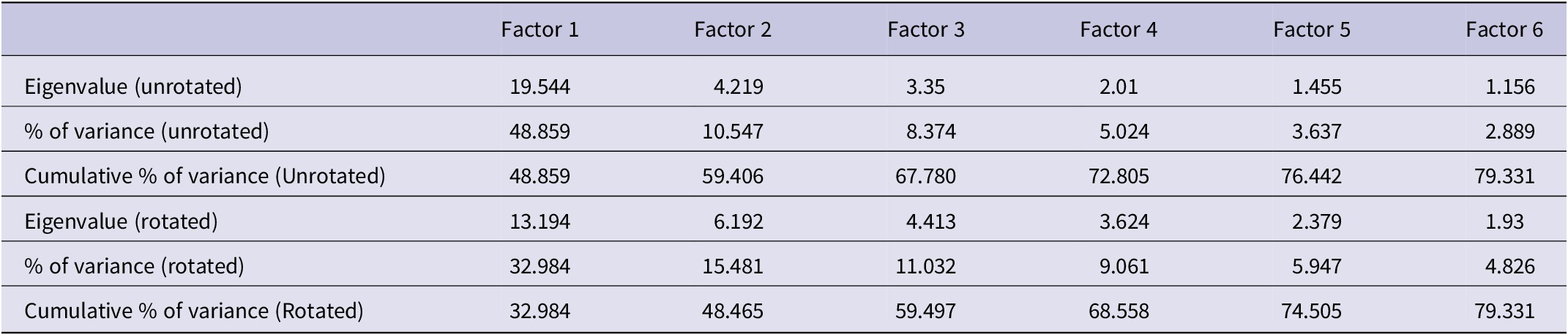
This study then used an EFA to extract the internal structural relationships within the data while reducing the dimensionality. The EFA results revealed that the first factor accounted for more than 40% of the total variance, and the cumulative variance contribution of the six factors was 79.331% (i.e., greater than 70%; Table 4). Thus, the 6 factors strongly accounted for the primary data information.
Table 4. EFA results
SEM Evaluation
This study adjusted the SEM to analyze the results for the collaborative outcomes during major infectious disease outbreaks; the subsequent path analysis revealed improved fit indices. The χ2/df was 2.484 (P=0.051), indicating a non-significant difference. The GFI was 0.995, the AGFI was 0.974, and the RMSEA was 0.044. These values, particularly the RMSEA value of less than 0.05, suggested that the model had acceptable fit. The fit coefficients significantly improved after the model’s adjustment, indicating that the model fit well and had ideal specification (Table 5).
Table 5. Path analysis of the GFI test

Abbreviations: χ2/df, the chi-square test of goodness of fit; GFI, goodness of fit index; AGFI, adjusted goodness of fit index; NFI, normed fit index; CFI, comparative fit index; RMSEA, root mean square error of approximation.
Hypotheses Tests
This study determined the final adjusted model of collaborative outcomes during major infectious disease outbreaks by evaluating a series of nested models based on the theoretical model of collaborative outcomes during such outbreaks. The hypothesized relationships were tested using a SEM (Figure 2). In SEM, latent variables (e.g., “Emergency Preparedness”) are inferred from observed indicators (questionnaire items). Each observed indicator is associated with an error term (e1-e4), representing the residual variance unaccounted for by the latent construct. For example, the latent variable “Medical Treatment” is measured by observed indicators such as “Emergency medical treatment plans are updated timely” (error = e1). Error terms (e) reflect measurement inaccuracies or unobserved factors influencing the indicators.
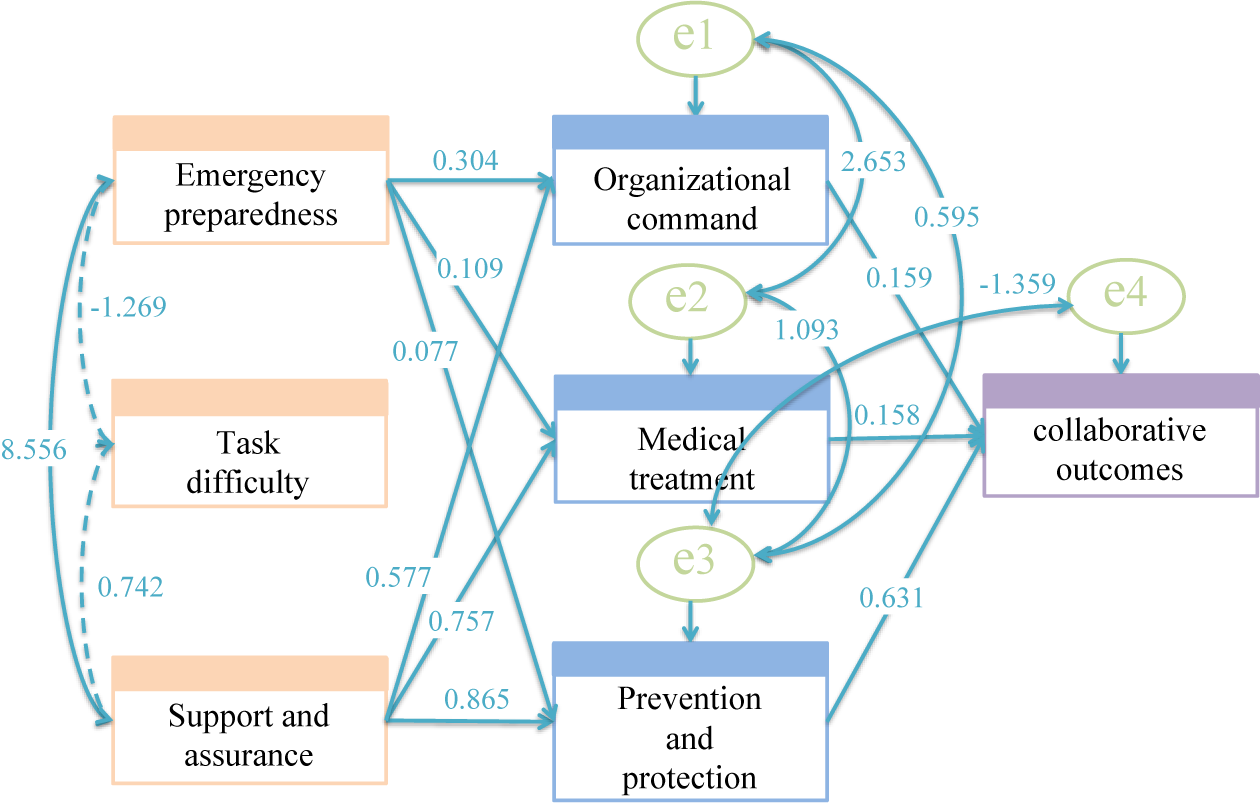
Figure 2. Path analysis results.
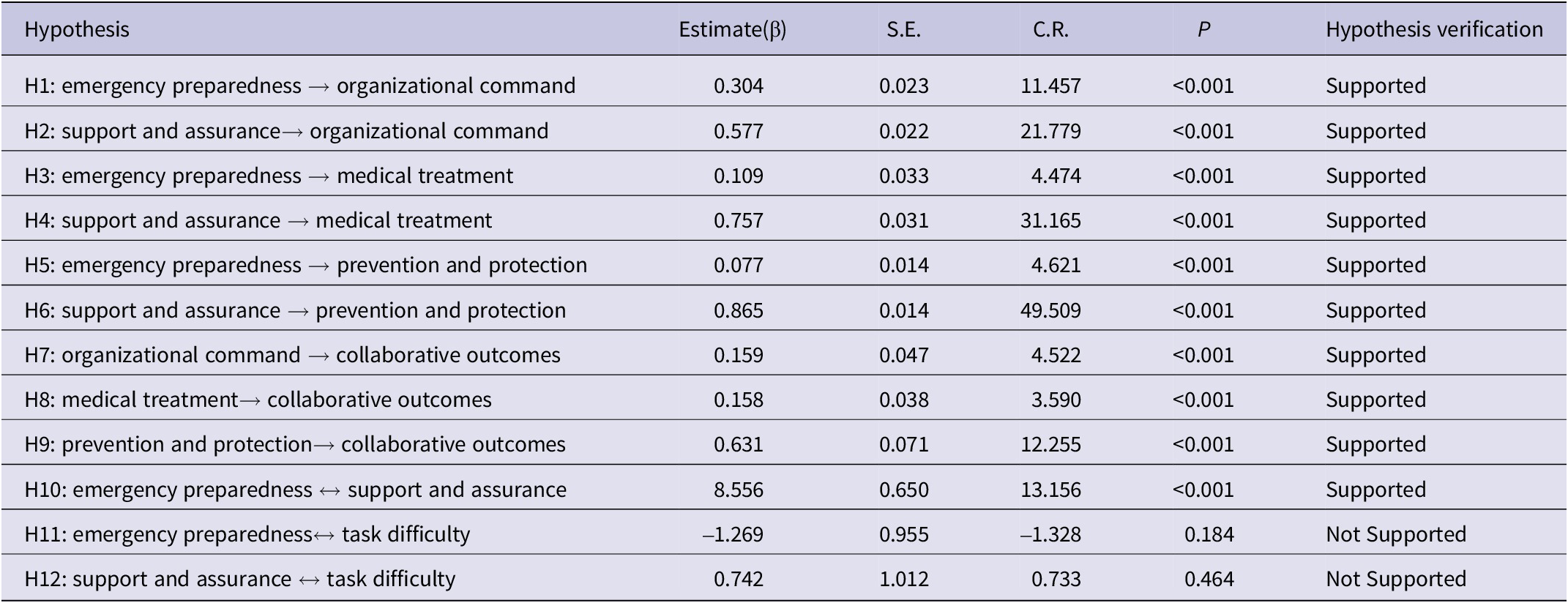
This study tested the hypotheses by examining the latent variables’ standardized path coefficients (Table 6). H1-H10 were all supported, indicating that emergency preparedness significantly predicted organizational command (H1: β = 0.304, P < 0.001), medical treatment (H3: β = 0.109, P < 0.001), and prevention and protection (H5: β = 0.077, P < 0.001). Support and assurance had even stronger effects on organizational command (H2: β = 0.577), medical treatment (H4: β = 0.757), and prevention and protection (H6: β = 0.865), all with P < 0.001. Moreover, organizational command, medical treatment, and epidemic prevention and protection had significant and positive impacts on collaborative outcomes. Notably, task difficulty showed no significant interaction with emergency preparedness (H11: β = -1.269, P = 0.184) or support and assurance (H12: β = 0.742, P = 0.464), as indicated by dashed paths in Figure 2. Error terms (e1-e4) in the model accounted for residual variances in observed indicators, with magnitudes ranging from 0.077 (prevention and protection) to 8.556 (emergency preparedness ↔ support and assurance covariance). This study’s findings showed that the latent construct epidemic prevention and protection (encompassing infection control training, PPE adequacy, and protocol implementation) significantly enhanced collaborative outcomes (β = 0.631, P < 0.001; Table 6). These terms reflect measurement limitations in fully capturing latent constructs.
Table 6. Results of hypotheses testing
Abbreviations: S.E., Scalar Estimates; C.R., Critical Ratio.
Discussion
This study’s results offer significant insights regarding collaborative outcomes during major infectious disease outbreaks, with implications for the academic research and practical management during future health crises. Emergency preparedness’ influence on collaborative outcomes is predominantly mediated through organizational command (H1: β = 0.304 → H7: β = 0.159), which serves as the critical operational bridge between planning and action. Support and assurance exerted the strongest direct effect on prevention and protection measures (β = 0.865, P < 0.001), nearly 11 times greater than preparedness’ impact (β = 0.077), underscoring resource allocation’s primacy over procedural planning alone. These results clarify that while preparedness initiates systems, leadership execution determines their efficacy. Emergency preparedness and support and assurance had significant positive influences on organizational command, medical treatment, and epidemic prevention and protection. Moreover, these factors had significant positive impacts on collaborative outcomes, highlighting the importance of comprehensive preparedness and robust support systems to achieve effective collaborative outcomes.
Organizational command mediated the effect of emergency preparedness on collaborative outcomes through a significant indirect pathway (β = 0.304 × 0.159 = 0.048, P < 0.001, Table 6), underscoring its role in operationalizing preparedness plans. This study’s results found that organizational command had a positive impact on collaborative outcomes. This finding aligns with literature that emphasized the importance of deploying leadership approaches through clear and flexible command chains when managing health crises.Reference Alami, Lehoux and Fleet 16 Moreover, an effective crisis response requires the ability to respond quickly to critical public health interventions (e.g., implementing lockdowns, reallocating medical resources, or mobilizing surge health care teams), which are often time-sensitive and context-dependent.Reference Caldeira, de Souza and Machado 17 Support and assurance exerted the strongest direct effect on prevention and protection (β = 0.865, P < 0.001), nearly 11 times greater than preparedness’ impact (β = 0.077), highlighting resource allocation’s critical role over procedural planning alone. This underscores the importance of institutional reforms aimed at improving emergency preparedness and responses. The establishment of a dedicated national or regional emergency management department is a strategic advancement in this direction and can significantly enhance the efficiency of preparedness and response efforts in the face of disasters.Reference Zhang, Wang and Wang 18 Such a centralized body would coordinate multi-sectoral resources, develop standardized response protocols, and conduct scenario-based training exercises. For example, models like China’s National Health Commission Emergency Office or the Federal Emergency Management Agency (FEMA) in the United States demonstrate how institutionalizing crisis management structures enhances preparedness and operational efficiency during disasters. This study’s results imply that adequate organizational command can facilitate rapid responses by ensuring needs are met; for example, by redeploying staff to different settings, such as hospitals and long-term care facilities.Reference Alami, Lehoux and Fleet 16 Moreover, this study’s findings highlight the complexity of cross-functional communication within health care organizations during a crisis. While our data primarily reflect challenges among clinical and managerial staff within hospitals, these insights may indirectly inform broader inter-organizational collaboration. As previously documented, the lack of coordinated and coherent communication can complicate the work of clinical and management staff.Reference Alami, Lehoux and Fleet 16 This underscores the importance of ensuring optimal collaboration and coordination among key health care stakeholders, including clinicians, nurses, hospital administrators, and infection control teams, to enhance the overall response efforts. This study identified the potential challenges in data-sharing among these internal stakeholders, particularly in situations of uncertainty and conflict.Reference Levesque, Sutherland and Watson 19 This finding suggests that defensive reactions and reluctance to share data can hinder effective collaboration and communication during a crisis. Therefore, addressing these barriers is crucial for improving overall response efforts and outcomes. While our findings focus on intra-organizational dynamics, similar barriers may extend to external partners in broader multi-sectoral collaborations, though this requires further investigation.
This study’s findings affirm that effective medical treatment significantly enhances collaborative outcomes during health crises. The global competition for essential medical equipment and drugs during the COVID-19 pandemic highlighted the critical importance of resource availability.Reference Alami, Lehoux and Fleet 16 Access to adequate medical equipment, including personal protective gear, ventilators, and diagnostic kits, is vital for positive collaborative outcomes, underscoring the need for efficient resource management during health crises. Similarly, the shortages of essential drugs, particularly for COVID-19 patients, underscore the importance of ensuring a consistent supply chain for necessary medications. This study’s results also emphasize the critical role of a well-trained and safeguarded health care workforce in facilitating effective collaborative outcomes.Reference Alami, Lehoux and Fleet 16 , Reference Florio, Zanella and Pesenti 20 Effective strategies include the rapid mobilization of health care providers and the use of telehealth services to maintain coverage and share expertise.
The findings align with studies demonstrating that systematic PPE training reduces protocol deviations, suggesting that workforce safety protocols are critical to operational efficiency.Reference Doos, Hughes and Pham 21 , Reference Kwon, Burnham and Reske 22 The high factor loadings of training (X38) and PPE adequacy (X39) indicate their centrality to infection control systems. This is significant, as the literature has highlighted the critical role of the public health workforce, training, protective equipment, and hospital infection control measures in managing and mitigating such crises.Reference Alami, Lehoux and Fleet 16 Literature has also noted a significant shortage of human resources in the public health sector, which impacts surveillance activities, epidemiological investigations, and crises promotion and prevention activities.Reference Alami, Lehoux and Fleet 16 This study supports this finding by suggesting that a sufficiently well-prepared public health workforce is essential for effective collaborative outcomes during health crises. The literature has also emphasized the need for training on the correct use of personal protective equipment. The presence of trained observers are essential to reduce the risk of self-contamination.Reference Harris and Adalja 23 This study’s results underscore the importance of such training in achieving positive collaborative outcomes, and highlight the need for clarification and education for all essential staff members through close planning and open communication with trained infection control personnel.Reference Griffin, Karas and Ivascu 24 Moreover, the importance of the proper disposal of soiled objects and sterilization of vacated rooms in hospital settings has garnered considerable attention;Reference Harris and Adalja 23 these infection control measures play a crucial role in limiting the spread of a contagion and optimizing resource allocation during a health crisis.
This study’s findings demonstrate that emergency preparedness had a positive impact on collaborative outcomes during health crises and was mediated through organizational command, medical treatment, and epidemic prevention and protection. Task difficulty showed no significant interaction with preparedness (β = -1.269, P = 0.184) or support systems (β = 0.742, P = 0.464), suggesting current frameworks may inadequately address high-complexity scenarios (e.g., novel zoonotic outbreaks). This reinforces the perspective that a thorough state of preparedness, including planning, the development of response capabilities, and public policy formulation, is essential for effective disaster risk management. They also agree with the scholarly consensus that has emphasized the vital role of emergency preparedness in managing and mitigating the repercussions of health crisesReference Alami, Lehoux and Fleet 16 , Reference Mitchell, Glavovic and Hutchinson 25 and the need for coherence between risk assessment, surveillance, early warning systems, resilient infrastructure, and coordinated incident management.Reference O’Brien, O’ Keefe and Gadema 26 –Reference Ong, Prasetyo and Lagura 28 Further, this study’s findings echo a prior study’s assertion that disaster planning and preparedness are instrumental for reducing risks and minimizing potential damage.Reference Kachali, Haavisto and Leskelä 29 However, our results also reinforce the literature’s caution against over-reliance on preparedness alone. Collaborative outcomes are co-determined by community engagement, citizen behavior, and multisector policy integration. For instance, despite robust preparedness systems, regions with low public trust in authorities or fragmented policy coordination experienced slower outbreak containment.Reference Lazarus, White and Wyka 30 In light of the complex and integrated nature of public health emergency preparedness, which involves components such as effective leadership, collaborative networks, strategic planning, and community involvement,Reference Khan, O’ Sullivan and Brown 31 the acknowledged deficiencies in global readiness for a catastrophic health emergency 32 highlight the need for enhanced investment in risk communication and community engagement strategies, which are vital for fostering public trust in official health directives.Reference Florio, Zanella and Pesenti 20 , Reference Bollyky, Hulland and Barber 33 –Reference Chiu, Crooks and Fraser 35 However, as the literature has shown, emergency preparedness alone cannot determine collaborative outcomes; rather, it must be considered alongside a multitude of other factors. These include local epidemic preparedness and response capabilities; citizen behavior, such as physical distancing and mask-wearing; and the interplay between health, economic, and social response policies.Reference Kachali, Haavisto and Leskelä 29 These factors significantly affect collaborative outcomes and enhance the understanding of the intricate dynamics of crises management.Reference Kachali, Haavisto and Leskelä 29 Therefore, it is critical to enact thorough and holistic emergency preparedness initiatives to address the deficiencies and strengthen collaborative outcomes during health crises.
Further, supportive measures, such as information and communication security, financial support, and diagnostic testing, had a positive impact on collaborative outcomes during health crises and were mediated through organizational command, medical treatment, and epidemic prevention and protection. These findings align with previous studies in that reliable real-time data are essential for effective decision-making, while electronic logistics management information systems can support health authorities in coordinating effective responses to ensure the timely availability of supplies during crises.Reference Wasswa, Oundo and Oteba 36 Meanwhile, the necessity for sufficient financial resources to support preparedness initiatives has been well-documented.Reference Sirleaf and Clark 37 The capacity to mobilize rapid and adaptable financial resources has been highlighted as being crucial for managing health crises.Reference Alami, Lehoux and Fleet 16 This study’s emphasis on the pivotal role of effective diagnostics in collaborative outcomes reinforces the urgency of the need for a diagnostic agenda that guarantees the deployment of these critical tools.Reference Boehme, Hannay and Pai 38 , 39 The limited availability of essential tests at the primary care level underscores the importance of accessible diagnostics for the early detection and response to potential outbreaks.Reference Kohli, Walia and Mazumdar 40
This study contributes to the literature by providing a detailed analysis of the factors that influence collaborative outcomes during infectious disease outbreaks. The findings suggest that a multifaceted approach that involves preparedness, organizational command, medical treatment, and prevention and protection measures is necessary for effective collaborative outcomes. Both emergency preparedness and supportive interventions exert constructive influences on collaborative outcomes, as transmitted through the intermediaries of organizational command, medical treatment, and epidemic prevention and protection measures. This study further contributes to the deeper understanding of the complexities involved in crises responses by illuminating the critical dimensions that demand enhancement in future health crises management initiatives. This study’s insights are pivotal for formulating policies and practices and ultimately improving the resilience and responsiveness of health care systems in the face of emerging infectious diseases and other health threats.
To address potential barriers that should be considered when improving effective collaboration and communication during a crisis, we propose actionable strategies. First, standardized data-sharing protocols should be implemented. Interoperable digital platforms should be developed to facilitate real-time information exchange between departments while ensuring data security, modeled after WHO’s Health Cluster Information Management System. Second, cross-functional crisis teams should be established. Representatives from clinical, administrative, and infection control units should be embedded in joint task forces to streamline decision-making, as successfully piloted in Singapore’s COVID-19 response. Third, an incentive structure should be introduced, linking compliance with collaborative metrics to institutional funding or accreditation, drawing lessons from the U.S. Hospital Preparedness Program. While our findings focus on intra-organizational dynamics, similar barriers may extend to external partners in broader multisectoral collaborations, though this requires further investigation.
This study’s limitations include its cross-sectional design, which limits its ability to establish causal relationships between variables, and the reliance on self-reported data. This may have introduced bias. Furthermore, direct evidence of inter-organizational dynamics requires further investigation beyond the scope of this health care facility-centered research. Future studies should explicitly examine mechanisms for bridging institutional silos, including public-private health sector partnerships, to strengthen crisis responses. Future research can benefit from a longitudinal design that tracks the changes in collaborative responses over time and explore objective collaboration and outcome measures, while expanding investigations into public-private partnerships to address inter-organizational barriers.
Conclusions
This study’s results underscore the critical roles of organizational command, medical treatment, and epidemic prevention and protection in achieving positive collaborative outcomes during health crises. Emergency preparedness and supportive measures enhance collaborative outcomes, with their effects mediated through the same key factors. Notably, hypotheses positing mutual impacts between task difficulty and preparedness/support systems—were not supported, suggesting that high-complexity outbreak scenarios may require tailored frameworks beyond generic preparedness models. These insights contribute to the academic understanding and practical management of health crises responses; they also provide a robust framework for policymakers and health care professionals to enhance preparedness, leadership, treatment protocols, and preventive measures. Future research should explore contextual thresholds where task difficulty begins to strain preparedness systems, thereby informing adaptive response strategies. By focusing on these areas, health care systems can be better equipped to manage future health crises and protect public health.
Supplementary material
The supplementary material for this article can be found at http://doi.org/10.1017/dmp.2025.127.
Data availability statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Author contribution
ML Conceptualization; PL Data curation; LY Formal analysis; ML, LZ and WY Funding acquisition; ML Investigation; LY and PL Methodology; ML Project administration; MJ Resources; PL Software; ML Supervision; MJ Validation; LY Visualization; LY and ML Writing - original draft; LY, PL, MJ, ML, LZ and WY Writing - review & editing.
Funding statement
This work was supported by the National Natural Science Foundation of China [grant numbers 72274209, 71673291, 72174204, and 72104140]; Shanghai top talent Program of Eastern Talent Plan [grant numbers BJWS2024052]; Medical Science and Technology Youth Training Program [grant number 21QNPY050]; the Soft Science Project of Shanghai Science and Technology Innovation Action Plan [grant number 23692113200, 23692115000].
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.










