In the last 2 decades, the number of mass casualty incidents (MCIs) has risen globally, with over 2 million fatalities and many more injured. 1 MCIs are short-term events that overwhelm local medical care systems, where the volume of patients exhausts available resources and capabilities. 2 The unprecedented number of recent major incidents has challenged the health systems, increased the need to review MCI responses, and review lessons from previous MCIs pre-hospital. Reference Brohi and Tallach3 Time to initial response in mass casualty events is crucial in determining outcomes in the early stages of an injured patients’ care. Reference Harmsen, Giannakopoulos and Moerbeek4,Reference Sampalis, Lavoie and Williams5 The time from injury to reaching definitive care is known as pre-hospital time (PHT). An extended pre-hospital period is associated with increased mortality rates, and contemporary trauma systems strive to reduce PHT to improve patient outcomes. Reference Harmsen, Giannakopoulos and Moerbeek4–Reference Heemskerk, Abode-Iyamah and Quinones-Hinojosa6
There is a lack of consensus about whether “scoop and run” (transporting patients as quickly as possible) or “stay and play” (stabilizing patients and initiating advanced treatment on scene) is most advantageous for patient outcomes. Reference Gauss, Ageron and Devaud7 Total PHT encompasses sequential intervals including pre-alarm, response, on-scene, and transport time. Reference Bigdeli, Khorasani-Zavareh and Mohammadi8,Reference Carr, Caplan and Pryor9 Each interval is associated with unique activities that may impact total PHT. Reference Bigdeli, Khorasani-Zavareh and Mohammadi8 Most pre-hospital care evidence focuses on response, on-scene, and/or transport time as the main indicators of PHT, and there is little previous research investigating the “pre-alarm interval,” which is the time between injury and ambulance departure. Reference Bigdeli, Khorasani-Zavareh and Mohammadi8,Reference Waalwijk, van der Sluijs and Lokerman10 Therefore, the current understanding of total PHT delays is unclear. Previous MCIs show that PHT intervals were 2.5 times longer than standard non-MCI Emergency Medical Services (EMS) responses. Reference Schenk, Wijetunge and Mann11 Single incident reports suggest that a number of factors have been implicated in extended PHTs during an MCI, including delays to EMS deployment, resource availability, and location. Reference Bigdeli, Khorasani-Zavareh and Mohammadi8,Reference Schenk, Wijetunge and Mann11,12 These issues are not limited to low- or middle-income countries alone, and have also been reported in high-income settings, indicating that other factors may contribute to PHT delays. Reference Schenk, Wijetunge and Mann11,12 In order to improve responses and outcomes for future incidents, it is important to investigate which factors are related to extended PHTs across published MCI reports. Therefore, this systematic review aimed to investigate the total PHT in different trauma-related MCIs and to identify factors associated with extended PHT for triaged patients at the MCI scene.
Methods
This systematic review was registered in the international prospective register of systematic reviews (PROSPERO) with registration number CRD42022288580. The review was performed according to The Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) recommendations in its conduct and reporting. Reference Page, McKenzie and Bossuyt13
Eligibility Criteria
Eligibility criteria and search strategies were developed using PEOS (Population, Exposure, Outcome, and Studies) (Table 1).
Table 1. Eligibility criteria

Sources of Information and Search Strategy
The search was conducted between January and February 2022 by 2 independent reviewers (FA and EKA). The following electronic databases were used to search for evidence: Web of Science (Thomson Reuters, New York, NY, USA), CINAHL Complete (EBSCO Information Services, Ipswich, MA, USA), MEDLINE (US National Library of Medicine, National Institutes of Health, Bethesda, MD, USA), and EMBASE (Elsevier, Amsterdam, Netherlands). Reference lists from identified articles were checked for missed publications. A grey literature search was conducted on the following databases: World Health Organization, Google Search, Google Scholar, and E-Theses Online Service. Reviewers (FA and EKA) searched The British Library to retrieve articles not available in full text from selected databases. The search terms were a combination of keywords and MeSH terms: “Mass Casualty Incidents,” “Disasters,” “Triage,” “Priority,” “Emergency Medical Services,” “Ambulances,” “Pre-hospital,” “Delay,” “Time”. Keywords were combined with Boolean Operators “OR” to expand the initial searches and then “AND” to combine records retrieved during individual searches (Supplemental Table 1).
Study Selection and Data Extraction
All articles selected from the database searches were imported into EndNote20 for Windows software (Clarivate Analytics, Philadelphia, PA, USA) to remove duplicates. Reference Gotschall14 Following this, 2 independent reviewers (FA and EKA) exported the articles into Rayyan software to screen titles and abstracts. Reference Ouzzani, Hammady and Fedorowicz15 Finally, full-text articles were assessed for inclusion against eligibility criteria. If there was any disagreement between the reviewers, a third independent reviewer (EC) was used for arbitration.
Quality Appraisal
Existing systematic review quality appraisal tools are either specific to a study methodology or focus on a specific patient cohort or case. Reference Ma, Wang and Yang16 There is no tool specifically designed to assess quality in mass casualty/ mass case evidence, therefore, a quality assessment checklist was adapted from Joanna Briggs Institute (JBI) Critical Appraisal Tools for case reports and NHS Guidelines for Major Incidents and Mass Casualty Events (Table 2). Reference Moola, Munn and Tufanaru17,18 The checklist has 10 questions, each of which has 4 potential answers: Yes (Y), No (N), Unclear (U), and Not Applicable (NA). The quality assessment of the developed tool was calculated based on the percentage of questions answered with “Yes.” According to the results of this checklist, each study was classified as low quality (< 50%), moderate quality (from 50% to 70%), and high quality (> 70%). Reference Stéfani, de Melo and Zardeto19 Quality appraisal was performed independently by 2 reviewers (FA and EKA).
Table 2. The quality assessment checklist for included studies a
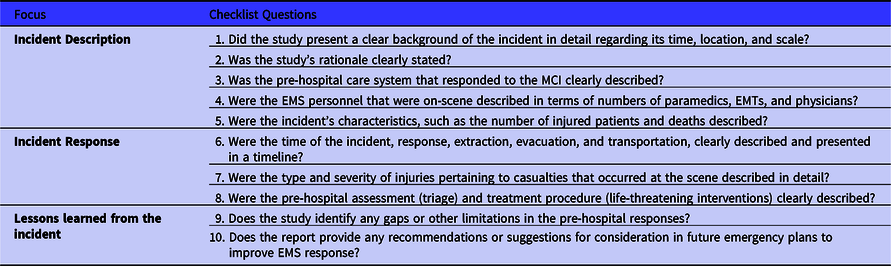
a The quality assessment tool was adapted from the following sources: the Joanna Briggs Institute (JBI) Critical Appraisal Tools for case reports, Reference Moola, Munn and Tufanaru17 and the NHS Guidelines for Major Incidents and Mass Casualty Events. 18
Data Analysis
Meta-analysis was not possible due to heterogeneity in timing measures, or incomplete timings, therefore, a narrative synthesis was performed based on Cochrane’s recommendations. Reference Ryan20 Studies that met the eligibility criteria were synthesized, focusing on methodological approach, relationships within and between studies and interpretation of findings. Studies were compared by location and design, incident types and setting, number of victims, and pre-hospital time, as well as responders, triage tools, mode of transportation, and mortality. The median and interquartile range (IQR) were calculated for each study that included PHT sequentially (per individual patient).
Definitions
-
(1) Mass Casualty Incident (MCI): A short-term event that overwhelms the local medical care systems with many patients that exhaust the available resources and capabilities. 2
-
(2) Pre-hospital time (PHT): The interval between injury time to hospital arrival.
-
(3) MCI triage: A sorting process in an incident scene for casualties into classifications based on their injury severity to distribute limited resources rationally. Reference Foley, Reisner and Ciottone21
Results
Study Selection and Data Extraction
Initial database searches resulted in 1992 documents (Figure 1), of which 781 duplicates were removed. The title and abstract screening revealed 31 potential studies meeting eligibility criteria. Of these, 3 studies were not available in full text. Therefore, full-text screening was carried out on the remaining 28 studies, of which 17 were excluded, and 11 papers met the inclusion criteria. One study was included from the citation and grey literature search, resulting in 12 studies for analysis.
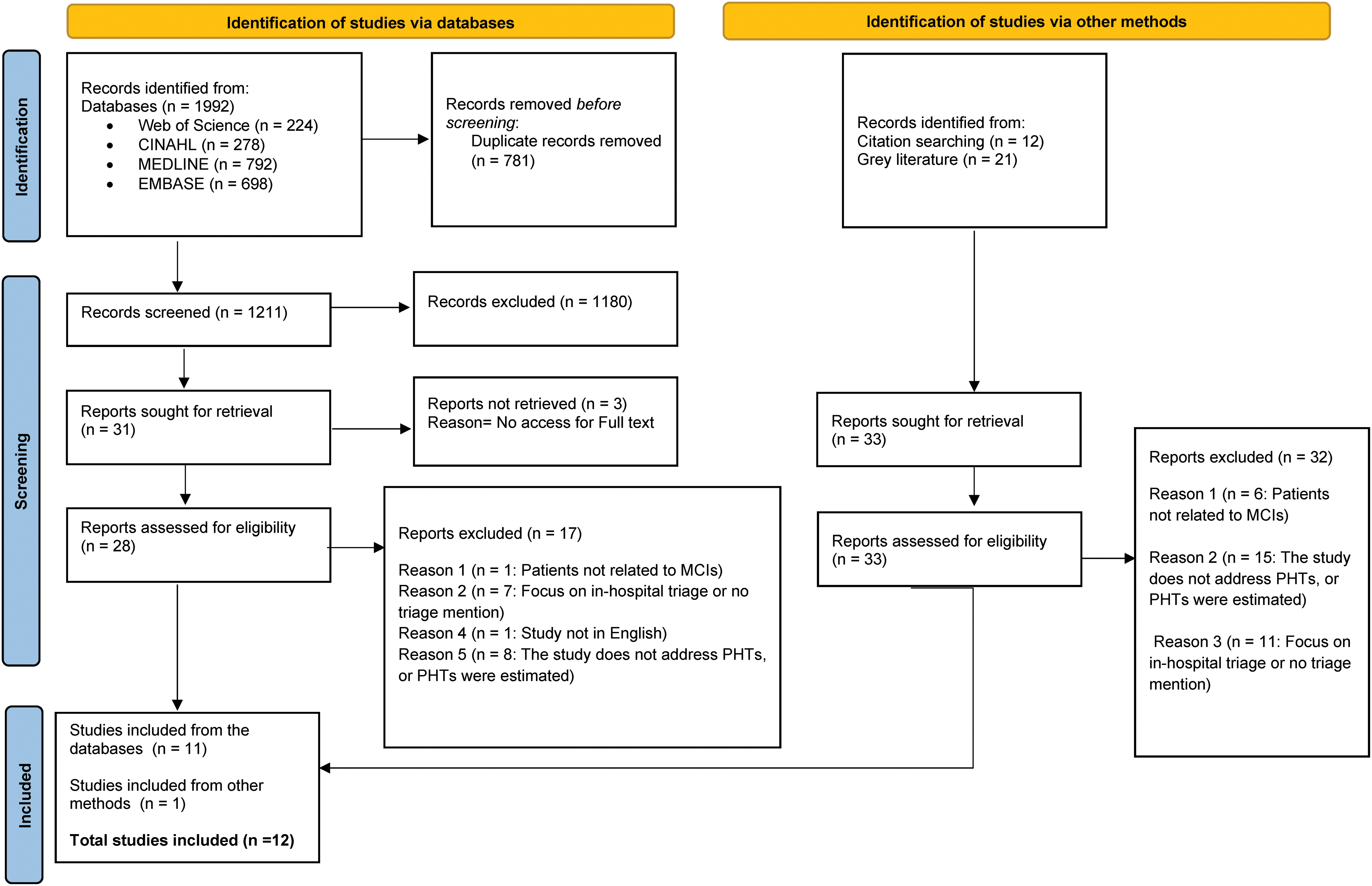
Figure 1. Modified PRISMA 2020 flow diagram for new systematic reviews, which included searches of databases and other sources. Abbreviation: PRISMA, Preferred Reporting Items of Systematic Reviews and Meta-Analysis.
Study Characteristics
Study methodologies comprised 6 retrospective observational cohort studies, Reference Sollid, Rimstad and Rehn22–Reference Raux, Carli and Lapostolle27 and 6 case reports (Table 3). Reference O’Keefe, Kheir and Martin28–Reference Leiba, Halpern and Priel33 Two studies were conducted in the USA, Reference Kahn, Schultz and Miller26,Reference O’Keefe, Kheir and Martin28 2 in Israel, Reference Raiter, Farfel and Lehavi32,Reference Leiba, Halpern and Priel33 2 in France, Reference Travers, Carfantan and Luft23,Reference Raux, Carli and Lapostolle27 and 2 in the Netherlands, Reference Welling, van Harten and Henny25,Reference Postma, Winkelhagen and Bloemers30 while the remaining were conducted within the UK, Reference McLeod, Hodgetts and Mahoney24 Canada, Reference Mulvey, Shaw and Betzner29 Norway, Reference Sollid, Rimstad and Rehn22 and Taiwan. Reference Lin, Pan and Wen31 Incidents were varying in nature and included terrorist attacks (n = 4) Reference Sollid, Rimstad and Rehn22,Reference Raux, Carli and Lapostolle27,Reference Raiter, Farfel and Lehavi32,Reference Leiba, Halpern and Priel33 and military operations (n = 2) Reference Travers, Carfantan and Luft23,Reference McLeod, Hodgetts and Mahoney24 (Supplemental Figure 1). The remainder focused on single incidents involving a balcony collapse, Reference O’Keefe, Kheir and Martin28 a train crash, Reference Kahn, Schultz and Miller26 a bus rollover, Reference Mulvey, Shaw and Betzner29 and a building fire, Reference Welling, van Harten and Henny25 as well as a flight crash, Reference Postma, Winkelhagen and Bloemers30 and a non-intentional explosion. Reference Lin, Pan and Wen31 Two studies focused on single transportation modes: air ambulances in French military operations, Reference Travers, Carfantan and Luft23 and ground ambulances in Paris attacks, while the rest involved air, and ground ambulances. EMS providers (paramedics, emergency medical technicians EMTs, and physicians) were involved in all studies. Additionally, nurses and emergency physicians responded to 3 MCIs, Reference Sollid, Rimstad and Rehn22,Reference McLeod, Hodgetts and Mahoney24,Reference O’Keefe, Kheir and Martin28 and anesthesiologists responded to the terrorist attacks in Norway. Reference Sollid, Rimstad and Rehn22
Table 3. Characteristics for the included studies in the systematic review
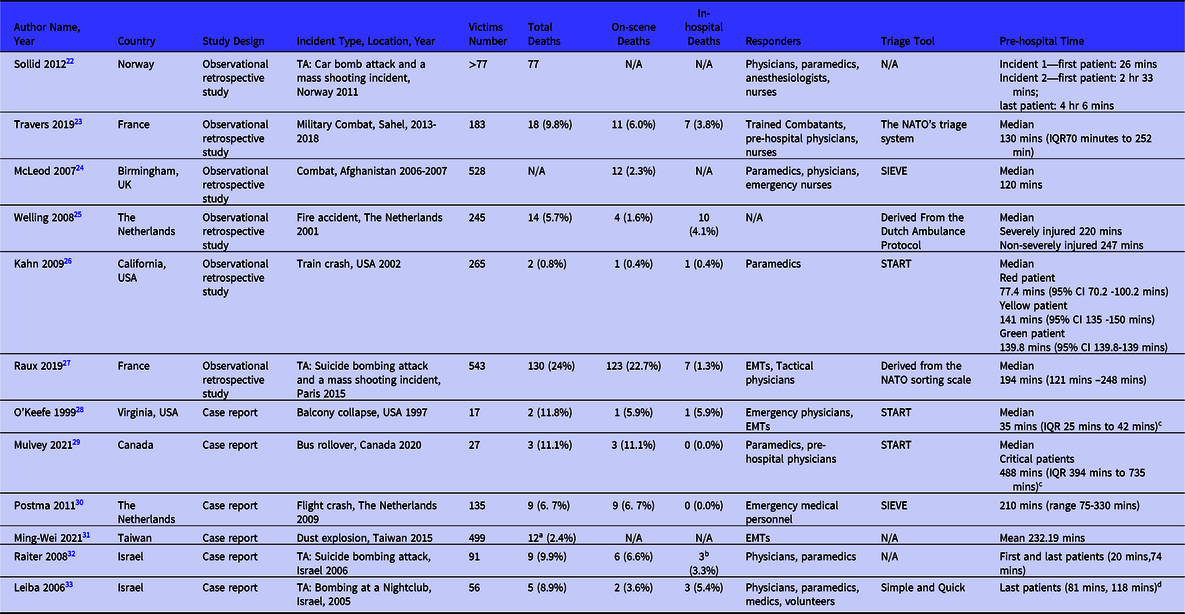
Abbreviations: IQR, Interquartile range; mins, minutes; N/A, The information was not reported; TA, terrorist attack; 95%CI, 95% confidence interval.
a Mortality data from a different study that reported the same incident but did not meet eligibility criteria. Reference Yang and Shih34
b Patients already dead on hospital arrival (transported via private vehicles).
c The reviewers calculated the IQR median for any case report that included all patients’ PHT sequentially (per individual patient).
d PHTs were reported for every patient in two different hospitals.
In total, 2589 patients were included, and overall mortality was 14.7% (n = 269). Most patients were formally triaged at the scene (2237, 86.4%), and “non-triage” occurred where victims were immediately transported or self-presented to the hospital. Reference Sollid, Rimstad and Rehn22,Reference Kahn, Schultz and Miller26 Of the triaged patients, 482 (29.0%) were red (critical, P1), 522 (35.6.5%) were yellow (delayed, P2), 475 (32.4%) were green (minor, P3), and 172 (10.8%) were black (dead-on-scene, P4) (Supplemental Table 2). The START (Simple triage and rapid treatment) system was implemented in 3 mass incidents in North America (USA and Canada), Reference Kahn, Schultz and Miller26,Reference O’Keefe, Kheir and Martin28,Reference Mulvey, Shaw and Betzner29 and the SIEVE system was utilized in 2 European MCIs (UK and The Netherlands). Reference McLeod, Hodgetts and Mahoney24,Reference Postma, Winkelhagen and Bloemers30
Quality Appraisal
Of the 6 observational studies, 4 papers were rated as moderate quality, Reference Sollid, Rimstad and Rehn22,Reference McLeod, Hodgetts and Mahoney24,Reference Kahn, Schultz and Miller26,Reference Raux, Carli and Lapostolle27 and 2 were deemed high quality. Reference Travers, Carfantan and Luft23,Reference Welling, van Harten and Henny25 For the case reports, 3 were deemed to be of moderate quality, Reference Postma, Winkelhagen and Bloemers30,Reference Lin, Pan and Wen31,Reference Leiba, Halpern and Priel33 while 3 reports were graded as high quality (Table 4). Reference O’Keefe, Kheir and Martin28,Reference Mulvey, Shaw and Betzner29,Reference Raiter, Farfel and Lehavi32
Table 4. Quality assessment of included studies

Pre-hospital Times in Mass Casualty Incidents
Most studies documented pre-hospital times of 2 hours or longer, Reference Travers, Carfantan and Luft23,Reference McLeod, Hodgetts and Mahoney24,Reference Kahn, Schultz and Miller26,Reference Raux, Carli and Lapostolle27,Reference Mulvey, Shaw and Betzner29–Reference Lin, Pan and Wen31 although PHTs were reported variably as means, medians, and sequences (per individual patient) (Table 3). Three studies focused on reporting the PHTs for individual patients who were of particular note (first and/ or last arrivals). Reference Sollid, Rimstad and Rehn22,Reference Raiter, Farfel and Lehavi32,Reference Leiba, Halpern and Priel33 Two of the studies used sub-grouped medians that were based on triage classifications. Reference Welling, van Harten and Henny25,Reference Kahn, Schultz and Miller26
In studies where average timings were reported or calculated by the reviewer, the shortest time to arrival at a hospital was a median of 35 minutes, following the balcony collapse in the USA where 16 people were injured (Figure 2). Reference O’Keefe, Kheir and Martin28 The longest reported time was 488 minutes, when 12 critically injured patients were evacuated following the bus rollover in Canada. Reference Mulvey, Shaw and Betzner29 Otherwise, timings ranged from 120 minutes (UK military incident) to 233.5 minutes for the fire incident in the Netherlands (Figure 2). Reference McLeod, Hodgetts and Mahoney24,Reference Welling, van Harten and Henny25
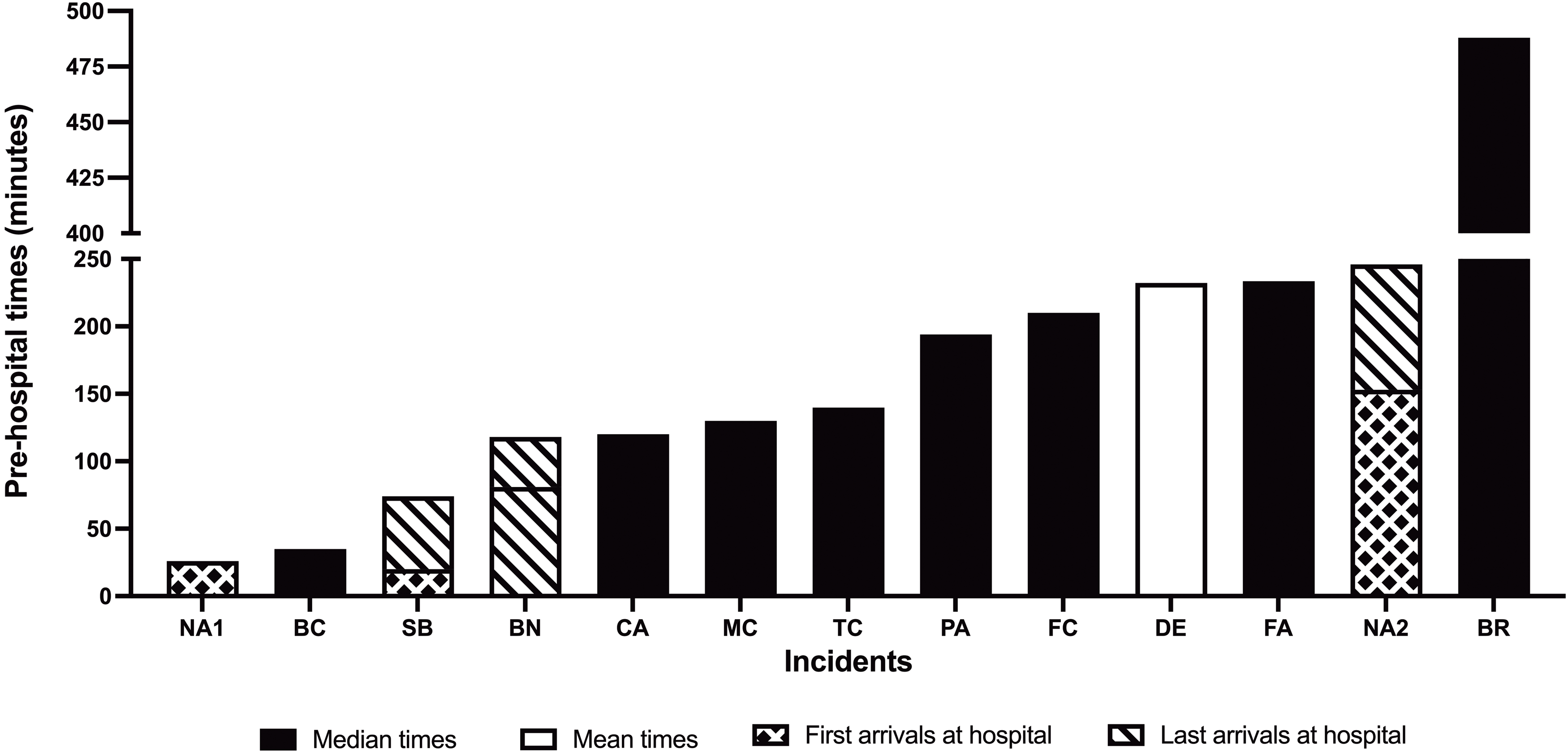
Figure 2. Bar chart shows pre-hospital time in minutes for mass casualty incidents included in the review. Abbreviations: NA1, 1st incident of Norway attacks (Car bombing) 2011; BC, Balcony collapse in Virginia 1997; SB, Bombing attack in Tel Aviv, Israel 2006; BN, Bombing at a nightclub, Israel 2005; CA, UK military operations, Afghanistan 2006-2007; MC, French military combat, Sahel region 2013-2018; TC, California train crash 2002; PA, Bombing attack and a mass shooting incident, Paris 2015; FC, Flight accident, The Netherlands 2001; DE, Dust explosion, Taiwan 2015; FA, Fire accident, The Netherlands 2001; NA2, 2nd incident of Norway attacks (Mass shooting ) 2011; BR, Bus rollover, Canada 2020.
Of the studies that reported the PHTs of individual patients, Reference Sollid, Rimstad and Rehn22,Reference Raiter, Farfel and Lehavi32,Reference Leiba, Halpern and Priel33 the first victims of a Norwegian car bombing arrived at trauma centers 26 minutes after the first incident (Figure 2). Reference Sollid, Rimstad and Rehn22 Similarly, first patients arrived 20 minutes after a Tel Aviv bomb attack in 2006. Reference Raiter, Farfel and Lehavi32 The most prolonged times for final patient arrival was 118 minutes following a nightclub bombing in 2005, and 246 minutes after the Norwegian mass shooting event. Reference Leiba, Halpern and Priel33 Two civilian MCIs with the largest numbers of casualties reported pre-hospital times of 194 and 232 minutes respectively (Table 3). Reference Raux, Carli and Lapostolle27,Reference Lin, Pan and Wen31 However, this volume-delay association was not observed across all MCIs, and the incident with the most prolonged times involved only 27 patients (Table 3). Reference Mulvey, Shaw and Betzner29 Similarly, there was no obvious relationship between PHTs and proportion of deaths (Figure 2, Table 3), although 3 studies failed to report mortality data. Reference Sollid, Rimstad and Rehn22,Reference McLeod, Hodgetts and Mahoney24,Reference Lin, Pan and Wen31
Factors associated with delayed pre-hospital time
Difficult access to incident locations
Inaccessibility to the incident site due to geographical location or obstruction was the main reason for patient triage and transportation delays in 3 studies. Reference O’Keefe, Kheir and Martin28–Reference Postma, Winkelhagen and Bloemers30 The Columbia icefield bus rollover occurred in an extreme environment, and despite having access to aeromedical services and physicians in the field, the steep slopes challenged the response teams resulting in a prolonged PHT of more than 4 hours for the first critical patient (Figure 3). Reference Mulvey, Shaw and Betzner29 At the Schiphol air crash, the evacuation and transportation for the first patient was delayed 74 minutes due to extremely muddy conditions. Reference Postma, Winkelhagen and Bloemers30 Similarly, road obstructions following a balcony collapse prevented EMS providers from reaching injured patients, which extended the pre-hospital period to a median of 35 minutes (Figure 3). Reference O’Keefe, Kheir and Martin28

Figure 3. Scatterplot represents factors associated with delays by pre-hospital times and number of casualties.a Abbreviations: BC, Balcony collapse in Virginia 1997; BR, Bus rollover, Canada 2020; BN, Bombing at a nightclub, Israel 2005; SB, Bombing attack in Tel Aviv, Israel 2006; FC, Flight accident, The Netherlands 2001; MC, French military combat, Sahel region 2013-2018; FA, Fire accident, The Netherlands 2001; TC, California train crash 2002; DE, Dust explosion, Taiwan 2015; PA, Bombing attack and a mass shooting incident, Paris 2015; CA, UK military operations, Afghanistan 2006-2007.
aThe terrorist attacks in Norway 2011 were not included in the graph as the number of casualties was not reported.
Delay to secure hot zones
Four studies reported that safety considerations had a crucial impact on extending the pre-hospital period during MCI triage responses. Reference Sollid, Rimstad and Rehn22–Reference McLeod, Hodgetts and Mahoney24,Reference Raux, Carli and Lapostolle27 In the Utoya Island mass shooting, the EMS responders had difficulty triaging wounded victims due to the ongoing shooting at the scene, and Helicopter Emergency Medical Service (HEMS) units could not land near the site, resulting in delays in securing the scene for 30 minutes. Reference Sollid, Rimstad and Rehn22 In a similar civilian event, Paris terrorist attacks involved active shooting and hostage-taking, which took 3 hours for police and tactical teams to secure the scene and evacuate casualties (Figure 3). Reference Raux, Carli and Lapostolle27 Two military studies reported delays due to tactical responses, Reference Travers, Carfantan and Luft23,Reference McLeod, Hodgetts and Mahoney24 1 within the battlefield, where deployments were intentionally extended for safety concerns. Reference Travers, Carfantan and Luft23 The other study reported extended PHT of 5 hours due to safety considerations when transporting victims from the incident scene. Reference McLeod, Hodgetts and Mahoney24
Adverse decision-making in MCI responses
Several studies found that uncertainty in MCI responses and triage misclassification were associated with prolonged times to care (Figure 3). Reference Welling, van Harten and Henny25,Reference Kahn, Schultz and Miller26,Reference Lin, Pan and Wen31 In the Taiwan color-dust explosion, although triage was implemented effectively at the scene, EMS providers did not follow the triage decisions to prioritize severely injured for transportation to hospital. Reference Lin, Pan and Wen31 As a result, the average pre-hospital time for severely injured patients was higher than for moderately injured patients (274.55 and 198.37 minutes, respectively). Reference Lin, Pan and Wen31 Similarly, there was no distinction regarding transportation priorities for different patient classifications following a fire incident because the response units failed to initiate effective triage response. Reference Welling, van Harten and Henny25 During the rail crash in California, the triage response incorporated significant rates of over-triaging, which led to transferring critically injured patients with non-urgent patients (over-triaged) to the hospital as the same transportation priority. Reference Kahn, Schultz and Miller26
Discussion
This systematic review investigated pre-hospital timings and factors affecting PHT delays during mass casualty events. MCIs were heterogeneous in nature and PHT varied greatly. Most MCIs reported pre-hospital timing delays of more than 2 hours, with the longest spanning over 8 hours. Three main factors were associated with prolonged PHTs including incident location, safety, and adverse decision-making in MCI responses. Overall, the quality of studies was rated as moderate to high.
The extended interval from injury time to definitive care is a known detriment associated with poor patient outcomes. Reference Heemskerk, Abode-Iyamah and Quinones-Hinojosa6 Previous pre-hospital studies focused solely on transport timeframes in non-MCI EMS responses. Reference Pham, Puckett and Dissanaike35–Reference Khorasani-Zavareh, Mohammadi and Bohm37 However, these studies cannot convey the complexity of factors affecting PHTs within an MCI. In this review, PHTs were varied with most being at least 2 hours or longer; MCIs were heterogeneous in terms of cause, EMS provision, transportation, and distance to health care. It is therefore challenging to combine the findings given the heterogeneity of events and there was no specific characteristic of the type of MCI associated with delays e.g., type of incident or number of casualties.
The complexity of the incident site was a significant factor associated with delayed pre-hospital intervals. This was mainly observed in major events situated in remote areas such as high slopes or where road obstructions prohibited pre-hospital provider access. Physical accessibility is a common feature in incidents occurring in remote regions. 38 Following a multi-scene transportation MCI involving difficult access and prolonged distances to trauma centers, use of air ambulance services was recommended to reduce transportation times from remote or challenging settings. Reference Assa, Landau, Barenboim and Goldstein39 Whilst HEMS services have been included in Norwegian mass casualty plans for some time, Reference Johnsen, Samdal and Sollid40 a recent systematic review reported that air-medical services units are not consistently included in MCI plans, even those with logistical and geographical challenges, and decisions are generally made on a case-by-case basis. Reference Johnsen, Fattah and Sollid41 The high cost of HEMS may also prohibit their use in low-income countries or very remote regions.
Scene safety and security considerations had a significant impact on triage delays in this review, which led to prolonged transportation times to definitive care. Reports of MCIs involving mass casualty shootings highlight the risks to responders, the need for safe inner cordon interventions and support for lower-level hospitals who may be required to admit casualties if access to higher level facilities is restricted. Reference Turner, Lockey and Rehn42,Reference Wild, Maher and Frazee43 Safety issues at incident scenes rely on police enforcement to secure the area as quickly as possible, yet this may be challenging in some settings. The most effective solution might come from an integrated response within MCI plans, involving police jurisdictions, EMS, and fire departments. Reference Reeping, Jacoby and Rajan44
Adverse triage responses were also associated with longer times to definitive care. Rapidly sorting several victims and identifying a priority for care is fraught with difficulty during unpredictable accidents. Reference Turner, Lockey and Rehn42 Misclassification, i.e., incorrect triage level, is associated with significant delays for critically injured patients. Reference Wild, Maher and Frazee43,Reference Reeping, Jacoby and Rajan44 Where EMS providers followed the “To see is to send” policy despite triage decisions, this conflicted with the ultimate goal of optimizing immediate transportation for critical patients and resulted in inappropriate distribution to facilities. This was previously described in the Virginia Tech Shootings’ findings which found that over-triaging increased the mortality of critical victims by 20%. Reference Reeping, Jacoby and Rajan44 Within this systematic review it was unclear as to why EMS triage decision-making was potentially sub-optimal. Education and training may help to increase knowledge and confidence, resulting in improved triage decision-making. Reference Reeping, Jacoby and Rajan44 Simulated flow models may also help to identify the effects of decision-making in response to an MCI, in a safe, large-scale environment. Reference Wang, Luangkesorn and Shuman45
Limitations
This review has several limitations. First, the eligibility criteria were limited only to evidence in English, and excluded non-English papers may have provided other information on factors which impact PHT in an MCI. Second, PHTs in the studies were reported variably, and some did not measure this period for all injured patients. We are therefore unable to discuss all potential confounders or factors affecting PHT. Lastly, existing quality assessment tools were not relevant to this review due to the nature of the topic, therefore, we had to adapt current tools to assess quality in the included studies.
Conclusion
This systematic review revealed that MCIs were heterogenous in nature and PHTs were significantly varied. Currently, most published MCIs have a PHT of 2 hours or longer. The incident location and scene safety are associated in delayed PHT. Adverse MCI triage decisions appear to have challenged responders resulting in longer PHTs. Future studies should focus on how MCI planning can mitigate the causes of pre-hospital delays.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/dmp.2023.187
Acknowledgements
The primary author would like to thank Professor Tim Harris and Dr. Zane Perkins for their feedback and contributions to this systematic review.
Author contribution
The review protocol was developed by FA and revised by EC. FA and EKA performed the literature search, data extraction, and quality assessment. FA analyzed and interpreted the results. FA wrote the paper and EC revised the drafted manuscript. KB was involved in the critical revision of the manuscript. All authors reviewed and approved the final draft.
Funding statement
Saudi Arabia Cultural Bureau in London funds Mr. Alruqi’s PhD study and this review is part of his PhD thesis.
Competing interests
The authors declare no conflicts of interest.
Abbreviations
EMS, Emergency Medical Services; HEMS, Helicopter Emergency Medical Services; MCI, Mass Casualty Incident; PHT, Pre-hospital Time; PRISMA, Preferred Reporting Items for Systematic Review and Meta-Analysis; START, Simple Triage and Rapid Treatment









