Introduction
Homelessness has been recognised as a persistent public health concern since the late 1980s, with extreme health inequalities, and increased morbidity and mortality compared to housed populations (Rossi et al., Reference Rossi, Wright, Fisher and Willis1987; Hwang et al., Reference Hwang, Kirst, Chiu, Tolomiczenko, Kiss, Cowan and Levinson2009; Aldridge et al., Reference Aldridge, Story, Hwang, Nordentoft, Luchenski, Hartwell, Tweed, Lewer, Vittal Katikireddi and Hayward2017). Over the past decade, the number of homeless people has increased at an alarming rate in almost all European countries (FEANTSA 2018). In France, 3.5 million people are considered precariously housed and 141 500 homeless, a number which has increased by 44% over the past decade (Mordier, Reference Mordier2016). Estimates hold that 31% of persons who are homeless have at least one severe mental illness (SMI) or/and addiction (high-need subpopulation) and that psychotic disorders are 8–10 times higher in that population than in the general population (Fazel et al., Reference Fazel, Geddes and Kushel2014; Laporte et al., Reference Laporte, Vandentorren, Detrez, Douay, Le Strat, Le Mener and Chauvin2018). Studies from several settings have shown that people who are homeless use more psychiatric services (mainly emergency units) and less outpatient mental health services, with higher discontinuation rates (McNiel and Binder, Reference McNiel and Binder2005; Doran et al., Reference Doran, Ragins, Iacomacci, Cunningham, Jubanyik and Jenq2013; Russolillo et al., Reference Russolillo, Moniruzzaman, Parpouchi, Currie and Somers2016; Stenius-Ayoade et al., Reference Stenius-Ayoade, Haaramo, Erkkila, Marola, Nousiainen, Wahlbeck and Erikson2017).
Historically, dedicated homeless-specific services are based on a step-by-step approach, i.e. requiring substance abstinence, rule compliance and absence of behavioural disorder to move from emergency shelter to transitional accommodation, and then on to supportive housing (MNASM , 2007; Velpry, Reference Velpry2009). Because the focus of the facility-based programs is on treatment, not on long-term housing, these models are called ‘treatment first’ (Carling, Reference Carling1993). Among other drawbacks, this approach has been shown to fail people with SMI, who often have difficulty moving on from supported accommodation; recovery-oriented practices may help people in this category (Killaspy et al., Reference Killaspy, Priebe, McPherson, Zenasni, Greenberg, McCrone, Dowling, Harrison, Krotofil, Dalton-Locke, McGranahan, Arbuthnott, Curtis, Leavey, Shepherd, Eldridge and King2019). An integrated medical and social program called Housing First (HF) for homeless people with chronic conditions has been trialled in North America and Europe. In contrast to the ‘treatment first’ approach, HF combines rapid access to permanent, non-abstinence-contingent ordinary housing and recovery-oriented mental health support teams (Hwang and Burns, Reference Hwang and Burns2014). HF has been evaluated in the USA and Canada in good quality randomised controlled trials (RCTs), showing interesting improvements in housing stability, but mixed results in healthcare use and limited effectiveness on recovery and quality-of-life outcomes (Rosenheck et al., Reference Rosenheck, Kasprow, Frisman and Liu-Mares2003; Sadowski et al., Reference Sadowski, Kee, VanderWeele and Buchanan2009; Stergiopoulos et al., Reference Stergiopoulos, Hwang, Gozdzik, Nisenbaum, Latimer, Rabouin, Adair, Bourque, Connelly, Frankish, Katz, Mason, Misir, O'Brien, Sareen, Schütz, Singer, Streiner, Vasiliadis and Goering2015; Woodhall-Melnik and Dunn, Reference Woodhall-Melnik and Dunn2015; Aubry et al., Reference Aubry, Goering, Veldhuizen, Adair, Bourque, Distasio, Latimer, Stergiopoulos, Somers, Streiner and Tsemberis2016).
To date, the transposability and enforceability of the results from USA and Canadian studies have never been demonstrated in Europe, including France. It is particularly essential given the importance of differing social and health-care models for programs like HF. Also, a recent review of HF model studies noted the lack of robust European data on its effectiveness (Baxter et al., Reference Baxter, Tweed, Katikireddi and Thomson2019).
The current study, named Un Chez Soi d'Abord, addresses this evidence gap, investigating the effects of the Housing First model in the French context, with France providing a quasi-universal health coverage with free mental health services, in parallel to a range of social aid and housing services. The study aimed to determine whether the Housing First program for people who are homeless with SMI improves hospital and emergency department use and is a cost-effective program. In the present study we also evaluate the effectiveness of the French HF program on housing stability, recovery and quality of life.
Methods
Study design and population
Un Chez Soi d'Abord was a RCT involving homeless adults with SMI from four French cities: Paris, Marseille, Toulouse and Lille.
Participants were recruited from homelessness shelters, mobile outreach teams, community mental health teams, hospitals and prisons. Trained research assistants and a psychiatrist at each site checked eligibility criteria within 24 h of referral. Eligible study patients were over 18 years old, absolutely homeless (no fixed place to stay for at least the previous seven nights, with little likelihood of finding a place in the upcoming month) or precariously housed (housed in a night shelter or homeless hostel as a primary residence AND with history of two or more episodes of being absolutely homeless in the past year OR one episode of being homeless for at least 4 weeks in the past year), and had a ‘high level of needs’, defined as schizophrenia (SCZ) or bipolar disorder (BD) diagnosis according to the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV-TR) (American Psychiatric Association 2000), moderate-to-severe disability according the Multnomah Community Ability Scale (score ⩽62; range 17–85) (Barker et al., Reference Barker, Barron, McFarland and Bigelow1994) and at least one of the following criteria: (i) ⩾2 hospitalisations for mental illness over the last 5 years; (ii) comorbid alcohol or substance use disorder; (iii) having been arrested or incarcerated over the previous 2 years. In addition, patients were required to be covered by French state health insurance. Exclusion criteria were the inability to provide informed consent, having dependent children or pregnancy.
Interviewers explained the procedures to all enrolled participants, obtained informed consent and confirmed study eligibility. A total of five face-to-face follow-up interviews were conducted every 6 months between baseline and 24 months. All participants received vouchers (tickets that may be exchanged for goods or services) for each interview. Details of the RCT protocol have previously been described (Tinland et al., Reference Tinland, Fortanier, Girard, Laval, Videau, Rhenter, Greacen, Falissard, Apostolidis, Lançon, Boyer and Auquier2013). All procedures were approved by the relevant institutional review boards: Ethics Committee (trial number 11.050) and the French Drug and Device Regulation Agency (trial number 2011-A00668-33) before the start of the initial survey.
Randomisation
Study participants were randomised 1:1 to the Housing First (HF) or Treatment-As-Usual (TAU) groups. Randomisation was stratified by site and a computer-generated randomised list was created using a permuted block design (block size: 10).
Sample size
The sample size calculation was conducted based on an absolute difference of 20% in the use of healthcare services (reference points = 3.6 for the number of hospitalisations and 5.7 for the number of ED visits) at 24 months between both groups (Sadowski et al., Reference Sadowski, Kee, VanderWeele and Buchanan2009). We estimated a minimal sample size of 600 patients using a two-tailed alpha risk of 5%, a 90% power and estimating 20% of patients lost to follow-up (Tinland et al., Reference Tinland, Fortanier, Girard, Laval, Videau, Rhenter, Greacen, Falissard, Apostolidis, Lançon, Boyer and Auquier2013).
Interventions
In the HF group, participants were offered scattered housing after their inclusion. They had some choice in the location and type of housing. They paid a maximum of 30% of their income as rent, depending on their resources, with the rest paid by the program (through the rent intermediation system). Individuals were firstly subtenants of their flat, becoming thereafter tenants through a lease transfer when they had sufficient resources. According to the HF model for a high level of needs, the multidisciplinary accompaniment teams (social worker, nurse, doctor, psychiatrist and peer worker) followed an Assertive Community Treatment (ACT) model (Lehman et al., Reference Lehman, Dixon, Hoch, Deforge, Kernan and Frank1999; Vanderlip et al., Reference Vanderlip, Williams, Fiedorowicz and Katon2014), with a recovery-oriented approach. A 10:1 client-staff ratio was operated. Participants were provided with at least one weekly visit at home or in the city at times convenient to them. Compliance with the recommendations for implementing the HF model of the US authors was verified at each stage using the HF Model fidelity scale (Gilmer et al., Reference Gilmer, Stefancic, Henwood and Ettner2015; Estecahandy Reference Estecahandy2018).
In the TAU group, homeless individuals received usual care, namely pre-existing dedicated homeless-targeted programs and services, including but not limited to outreach teams, shelters and day-care facilities. Existing TAU services in France are numerous but heavily compartmentalised between housing and health services. In addition the French TAU's system for social integration does not offer direct access to housing. These standard services mostly use a graduated approach where access to transitional housing is conditional on sobriety and psychiatric treatment compliance.
Outcomes
Primary outcomes and main secondary outcome
The primary outcomes were measured by emergency department (ED) visits, hospitalisations and inpatient days during the 24-month period.
The total costs were measured by investment costs in the HF program and the costs associated with the use of health, justice and social services over the 24-month study period. Those costs included ED visits, hospital admissions and length-of-stay, physician consultations, court appearances, days in detention and penitentiary centres, in residential structures (emergency shelters, long-term shelters and supported accommodation) and received welfare benefits. Resource use was self-reported every 6 months. The cost of the HF program included the share of the housing subsidies (i.e. €18/day v. 16/day for standard rent intermediation system in the social sector) and the share of ACT team. online Supplementary Table S1 provides detailed unit costs. A flat-rate estimate was considered in the analysis, reflecting the budget line allocated by French institutions to the HF experimentation over 2 years. Unit costs were estimated using data from the Organic Law on Finance, the French Ministry of justice and Health Ministries' hospital reimbursement reports and National tariffs (2016).
Secondary outcomes
– Housing stability: defined as the number of days in an independent house or flat, with (sub-) tenancy rights except those from the ETHOS classification (FEANTSA 2007), (online Supplementary Table S2), determined using a residential time-line follow-back calendar. Total number of days stably housed over 2 years was assessed (range: 0–730 days).
– Recovery: defined broadly as rehabilitation and growth after an illness and assessed using the Recovery Assessment Scale (RAS) (Girard et al., Reference Girard, Tinland, Mohamed, Boyer and Auquier2015). This self-administered instrument comprises 24 items, exploring five domains: personal confidence and hope, willingness to ask for help, goal and success orientation, reliance on others and no domination by symptoms, with each domain score having a specific range. An index is calculated (range: 0–100), with higher values indicating better recovery (see online Supplementary Table S3).
– Mental health symptoms during the previous month: assessed using the Modified Colorado Symptom Index (MCSI) (Conrad et al., Reference Conrad, Yagelka, Matters, Rich, Williams and Buchanan2001). The MCSI contains 14 items which evaluate how often in the past month an individual experienced a variety of mental health symptoms, including loneliness, depression, anxiety and paranoia. A higher score indicates more self-perceived symptoms (range: 14–70).
– Adherence: assessed with the Medication Adherence Rating Scale (MARS) (Thompson et al., Reference Thompson, Kulkarni and Sergejew2000). It consists of a 10-item, multidimensional, self-reporting instrument describing three dimensions: ‘medication adherence behavior’, ‘attitude toward taking medication’ and ‘negative side-effects and attitudes to psychotropic medication’. For each dimension a score is calculated. A global score is also produced, with a higher score indicating better adherence (range: 0–10).
– Quality of life (QoL) was assessed using the Schizophrenia-QoL 18 (S-QoL 18) (Boyer et al., Reference Boyer, Simeoni, Loundou, D'Amato, Reine, Lancon and Auquier2010; Girard et al., Reference Girard, Tinland, Bonin, Olive, Poule, Lancon, Apostolidis, Rowe, Greacen and Simeoni2017) and a generic QoL questionnaire, the Medical Outcomes Study 36-item Short Form Health Survey (SF-36) (Ware and Sherbourne, Reference Ware and Sherbourne1992; Leplege et al., Reference Leplege, Mesbah and Marquis1995). The S-QoL 18 is a validated self-reporting questionnaire for homeless subjects with mental disorders and comprises 18 items describing eight dimensions: psychological well-being, self-esteem, family relationships, relationship with friends, resilience, physical well-being, autonomy and sentimental life. It also generates a global index, which ranges from 0 to 100, with higher values indicating better QoL. The SF-36 is a self-administered questionnaire consisting of 36 items describing eight dimensions: physical functioning, social functioning, role-physical problems, role-emotional problems, mental health, vitality, bodily pain and general health. Two composite scores can be calculated: the physical composite score (PCS) and the mental composite (MCS) score, ranging from 0 (lowest QoL) to 100 (highest QoL).
– Substance and alcohol dependence, using sections K and J of the Mini International Neuropsychiatric Interview (MINI) (Sheehan et al., Reference Sheehan, Lecrubier, Sheehan, Amorim, Janavs, Weiller, Hergueta, Baker and Dunbar1998). The MINI is an abbreviated, structured diagnostic interview that determines the presence or absence of diagnoses of dependence on and/or abuse of alcohol and/or more frequently used or more problematic drugs and whether the diagnosis is current (preceding 12 months) and/or a lifetime diagnosis (anytime in life – may or may not be current).
Online Supplementary Table S3 provides details of internal consistency for each measure.
Outcomes were assessed every 6 months (M0, M6, M12, M18 and M24), except substance and alcohol dependence (only M12 and M24).
Statistical methods
All analyses were performed on an intent-to-treat basis. Statistical methods were employed for missing data according to their potential impact depending on nature and frequencies (Sterne et al., Reference Sterne, White, Carlin, Spratt, Royston, Kenward, Wood and Carpenter2009). Missing data were addressed using multiple imputations (see Methods S1 for details). Imputation models were implemented using MICE by chained equations and mitools R packages. In a sensitivity analysis, the multiple imputation approach was compared to existing methods for handling missing data (complete case analysis, ‘Last observation carried forward’ (LOCF), imputed data using the mean and the worse-case scenario). Statistical analysis was performed using SPSS 12 for Windows (SPSS Inc., IBM, NY, USA) and RStudio version 3.2.1 (RStudio, Inc., Massachusetts, USA).
Descriptive analyses for primary outcomes were presented as means and standard errors (SE). We employed generalised estimating equations (GEE – GENLIN function) to test for treatment differences among the primary outcomes. We choose a negative binomial distribution with a link log after having tested different distributions for skewed and over dispersed data. A random effect (for clustering) was included to adjust standard errors for the non-independence of observations within participants (cluster parameter = ‘site’). Exponentiation of the raw regression coefficients gave the corresponding risk ratio (RR). We also provided 95% CIs and adjusted p-values for multiple comparisons (Benjamini and Hochberg, Reference Benjamini and Hochberg1995). In addition, an interaction term between the treatment group and sites was considered. For secondary outcomes, a GEE model was used for total costs (count variables). Mixed linear models (MIXED) over time for repeated-measure analyses were applied for all other variables, with a repeated variable (ln(t + 1) where t is the time from baseline) and a random effect (site). Effect sizes were assessed using the coefficient of interaction term between the group and time (difference in slopes between the two groups): if statistically significant, the interaction implied the trajectory of improvement over time was better with HF than with TAU. For alcohol and substance dependency, a binomial distribution was fitted.
In a sensitivity analysis, we investigated the effect of using the data from all patients or from those with complete data.
Results
Overall, 779 homeless people were addressed by outreach teams, 717 eligible, of whom 703 agreed to participate and were randomised from August 2011 to April 2014: 353 assigned to the HF group and 350 to the TAU group (Fig. 1). Of these, 5.1% of patients withdrew from the study. Over the study period, 255(78%) HF participants v. 197(63%) TAU participants completed the study, while 34 known deaths were recorded (23 (6.5%) in HF group v. 11 (3.1%) in TAU group; p = 0.056).

Fig. 1. Flow chart of Un Chez-Soi randomized controlled trial
Baseline characteristics were similar between treatment groups, except for housing status and alcohol dependence (Table 1). The sample comprised males (82.5%), with median age of 40 and 68% diagnosed with SCZ. The median duration of homelessness was 72 months (interquartile range: 24–144 months) (Table 1). Characteristics at baseline were compared between complete (n = 452) and incomplete (n = 251) cases at 24-month of follow-up with no significant differences found except for study group and site proportions (P < 0.005).
Table 1. Baseline characteristics of participants (N = 703)
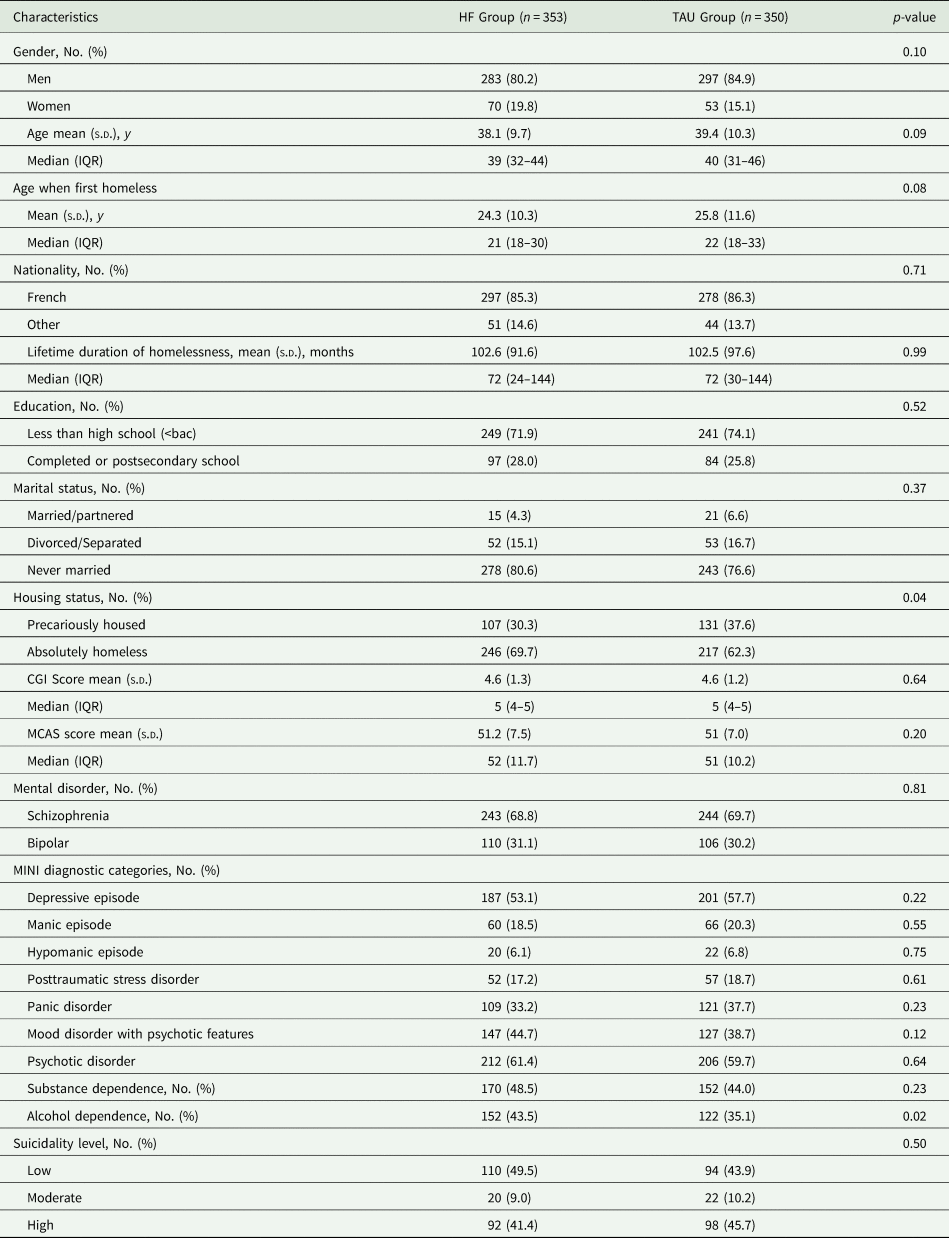
HF: Housing First; TAU: treatment-as-usual; s.d., standard deviation; IQR, interquartile range; CGI, Clinical Global Impression scale; MCAS, Multnomah Community Ability Scale; MINI, Mini International neuropsychiatric interview.
Primary outcome and main secondary outcome
On average, HF participants spent significantly less days hospitalised than TAU participants over time (51.8 days (s.e. = 5.2) v. 83.6 (s.e. = 6.9); p < 0.001) (Table 2). The RR of the number of days spent hospitalised for the HF group was 0.62 (95% CI, 0.42–0.80)). HF participants reported a similar number of hospital admissions (mean, 2.05 (s.e. = 0.1) v. 2.11 (SE = 0.2)) and ED visits over time (mean, 2.20 (s.e. = 0.2) v. 2.47 (s.e. = 0.2)). The interaction term between group and site was non-significant in each model.
Table 2. Primary outcomes at each follow up and over the 24-month period between the 353 participants in the Housing First (HF) group and 350 participants in the treatment-as-usual (TAU) group
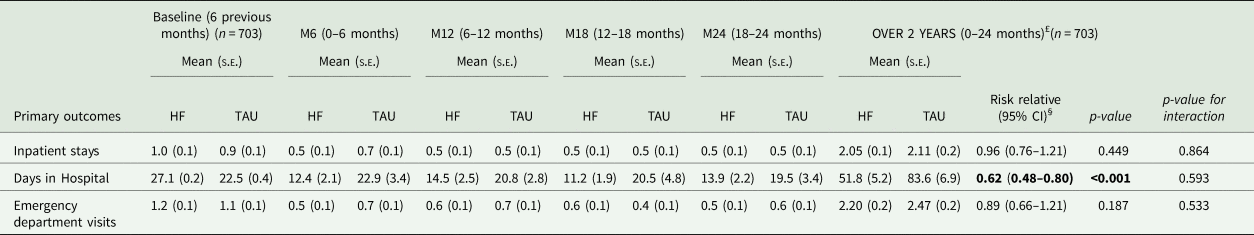
s.e., standard error. HF: Housing First; TAU: treatment-as-usual. Values in bold indicate a statistically significant difference.
£: The data set used for the imputation analysis included all randomised individuals at baseline (n = 703) minus those who withdrawn before the first follow-up or died before completed all interviews (n = 70). GEE models using a negative binomial distribution with a link log. A random effect (site, n = 4) was fitted in the model with an exchangeable covariance matrix.
§: Estimated treatment risk relative were based on the imputed-analysis set.
$: p-value for treatment × site interaction.
Compared to TAU participants, HF individuals spent 48% less on health care (mean € 29 454 v. € 47 570; RR 0.62, 95% CI, 0.48–0.78) and 93% less on standard residential services (mean €687 v. €8963; RR 0.07, 95% CI, 0.05–0.11) (Table 3). Inversely, participants from the HF group received statistically significant higher welfare benefits (RR 1.10, 95% CI, 1.03–1.17; p = 0.006). Finally, comparing the total costs, no difference was found between two groups (p = 0.141). This result suggests that the costs of Un Chez Soi d'Abord program were compensated by cost savings in health and social services.
Table 3. Mean costs per patient over the 24-month follow-up period between the 353 participants in the HF group and the 350 participants in the TAU group

HF, Housing First; TAU, treatment-as-usual; s.e., standard Error; 95% CI, 95% confidence interval.
Generalised linear models were used to address the P-value for interaction between intervention groups and site. The within-subject ‘random’ effects were modelled for each participant to adjust standard errors for the non-independence of observations within participants (cluster parameter = ‘site’; n = 4).
$: a negative binomial distribution with a link log was used.
Values in bold indicate a statistically significant difference in pooled imputation data set from the group variable (HF v. TAU groups).
a: including the cost of ACT team support and housing subsidies in the HF group. Housing subsidies (IML) included a guarantee of rent and repair of potential damages.
b: including ED visits, hospital admissions (either medical, psychiatric hospital or Nursing and long-term care facilities), Health rehabilitation residential program and therapeutic apartment, outpatient consultations (either general practitioner, psychiatrist or other specialists).
c: including Emergency shelters, Transitional shelters and other residential structures for formerly homeless people (based on individual's resources and rent subsidies (IML)).
d: including court appearances, transitional prison (awaiting for judgement or sentence of less than 2 years), detention centre (including reinsertion approach), detention centre with high level of security, and penitentiary centre (mixed structure).
e: including all welfare benefits reported by the participants such as housing allowances or work subsidies (social minimum welfare benefits) as well as disability benefits for physical or mental health issues.
Secondary outcomes
The mean days stably housed improved in both groups at each time interval, while mean change from baseline to 24 months improved significantly in the HF group compared to the TAU group (difference in slopes, 116; 95% CI, 103–128) (Table 4).
Table 4. Clinical variables, recovery and quality of life from baseline to 24 months and mixed-model results through 24 months between the participants in the HF group and TAU group
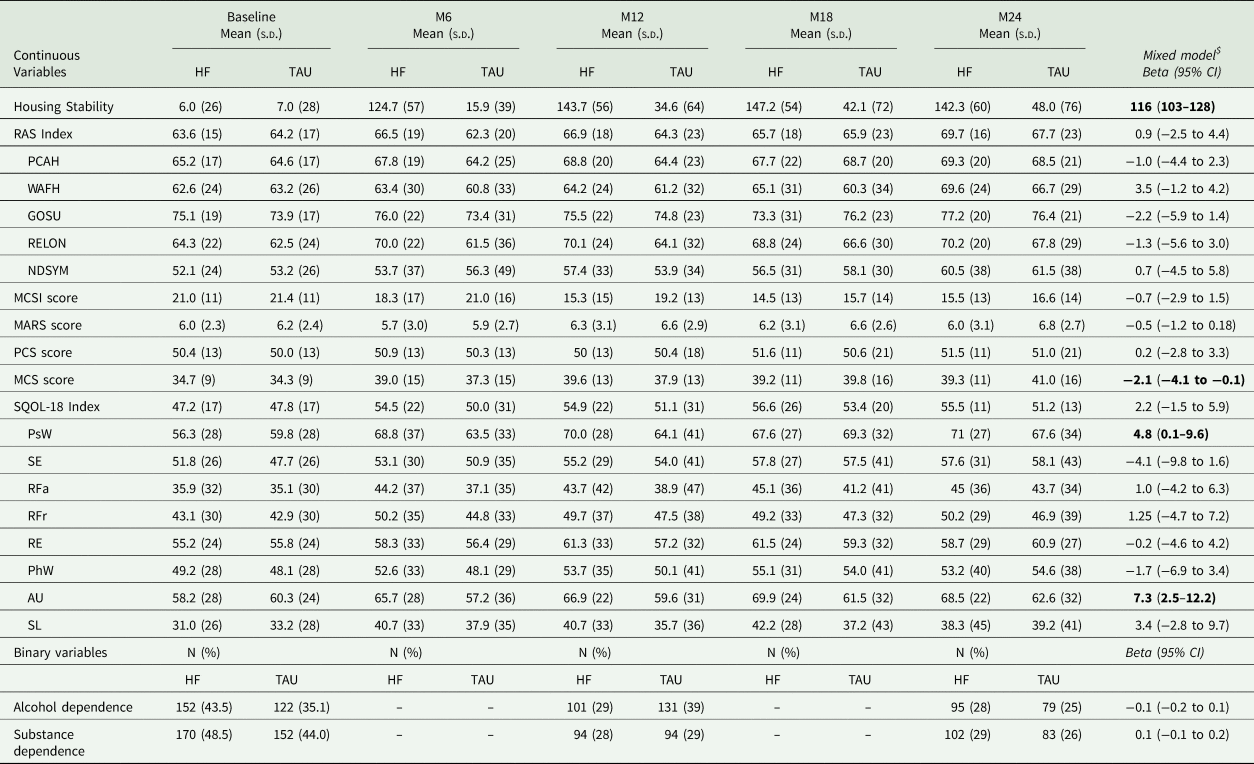
SD, standard deviation. HF, Housing First; TAU, treatment as usual; RAS, Recovery assessment scale; RAS dimensions, PCAH, Personal Confidence and Hope; WAFH, Willingness to Ask for Help; GOSU, Goal and Success Orientation; RELON, Reliance on Others; NDSYM, Not Dominated by Symptoms; MCSI, Modified Colorado symptom index; MARS, Medication Adherence Rating Scale; PCS, Physical composite score; MCS, Mental composite score; S-QoL, Schizophrenia Quality of Life Questionnaire; S-QoL dimensions, PsW, psychological well-being; SE, self-esteem; RFa, family relationships; RFr, relationships with friends; RE, resilience; PhW, physical well-being; AU, autonomy; and SL, sentimental life.
$: Mixed linear models (MIXED) for repeated-measure analyses were applied, using a restricted maximum likelihood approach for variance estimation, with a repeated variable (ln(t + 1) where t is the time from baseline and random effect (site, n = 4). The effect size was assessed by using the beta of the treatment × time interaction (difference in slopes between the two groups). For all models, an unstructured covariance matrix for repeated measures was used. Interactions between intervention groups and covariates (age when first homeless, SCZ or BP disorder diagnosis, gender), as well as for the interaction term between intervention groups and site were tested. No interactions were kept because none achieved statistical significance.
We found no statistically significant changes within the HF and TAU groups in RAS, MCSI or MARS scores, with both groups improving scores from baseline to 24 months.
Mean changes from baseline did not differ significantly between the HF and TAU for PCS score, with only slight score changes at each point in both groups; whereas HF group participants exhibited improved MCS score compared to the TAU group (difference in slopes, −2.1; 95% CI, −4.1 to −0.1). Similarly, HF participants exhibited improved SQoL scores from baseline to 24 months on two subscales: psychological well-being (difference in slopes 4.8; 95% CI, 0.1–9.6) and autonomy (difference 7.3; 95% CI 2.5–12.2) compared to the TAU group.
We found no statistically significant differences between groups for substance and alcohol dependence; more than one-quarter of participants were still diagnosed with alcohol or substance dependency at 24 months.
The sensitivity analyses reported little impact on the results (online Supplementary Table S4); in the worst-case scenario, results remained stable.
Discussion
This is the first randomised controlled trial on Housing First in Europe, and the first one to focus on psychotic disorders (SCZ/BP) among SMI. Our results can be summarised as follows: (i) The HF program was more effective on days spent in hospital, but no differences were detected in hospital admissions or ED visits. (ii) HF was effective for improving housing stability. (iii) HF improved some dimensions of quality-of-life, but no differences were found in other self-reported health outcomes. (iv) From an economic perspective, some discrepancies were significantly marked in cost categories: HF was associated with cost savings through decreased inpatient care and homeless residential facility use, whereas welfare benefits increasing in the HF group and costs of justice were well balanced between two groups. Overall costs were not significantly different between groups.
In the present study, the initial lengthy hospitalisation duration (including psychiatric hospitals), combined with its sharp fall over the 2 years in the HF group, explains the majority of the cost savings, with overall cost offsets representing 100% of the French program costs. For reference, in the most comparable arm of the Canadian RCT (sub-group of high needs), Aubry and colleagues reported cost savings representing 96% (Aubry et al., Reference Aubry, Goering, Veldhuizen, Adair, Bourque, Distasio, Latimer, Stergiopoulos, Somers, Streiner and Tsemberis2016). The reduction in time spent hospitalised found in our study is consistent with previous studies (Sadowski et al., Reference Sadowski, Kee, VanderWeele and Buchanan2009; Stergiopoulos et al., Reference Stergiopoulos, Hwang, Gozdzik, Nisenbaum, Latimer, Rabouin, Adair, Bourque, Connelly, Frankish, Katz, Mason, Misir, O'Brien, Sareen, Schütz, Singer, Streiner, Vasiliadis and Goering2015; Aubry et al., Reference Aubry, Goering, Veldhuizen, Adair, Bourque, Distasio, Latimer, Stergiopoulos, Somers, Streiner and Tsemberis2016) although the intensity of reduction was less. Indeed, these latter RCTs were performed in countries where deinstitutionalisation is more widespread: in the USA, with average 0.21 psychiatric beds per 1000 people (with huge state by state variation) and in Canada with 0.35 beds per 1000 people; whereas the hospital bed ratio to population is higher in France, with 0.86 per 1000 people (OECD 2015). We also did not observe a reduction in hospital admissions and ED visits. On this point it is important to note that, for the French case, the ED has become a key point of access to care for the general population as well, with an increased number of patients seeking care in EDs instead of their general practitioner (Durand et al., Reference Durand, Gentile, Devictor, Palazzolo, Vignally, Gerbeaux and Sambuc2011). Also homeless people are facing competing priorities such as seeking shelter, work or even food, or having issues with the legal system, which may discourage them from seeking preventive care (Gelberg et al., Reference Gelberg, Gallagher, Andersen and Koegel1997; Crawley et al., Reference Crawley, Kane, Atkinson-Plato, Hamilton, Dobson and Watson2013; White and Newman, Reference White and Newman2015). As a consequence, addressing major lifestyle changes among a population for which the ED and hospital admission have appeared to be the first-line health provider for years would probably require a longer period of follow up.
Decrease in residential service costs and increase in welfare benefits in the HF group were both linked to the effectiveness of HF in helping individuals to escape homelessness and achieve housing stability. While the present study extends previous studies with respect to housing stability (Sadowski et al., Reference Sadowski, Kee, VanderWeele and Buchanan2009; Padgett et al., Reference Padgett, Stanhope, Henwood and Stefancic2011; Palepu et al., Reference Palepu, Patterson, Moniruzzaman, Frankish and Somers2013; Henwood et al., Reference Henwood, Dichter, Tynan, Simiriglia, Boermer and Fussaro2015; Stergiopoulos et al., Reference Stergiopoulos, Hwang, Gozdzik, Nisenbaum, Latimer, Rabouin, Adair, Bourque, Connelly, Frankish, Katz, Mason, Misir, O'Brien, Sareen, Schütz, Singer, Streiner, Vasiliadis and Goering2015; Aubry et al., Reference Aubry, Goering, Veldhuizen, Adair, Bourque, Distasio, Latimer, Stergiopoulos, Somers, Streiner and Tsemberis2016), the conclusions of the increase in social benefits are substantial: access to housing has occurred simultaneously with an increase in concerns about financial resources to pay the rent over the long-term. Participants in the HF group, with the support of the team, applied for housing allowances, welfare and disability allowances. This explains the simultaneous increase in welfare benefits over the 2 years of follow up (Rhenter et al., Reference Rhenter, Moreau, Laval, Mantovani, Albisson, Suderie, Boucekine, Tinland, Loubière, Greacen, Auquier and Girard2018). Costs of justice were not impacted by the intervention due to very small sample size to capture an effect on this service use. Nonetheless, previous RCT studies also found no significant effect on this resource (Stergiopoulos et al., Reference Stergiopoulos, Hwang, Gozdzik, Nisenbaum, Latimer, Rabouin, Adair, Bourque, Connelly, Frankish, Katz, Mason, Misir, O'Brien, Sareen, Schütz, Singer, Streiner, Vasiliadis and Goering2015; Aubry et al., Reference Aubry, Goering, Veldhuizen, Adair, Bourque, Distasio, Latimer, Stergiopoulos, Somers, Streiner and Tsemberis2016).
Most of the secondary outcomes yielded no different findings. Recovery measure, self-perceived symptoms, social functioning, perceived or objective QoL, as well as addiction issues, except some of them for which we will address a specific discussion, were not altered by the HF intervention.
The main reason is the time frame of the study. On the one hand, it would be unrealistic to expect any significant improvements in 2 years in the population of people suffering from SCZ and even more in homeless schizophrenics. A 2-year follow-up period represents a time of adjustment and settling in for many homeless people with mental illness, and may be both unrepresentative of longer term outcomes and too short to observe perceived or objective improvements. On the other hand, this limitation related to the short time horizon was also found in North American studies (Rosenheck et al., Reference Rosenheck, Kasprow, Frisman and Liu-Mares2003; Aubry et al., Reference Aubry, Goering, Veldhuizen, Adair, Bourque, Distasio, Latimer, Stergiopoulos, Somers, Streiner and Tsemberis2016; Stergiopoulos et al., Reference Stergiopoulos, Mejia-Lancheros, Nisenbaum, Wang, Lachaud, O'Campo and Hwang2019). Nonetheless, it was not possible at the outset of the project and in view of its costs to set it up on a more relevant horizon of 4 or 6 years.
The only significant differences were observed in the ‘mental composite score’ and in sub-dimensions of quality of life (autonomy, psychological well-being), suggesting that HF starts with restoring a sense of self, more than improving the relational environment. We relate this result to those of Padgett, who showed in a qualitative study that HF participants acquire ontological security (constancy, daily routines, privacy and having a secure base for identity construction) (Padgett, Reference Padgett2007). For other dimensions of QoL, the HF group scores improved rapidly and markedly, though the gap narrowed over time through continued improvements in the TAU group, leaving no difference to be highlighted at 2 years.
As reported in previously-cited RCTs, the decrease in self-assessed symptoms was marked in both groups, not allowing any difference to be significantly demonstrated. Interestingly, this decrease of symptoms was not explained by increased adherence.
The absence of differences on addictive behaviours in the HF group in comparison with the TAU group is puzzling, considering mixed results on addictive disorders improvement with the HF model underlined by previous research on the basis of their design (Padgett et al., Reference Padgett, Stanhope, Henwood and Stefancic2011; Woodhall-Melnik and Dunn, Reference Woodhall-Melnik and Dunn2015; Cherner et al., Reference Cherner, Aubry, Sylvestre, Boyd and Pettey2017). The HF group was reporting a 40% reduction in dependence rates compared to baseline with no obligation to do so, which is encouraging, although the decrease in substance dependence did not occur at a higher level than the TAU group. In contrast, the reduction of addictive behaviour in the TAU group may be related to the strict prohibition of alcohol or substance consumption in most places where this group spends nights (the vast majority of shelters, medical or penal institutions), while participants may have also hidden addictive activity because it was forbidden. HF teams practice a harm reduction approach, aiming to minimizing risks even if the person remains addicted (Tsemberis et al., Reference Tsemberis, Gulcur and Nakae2004). Other hypotheses concern the lack of training of HF French teams in addictology. For the decision makers or professionals who would like to implement the HF program in their own locations, addictology skills should exist within the HF teams so that people included in the program can be better taken care of on this issue. Additional studies should further explore this issue.
Finally, the mortality results are concerning. We conducted a retrospective search of any proof of life or death among family and friends, social and medical institutions, and administrative databases, by linking participants to their provincial death registry when possible (a non-negligible proportion of the participants were born in a foreign country). The question remained open whether or not the difference in mortality between TAU and HF groups was due to the higher proportion of participants in the TAU group whose vital status was uncertain (9.5% v. 0.6%).
Regarding the generalisability of our results, these most immediately apply to the French population of homeless people with SCZ/BP disorders. Although the ratio SCZ/BP did not differ between the HF and TAU groups, future research could focus on the effectiveness of HF in subgroups with severe psychotic disorders and identify ways to improve strategies.
More broadly, these findings may help the process of supporting expansion of HF programs in other countries, notably European countries where similarities in health care systems may be observed, with either universal health care or a strong publicly funded health care option.
This study displays some limitations. Firstly, HF is a complex intervention that contains several interacting components and our design does not enable examination of individual elements of the intervention. Secondly, a longer-term follow-up may help to support morbidity, quality of life and recovery outcomes. A Canadian study over a 4 years of follow-up showed encouraging results (Stergiopoulos et al., Reference Stergiopoulos, Mejia-Lancheros, Nisenbaum, Wang, Lachaud, O'Campo and Hwang2019). In Europe, a more extended follow-up, over 6 years, would be appreciated to address long-term impacts of HF programs. Thirdly, our study was based on interviews. Using self-reported outcomes could be seen as a problem when assessing symptoms or addiction troubles, and even more when collecting data on healthcare use. The measure of self-reported healthcare use has been shown to be reliable in homeless people with mental illness (Hwang et al., Reference Hwang, Chambers and Katic2016; Somers et al., Reference Somers, Moniruzzaman, Currie, Rezansoff, Russolillo and Parpouchi2016), and tools measuring the users' subjective perspective were deliberately chosen as indicators. Finally, we did not report indirect costs (productivity gains) in the present cost analysis. A complementary study addressing the cost-effectiveness of HF will be published and includes a full evaluation of direct and indirect costs, with housing stability as the effectiveness measure and using a Markov model over the lifetime horizon.
The coalition between researchers, advocates and the government has enabled this study to achieve a high social impact. These findings are in the process of supporting expansion of HF programs (from four to 20 cities in France), which is enshrined in the Organic Law on Social Security and funded by Social Security. Similarly, these findings support the French 5-year government plan called ‘housing and homelessness strategies’, which promotes the ‘Housing First’ approach. This kind of research policy holds that knowledge shapes policy (Boswell and Smith Reference Boswell and Smith2017) and was unprecedented in France.
In conclusion, among homeless people suffering from severe mental illness, the HF model combining immediate access to housing and the support of an ACT team seems to be effective in reducing time spent in hospital, in achieving housing stability and is a cost-saving intervention relative to existing practices.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S2045796020000785
Data
Not all the data are freely accessible because no informed consent was given by the participants for open data sharing, but we can provide the data used in this study to researchers who want to use them, following approval by the ethics committee of the Aix Marseille University.
Acknowledgements
We would like to thank the hundreds of people who agreed to take part in the survey. We are also indebted to the field research team members. Specifically, we wish to thank: Coralie Lemoine, El-had Mohammed, Amandine Albisson, Pierre Allenou, Karine Baumstarck, Emma Beetlestone, Julien Billard, Philippe Birmes, Raphaël Bouloudnine, Emmanuelle Bourlier, Thomas Bosetti, Jean-Marc Colucci, Thierry Danel, Jacques Debieve, Achille Djiena, David Flahaut, Cécile Fortanier, Géraldine Guétière, Pascale Hérédia-Rodier, Emmanuelle Jouet, Patrick Le Cardinal, Jean-Marc Legagneux, Emilie Labeyrie, Jean Mantovani, Alain Mercuel, Delphine Moreau, Jean Naudin, Fanny Olive, Stefano Rampa, Elodie Requier, Jean-Luc Roelandt, Eglantine Simonnet, Guillaume Suderie, Aurélien Troisoeufs, Pierre-Pascal Vandini, René Wulfman, and Thomas Gesmond. We thank Owen Taylor for the English grammar correction of the manuscript. Special thanks go to the Dihal: Délégation interministérielle à l'habitation et au logement and Dr Pascale Estecahandy. In addition, we would like to thank members of the Canadian At Home/Chez Soi team for their help and advice in developing the French Housing First program: Paula Goering, Jean-Pierre Bonin, Cécile Leclerc, Eric Latimer and Sonia Coté, as well as Tim Aubry.
The authors alone are responsible for the findings.
Financial support
This work was funded by institutional grants from the 2011 Programme Hospitalier de Recherche Clinique National (PA, grant number PHRC/DGOS/PF4/2010/24.02), the French Ministry of Health (Direction Générale de la Santé), the Fondation de France and Janssen Pharmaceutical Company. The funding sources had no role in the design or conduct of the study, collection, analysis or interpretation of the data, preparation, review or approval of the manuscript or the decision to submit the manuscript for publication.
The sponsor was represented by Assistance Publique, Hôpitaux de Marseille (AP-HM), France.
Conflict of interest
All the authors have no conflicts of interest relating to this study.
Ethical standards
The French ethics committee (Comité de Protection des Personnes Sud-Méditerranée V, France: trial number 11.050) and the French Drug and Device Regulation Agency (trial number 2011-A00668-33) approved this study.
French Housing First Study Group (non-author collaborators)
Thémis Apostolidis, Philippe Birmes, Thomas Bosetti, Raphael Bouloudnine, Jacques Debieve, Bruno Falissard, Tim Greacen, Christophe Lancon, Patrick Le Cardinal, J. Mantovani, Delphine Moreau, Jean Naudin, Benjamin Videau and Anderson Loundou.






