Impact statement
Marginalised populations – including persons who are socio-economically disadvantaged, migrants and members of ethno-racial minorities, experience homelessness – have taken an important public health toll because of the COVID-19 epidemic. In particular, they seem to have especially high levels of symptoms of anxiety and depression, which deserve special attention from health professionals and public health decision makers. There are potentially effective interventions that can help target marginalised groups and should be made widely available to limit the mental health burden in this group.
Social media summary
Marginalized groups are at higher risk of experiencing mental health difficulties in the aftermath of the COVID-19 pandemic, yet few interventions have been shown to be effective in these populations.
Background
Since the end of 2019, the COVID-19 pandemic has had detrimental consequences worldwide in terms of morbidity and mortality, has weakened healthcare systems and has led to the implementation of preventive measures which were disruptive in terms of social and economic life including lockdowns, workplace and school closing as well as other restrictions in daily activities (WHO, 2020; OECD, 2021). These aspects of the COVID-19 pandemic have resulted in a significant deterioration of population mental health (Fiorillo et al., Reference Fiorillo, Sampogna, Giallonardo, Del Vecchio, Luciano, Albert and Carmassi2020; Santomauro et al., Reference Santomauro, Herrera, Shadid, Zheng, Ashbaugh, Pigott and Abbafati2021).
This situation was not entirely unexpected. Previous epidemics such as H1N1, MERS, Sars-Cov-1 and Ebola had highlighted the risk of an increase in levels of anxiety, depression and post-traumatic stress disorder (PTSD) (Park et al., Reference Park, Park, Lee, Kim, Lee, Lee and Shin2020; Zürcher et al., Reference Zürcher, Banzer, Adamus, Lehmann, Richter and Kerksieck2022), particularly among frontline healthcare workers (Chigwedere et al., Reference Chigwedere, Sadath and Kabir2021; Magnavita et al., Reference Magnavita, Chirico, Garbarino, Bragazzi, Santacroce and Zaffina2021; Yuan et al., Reference Yuan, Gong, Liu, Sun, Tian, Wang and Zhong2021). Yet, the COVID-19 pandemic had a much broader scope, and in addition to healthcare workers, women, young people as well as persons experiencing chronic mental and physical disorders have also found to be at increased risk of psychological distress, as well as of symptoms of anxiety and depression (Salari et al., Reference Salari, Hosseinian-Far, Jalali, Vaisi-Raygani, Rasoulpoor, Mohammadi, Rasoulpoor and Khaledi-Paveh2020; Chigwedere et al., Reference Chigwedere, Sadath and Kabir2021; Panchal et al., Reference Panchal, de Pablo, Franco, Moreno, Parellada, Arango and Fusar-Poli2022). Several authors have suggested that the COVID-19 pandemic should be considered as a new source of mental health trauma (Adhanom Ghebreyesus, Reference Adhanom Ghebreyesus2020; Bridgland et al., Reference Bridgland, Moeck, Green, Swain, Nayda, Matson, Hutchison and Takarangi2021). Moreover, different marginalised groups experienced particularly high increases in rates of psychiatric disorders, including persons who experience socio-economic disadvantage, the homeless, migrants and members of ethno-racial minority groups. These groups have disproportionately suffered from the direct and indirect impacts of the COVID-19 pandemic, in terms of health as well as economic and social impact (Wachtler et al., Reference Wachtler, Michalski, Nowossadeck, Diercke, Wahrendorf, Santos-Hövener, Lampert and Hoebel2020; Green et al., Reference Green, Fernandez and MacPhail2021). Moreover, inequalities in mental health exacerbated by the COVID-19 pandemic could cause further socio-economic disadvantage in the foreseeable future. Additionally, marginalised groups tend to experience difficulties in accessing standard healthcare (Wachtler et al., Reference Wachtler, Michalski, Nowossadeck, Diercke, Wahrendorf, Santos-Hövener, Lampert and Hoebel2020), which calls for innovative interventions. Prior systematic reviews and meta-analyses of the mental health impact of COVID-19 have extensively summarised findings on levels of psychological distress in the general population and among healthcare workers (Zürcher et al., Reference Zürcher, Kerksieck, Adamus, Burr, Lehmann, Huber and Richter2020; Chigwedere et al., Reference Chigwedere, Sadath and Kabir2021; Magnavita et al., Reference Magnavita, Chirico, Garbarino, Bragazzi, Santacroce and Zaffina2021; Yuan et al., Reference Yuan, Gong, Liu, Sun, Tian, Wang and Zhong2021); however, to date there was no overview of the situation among marginalised groups. There is also evidence that in-person as well as online psychosocial interventions can be effective in reducing levels of stress, anxiety, depression and insomnia exacerbated by the COVID-19 pandemic (Lekagul et al., Reference Lekagul, Piancharoen, Chattong, Suradom and Tangcharoensathien2022; Ye et al., Reference Ye, Li and Zhu2022). The aim of this literature review is to describe current evidence regarding the levels of psychological distress and psychiatric disorders among persons belonging to marginalised groups in the context of the COVID-19 pandemic, as well as promising interventions well-suited for these populations. Given the large number of studies recently published in this area and in order to analyse the most rigorous evidence, we focused our review on systematic reviews and meta-analyses.
Methods
Marginalised groups considered in this review are persons who experience socio-economic disadvantage (i.e. low income, low educational level, a low-grade occupation or unemployment), migrants and persons belonging to an ethno-racial minority group and persons who experience homelessness. Regarding interventions, we included all studies describing programmes which could mitigate the mental health impact of the COVID-19 pandemic among marginalised groups. We defined mental health outcomes as participants’ overall mental health, as well as symptoms of anxiety, depression, stress and psychological distress, which are the most frequent psychological difficulties in the general population. Additionally, we considered all interventions aiming to help persons cope with psychological distress during the COVID-19 pandemic.
To identify articles examining rates of psychological distress as well as psychiatric disorders among marginalised groups in the context of the COVID-19 pandemic, we proceeded as follows. An electronic search was subsequently conducted in Google scholar and PubMed between April 8, 2022 and May 2, 2022 to identify systematic reviews and/or meta-analyses published after March 2020. Using Boolean combinations (AND, OR, NOT), the following research terms were used: ‘COVID-19’; ‘SARS-CoV-2’; ‘coronavirus’; ‘vulnerable group’; ‘vulnerability’; ‘group at high-risk’; ‘marginalised’; ‘inequality’; ‘income loss’; ‘low-income’; ‘household income’; ‘socioeconomic disadvantaged’; ‘unemployment’; ‘homeless’; ‘people experiencing homelessness’; ‘migrant’; ‘born abroad’; ‘ethnic minority’; ‘minority’; ‘ethnic group’; ‘ethno-racial minority’; ‘mental health’; ‘mental health disorder’; ‘depression’; ‘anxiety’; ‘psychological distress’; ‘suicide’.
Due to the dearth of current reviews on mental health interventions specifically designed for/targeted at marginalised groups, we decided to broaden the scope of the search to all intervention studies aiming to reduce mental health difficulties during the COVID-19 pandemic. Specifically, the terms searched for in Google scholar and PubMed were ‘digital intervention’; ‘intervention’; ‘prevention’; ‘COVID-19’; ‘SARS-CoV-2’; ‘coronavirus’; ‘mental health’; ‘mental disorder’; ‘depression’; ‘anxiety’; ‘psychological distress’; ‘suicide’; ‘decrease’; ‘reduction’.
Studies included in our review had to fulfil the following criteria: (1) systematic review and/or meta-analysis; (2) focus on mental health outcomes or a mental health intervention; (3) inclusion of at least one of the targeted marginalised groups; (4) implementation during the period of the COVID-19 pandemic and (5) English language. The time range for the publication of the selected papers was January 1, 2020 to May 2, 2022.
Data collection
Data extraction was performed in Excel. The data extraction form relative to systematic analyses on mental health risk of marginalised groups included the following information: (1) authors; (2) journal; (3) date of publication; (4) title; (5) period covered; (6) number of articles included in the review; (7) countries; (8) study design; (9) populations studied; (10) mental health outcomes and (11) main results. Whenever possible, we also extracted p-values.
The data extraction form relative to systematic reviews of interventions aiming to reduce the impact of the COVID-19 pandemic on mental health included the following information: (1) authors, (2) journal, (3) setting, (4) characteristics of the studied population, (5) type of intervention and (6) mental health outcomes.
Results
Our search retrieved 792 studies through searching the identified databases. After removing duplicates, we screened the titles and abstracts of the remaining studies. After reading the full text of the remaining studies, 17 studies met our eligibility criteria.
Characteristics of studies describing mental health risks among marginalised populations
Overall, we identified 12 systematic reviews examining mental health difficulties in one or several marginalised groups during the COVID-19 pandemic and 5 systematic reviews on interventions that can mitigate the mental health impact of the COVID-19 pandemic. Four systematic reviews also included a meta-analysis. The number of included studies per article ranged from 15 to 294 (Table 1).
Table 1. Systematic reviews examining the mental health of marginalised groups in the context of the COVID-19 pandemic: 2020–2022
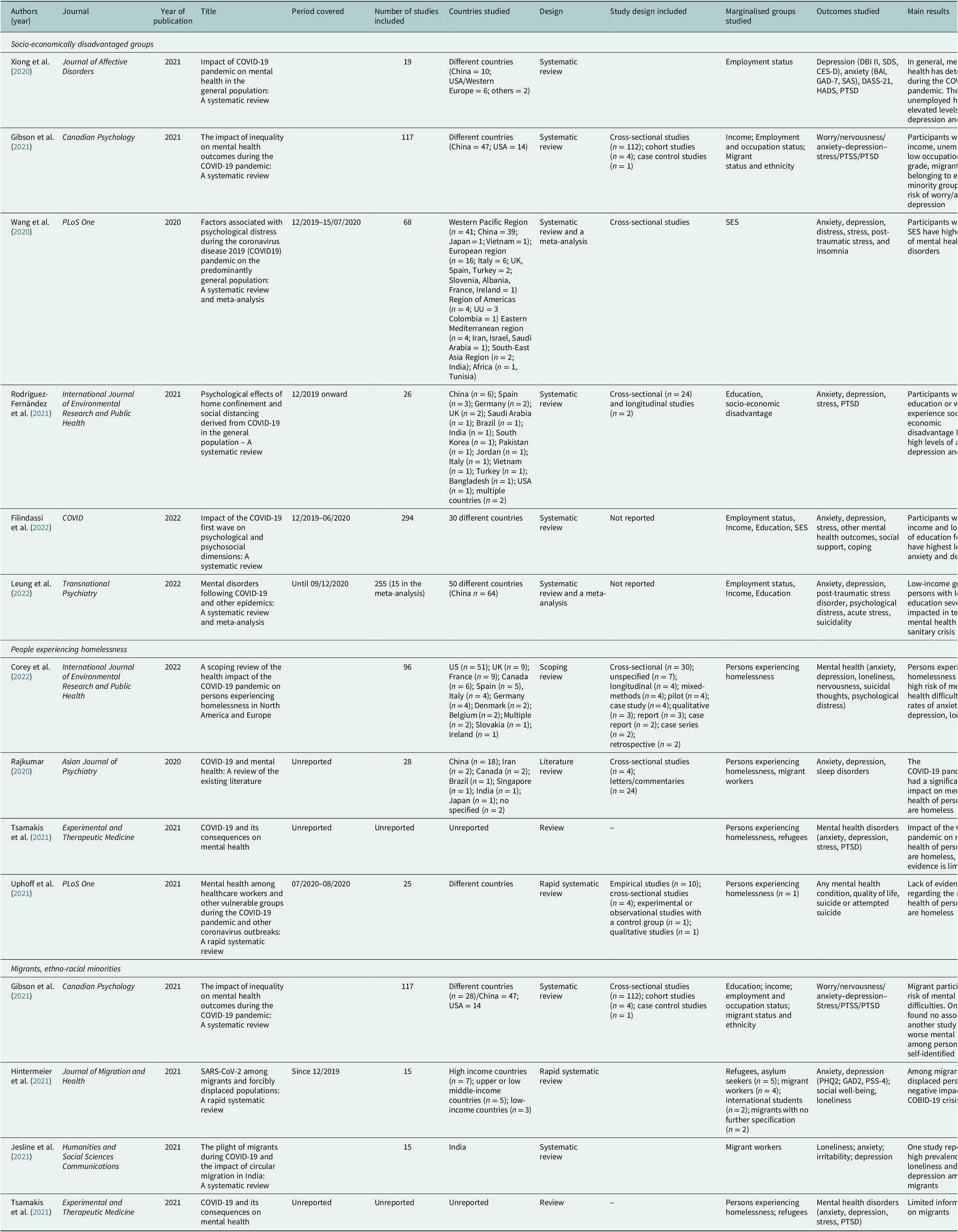
The systematic reviews we identified mainly included cross-sectional studies and were mostly based in China or Western industrialised countries (USA, UK, France, Italy and Spain). The majority of systematic reviews presented data on the targeted marginalised groups as a subgroup of the population studied, except Hintermeier et al. (Reference Hintermeier, Gencer, Kajikhina, Rohleder, Santos-Hövener, Tallarek, Spallek and Bozorgmehr2021), Jesline et al. (Reference Jesline, Romate, Rajkumar and George2021) and Corey et al. (Reference Corey, Lyons, O’Carroll, Stafford and Ivers2022) who specifically focused on persons experiencing homelessness, migrants and displaced populations.
A majority of systematic reviews explored a diversity of mental health outcomes including depression (Xiong et al., Reference Xiong, Lipsitz, Nasri, Leanna, Gill, Phan and Chen-Li2020; Wang et al., Reference Wang, Kala and Jafar2020; Gibson et al., Reference Gibson, Schneider, Talamonti and Foreshaw2021; Hintermeier et al., Reference Hintermeier, Gencer, Kajikhina, Rohleder, Santos-Hövener, Tallarek, Spallek and Bozorgmehr2021; Rodríguez-Fernández et al., Reference Rodríguez-Fernández, González-Santos, Santamaría-Peláez, Soto-Cámara, Sánchez-González and González-Bernal2021; Corey et al., Reference Corey, Lyons, O’Carroll, Stafford and Ivers2022; Filindassi et al., Reference Filindassi, Pedrini, Sabadini, Duradoni and Guazzini2022; Leung et al., Reference Leung, Ho, Bharwani, Cogo-Moreira, Wang, Mathew, Fan, Galea, Leung and Ni2022), anxiety (Xiong et al., Reference Xiong, Lipsitz, Nasri, Leanna, Gill, Phan and Chen-Li2020; Wang et al., Reference Wang, Kala and Jafar2020; Gibson et al., Reference Gibson, Schneider, Talamonti and Foreshaw2021; Hintermeier et al., Reference Hintermeier, Gencer, Kajikhina, Rohleder, Santos-Hövener, Tallarek, Spallek and Bozorgmehr2021; Jesline et al., Reference Jesline, Romate, Rajkumar and George2021; Rodríguez-Fernández et al., Reference Rodríguez-Fernández, González-Santos, Santamaría-Peláez, Soto-Cámara, Sánchez-González and González-Bernal2021; Corey et al., Reference Corey, Lyons, O’Carroll, Stafford and Ivers2022; Filindassi et al., Reference Filindassi, Pedrini, Sabadini, Duradoni and Guazzini2022; Leung et al., Reference Leung, Ho, Bharwani, Cogo-Moreira, Wang, Mathew, Fan, Galea, Leung and Ni2022), PTSD (Wang et al., Reference Wang, Kala and Jafar2020; Xiong et al., Reference Xiong, Lipsitz, Nasri, Leanna, Gill, Phan and Chen-Li2020; Gibson et al., Reference Gibson, Schneider, Talamonti and Foreshaw2021; Rodríguez-Fernández et al., Reference Rodríguez-Fernández, González-Santos, Santamaría-Peláez, Soto-Cámara, Sánchez-González and González-Bernal2021; Leung et al., Reference Leung, Ho, Bharwani, Cogo-Moreira, Wang, Mathew, Fan, Galea, Leung and Ni2022), stress (Wang et al., Reference Wang, Kala and Jafar2020; Xiong et al., Reference Xiong, Lipsitz, Nasri, Leanna, Gill, Phan and Chen-Li2020; Gibson et al., Reference Gibson, Schneider, Talamonti and Foreshaw2021; Rodríguez-Fernández et al., Reference Rodríguez-Fernández, González-Santos, Santamaría-Peláez, Soto-Cámara, Sánchez-González and González-Bernal2021; Filindassi et al., Reference Filindassi, Pedrini, Sabadini, Duradoni and Guazzini2022; Leung et al., Reference Leung, Ho, Bharwani, Cogo-Moreira, Wang, Mathew, Fan, Galea, Leung and Ni2022), suicidal thoughts (Corey et al., Reference Corey, Lyons, O’Carroll, Stafford and Ivers2022), self-harm, nervousness (Corey et al., Reference Corey, Lyons, O’Carroll, Stafford and Ivers2022; Gibson et al., Reference Gibson, Schneider, Talamonti and Foreshaw2021) and well-being (Hintermeier et al., Reference Hintermeier, Gencer, Kajikhina, Rohleder, Santos-Hövener, Tallarek, Spallek and Bozorgmehr2021; Filindassi et al., Reference Filindassi, Pedrini, Sabadini, Duradoni and Guazzini2022). All included systematic reviews presented at least two different mental health outcomes.
Most included studies relied upon participants’ self-reports of psychological distress or psychological difficulties, assessed using a variety of scales [e.g., the General Anxiety Disorder scale (GAD-7), Beck Anxiety Inventory (BAI), Patient Health Questionnaire (PHQ-9), Depression, Anxiety and Stress Scale (DASS), General Health Questionnaire (GHQ), Hospital Anxiety and Depression Scale (HADS), Perceived Stress Scale (PSS), Self-rating Depression Scale (SDS) and Self-rating Anxiety Scale (SAS)].
Persons experiencing socio-economic disadvantage
Regarding rates of mental health difficulties and psychiatric disorders among persons experiencing socio-economic disadvantage, we observed the following. Wang et al. (Reference Wang, Kala and Jafar2020) reported an elevated prevalence of anxiety [1.21 (1.05–1.40; I 2 = 86.1%)], depression [1.15 (1.03–1.29; I 2 = 82.0%)] and stress [1.15 (1.03–1.29); I 2 = 9.0%] among persons with a low educational level, compared to those with an intermediate or high educational level across 30 studies. Rodríguez-Fernández et al. (Reference Rodríguez-Fernández, González-Santos, Santamaría-Peláez, Soto-Cámara, Sánchez-González and González-Bernal2021) also found an increased prevalence of symptoms of anxiety (8.3–45.1% in five studies), depression (14.6–46.42% in seven studies), stress-related symptoms and PTSD (8.1–49.66% in four studies) among persons with a low level of education. Xiong et al. (Reference Xiong, Lipsitz, Nasri, Leanna, Gill, Phan and Chen-Li2020) found that persons with a low level of education were more likely to suffer from anxiety (ranging from 6.33% to 50.9% in 11 studies) and depression (ranging from 14.6% to 48.3% in 12 studies), compared to persons with a high level of education. However, in this systematic review, a low level of education was not associated with symptoms of PTSD. Finally, Gibson et al. (Reference Gibson, Schneider, Talamonti and Foreshaw2021), analysing 28 studies, found that a low level of education was associated with a deteriorated mental health. Conversely, the same systematic review also reported that in five studies a high level of education was associated with worse mental health outcomes and in four studies the level of education was not associated with participants’ mental health. Likewise, Filindassi et al. (Reference Filindassi, Pedrini, Sabadini, Duradoni and Guazzini2022) found a high rate of anxiety among highly educated groups in two studies. Nevertheless, stress and depression were significantly more frequent among persons with a low level of education in most studies included in this systematic review (Gibson et al., Reference Gibson, Schneider, Talamonti and Foreshaw2021; Rodríguez-Fernández et al., Reference Rodríguez-Fernández, González-Santos, Santamaría-Peláez, Soto-Cámara, Sánchez-González and González-Bernal2021; Wang et al., Reference Wang, Kala and Jafar2020; Xiong et al., Reference Xiong, Lipsitz, Nasri, Leanna, Gill, Phan and Chen-Li2020).
Similarly, six studies reported that individuals with a low income were also at increased risk of psychological distress during the COVID-19 pandemic. Wang et al. (Reference Wang, Kala and Jafar2020) suggested that members of low-income groups were more likely to suffer from anxiety [1.45 (1.24–1.69; I 2 = 82.3%)], depression [1.56 (1.26–1.92; I 2 = 85.4%)] and stress [1.27 (1.20–1.34; I 2 = 0%)] in comparison with members of higher-income groups. Gibson et al. (Reference Gibson, Schneider, Talamonti and Foreshaw2021) and Rodríguez-Fernández et al. (Reference Rodríguez-Fernández, González-Santos, Santamaría-Peláez, Soto-Cámara, Sánchez-González and González-Bernal2021) observed similar findings. Specifically, Rodríguez-Fernández et al. (Reference Rodríguez-Fernández, González-Santos, Santamaría-Peláez, Soto-Cámara, Sánchez-González and González-Bernal2021) reported elevated levels of symptoms of anxiety (in eight studies), depression (in 10 studies) and PTSD (in six studies) among persons with low income. Additionally, Filindassi et al. (Reference Filindassi, Pedrini, Sabadini, Duradoni and Guazzini2022) found higher levels of symptoms of mental distress such as anxiety (in four studies), depression and stress (in three studies) among persons with low income. Xiong et al. (Reference Xiong, Lipsitz, Nasri, Leanna, Gill, Phan and Chen-Li2020) showed a positive association between a low income and the risk of depression in two studies. Leung et al. (Reference Leung, Ho, Bharwani, Cogo-Moreira, Wang, Mathew, Fan, Galea, Leung and Ni2022) found a pooled prevalence of 13.0% of psychological distress in the general population, with persons experiencing low income being at high risk. Persons belonging to a low-income group were also at increased risk of experiencing an acute stress disorder.
Across the systematic reviews analysed, there is consensus regarding the association between unemployment and mental health problems of the context of the COVID-19 epidemic. Xiong et al. (Reference Xiong, Lipsitz, Nasri, Leanna, Gill, Phan and Chen-Li2020) reported that persons who were unemployed were at increased risk of developing depression (prevalence rates across 12 studies ranging from 14.6% to 48.3%) and stress symptoms (prevalence rates across four studies ranging from 8.1% to 81.9%). Leung et al. (Reference Leung, Ho, Bharwani, Cogo-Moreira, Wang, Mathew, Fan, Galea, Leung and Ni2022) reported prevalence rates of anxiety ranging from 14% to 32.8% (in six studies) and of depression ranging from 9.5% to 27.8% (in 12 studies) with persons who were unemployed disproportionately affected by these symptoms. Rodríguez-Fernández et al. (Reference Rodríguez-Fernández, González-Santos, Santamaría-Peláez, Soto-Cámara, Sánchez-González and González-Bernal2021) and Filindassi et al. (Reference Filindassi, Pedrini, Sabadini, Duradoni and Guazzini2022) also reported elevated levels of symptoms of anxiety, stress and psychological distress among persons who were unemployed. These results corroborate those of the meta-analysis performed by Wang et al. (Reference Wang, Kala and Jafar2020): in this analysis persons who were employed had a pooled OR of psychological distress of 0.89 (0.78–1.02; I 2 = 26.6%) in relation to those who were unemployed, highlighting a protective effect of employment. Gibson et al. (Reference Gibson, Schneider, Talamonti and Foreshaw2021) confirmed this finding. Noticeably, two studies reported by Gibson et al. (Reference Gibson, Schneider, Talamonti and Foreshaw2021) found that being on temporary leave because of the COVID-19 pandemic was more strongly associated with poor mental health than unemployment. The conclusion of Gibson et al. (Reference Gibson, Schneider, Talamonti and Foreshaw2021) contrasts with findings of others studies and indicates heterogeneity in the risk of psychological distress according to employment status.
Migrants and members of ethno-racial minority groups
Four systematic reviews examined levels of psychological distress among persons who are migrant or belong to an ethno-racial minority group, mostly suggesting an elevated risk of mental health difficulties. Gibson et al. (Reference Gibson, Schneider, Talamonti and Foreshaw2021) reported worse mental health among migrants and members of the Black, Asian and Minority Ethnic group in 10 studies. Hintermeier et al. (Reference Hintermeier, Gencer, Kajikhina, Rohleder, Santos-Hövener, Tallarek, Spallek and Bozorgmehr2021) examined five studies and reported that 73.5% of migrant workers felt anxiety, depression or perceived stress due to the COVID-19 pandemic, persons originating from South-East Asia being especially impacted. 63.3% of migrant workers reported an increase in negative thoughts, tension, frustration, irritability and fear of death. Two studies reported significantly elevated levels of distress among migrants (Hintermeier et al., Reference Hintermeier, Gencer, Kajikhina, Rohleder, Santos-Hövener, Tallarek, Spallek and Bozorgmehr2021). Tsamakis et al. (Reference Tsamakis, Tsiptsios, Ouranidis, Mueller, Schizas, Terniotis and Nikolakakis2021) suggested that deterioration in mental health among migrants arises from disadvantaged living conditions, which also contribute to an increased risk of COVID-19 infection. Similarly, Jesline et al. (Reference Jesline, Romate, Rajkumar and George2021) also suggested that precarious living conditions in migrant populations contribute to high levels of psychological difficulties experienced in this group. This marginalised population, experiencing multiple forms of social vulnerability, has elevated odds of experiencing various negative outcomes: suicidal tendencies, self-harm, loneliness, anxiety and psychological distress.
However, two studies analysed by Gibson et al. (Reference Gibson, Schneider, Talamonti and Foreshaw2021) did not report elevated rates of mental health difficulties among members of ethno-racial minority groups. Furthermore, at least one study conducted in the USA found that persons who identified as White Caucasian had higher levels of psychological disorders during the COVID-19 pandemic than those who identified as Asian or Hispanic. Although members of migrant and ethno-racial minority groups were overall at significantly higher risk of experiencing mental disorders, it is important to note that the extent to which this risk is elevated varies across different groups and settings.
People experiencing homelessness
Corey et al. (Reference Corey, Lyons, O’Carroll, Stafford and Ivers2022) conducted an exhaustive literature review regarding issues affecting persons experiencing homelessness in the context of the COVID-19 pandemic. Five original studies revealed poor mental health in this group, with a 32% and 49% prevalence of symptoms of anxiety and of feelings of loneliness, respectively. Women experiencing homelessness and unstable housing appear particularly likely to have high levels of anxiety (42%) and depression (55%) according to nine studies. Moreover, Corey et al. (Reference Corey, Lyons, O’Carroll, Stafford and Ivers2022) demonstrated that the COVID-19 pandemic induced a deterioration in the mental health of persons experiencing homelessness. Additionally, two of the included studies indicated a deterioration of mental health (39% of persons) throughout the COVID-19 pandemic and a rise in thoughts of self-harm and suicide (up to 21%). To the contrary, three studies summarised in the review conducted by Corey et al. (Reference Corey, Lyons, O’Carroll, Stafford and Ivers2022), suggested improvements in mental health and well-being among persons experiencing homelessness during the COVID-19 pandemic. These studies conducted in Italy and Ireland were performed in night shelters that provided services 24 hours a day, 7 days a week, which could have mitigated the impact of the COVID-19 pandemic. Another study, analysed by Corey et al. (Reference Corey, Lyons, O’Carroll, Stafford and Ivers2022) and conducted among persons experiencing homelessness in France, indicated that 24% had unmet mental health needs. Several barriers to care were pointed out: barriers in access as well as insufficient efficacy of telephone and online services.
Three additional reviews indicated high levels of psychological distress among persons experiencing homelessness (Rajkumar, Reference Rajkumar2020; Tsamakis et al., Reference Tsamakis, Tsiptsios, Ouranidis, Mueller, Schizas, Terniotis and Nikolakakis2021; Uphoff et al., Reference Uphoff, Lombardo, Johnston, Weeks, Rodgers, Dawson, Seymour, Kousoulis and Churchill2021).
Interventions aiming to reduce the risk of mental health difficulties in marginalised groups
Different types of tools appear to be effective in addressing individuals’ psychological needs and may be well-suited for marginalised populations in pandemic time.
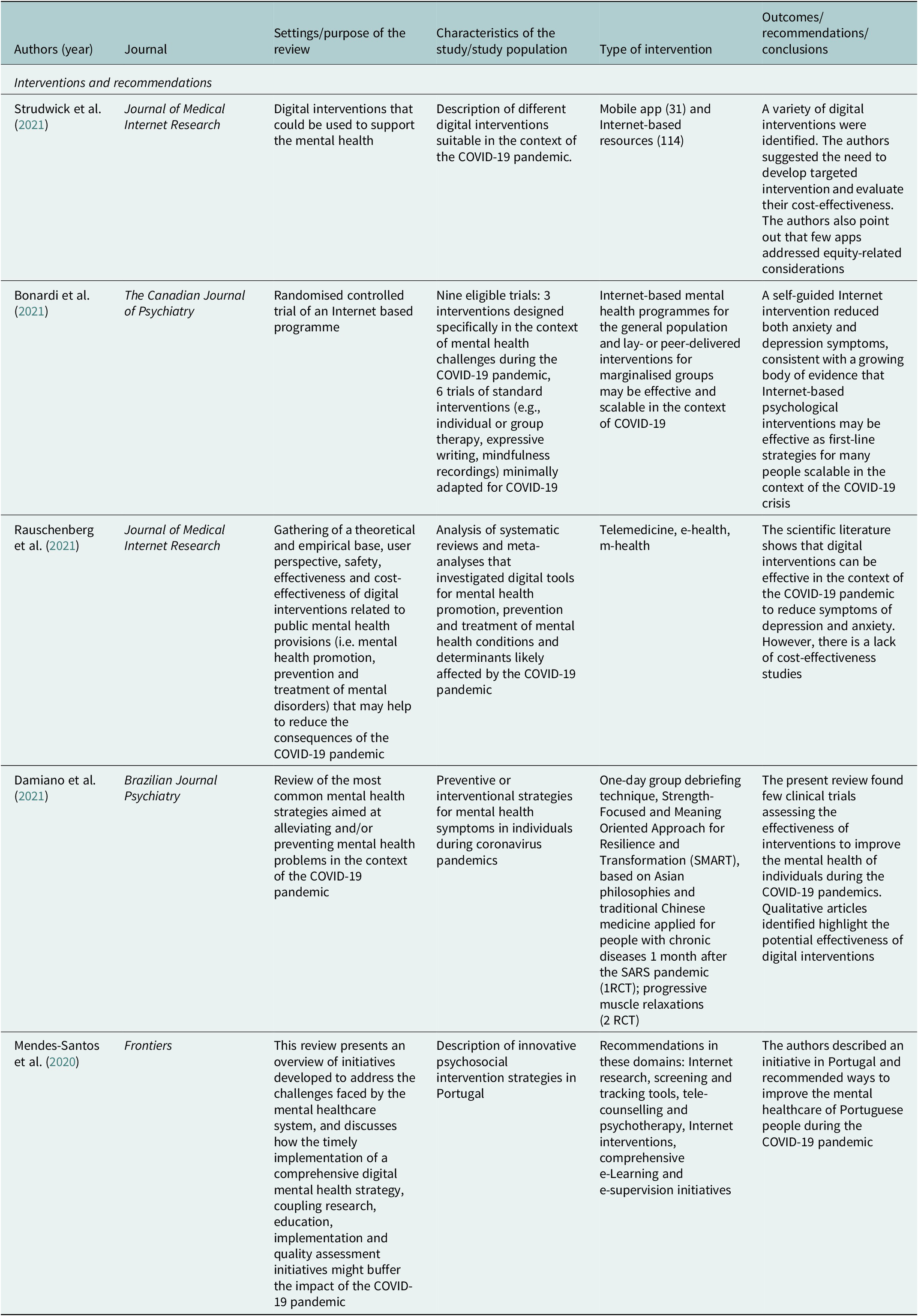
Bonardi et al. (Reference Bonardi, Wang, Li, Jiang, Krishnan, He and Sun2021) performed a review of nine randomised controlled trials (RCTs). Three were designed during the COVID-19 pandemic and included a racially and ethnically diverse sample. One trial tested the effects of a 4-week lay person-delivered intervention consisting of telephone calls to a group of homebound older adults in the USA receiving home meal services through the Meals on Wheels programme. The investigators trained university students in empathetic conversational skills (e.g., prioritising listening, eliciting conversation on topics of interest to participants) and each caller supported 6–9 participants. Calls were performed on 5 days during the first week and 2–5 days in the following 3 weeks and lasted less than 10 minutes. The study observed effects on participants’ symptoms of anxiety, depression, overall mental health and loneliness. A second trial tested the efficacy of multifaceted videoconference-based 4-week group intervention tested in 12 countries and aiming to reduce levels of anxiety, depression, fear and loneliness among persons with rare autoimmune diseases, systemic sclerosis or scleroderma. The third study showed the effect of a self-guided online cognitive behavioural intervention tested in the general population of Sweden. Regarding these three interventions, COVID-19-specific anxiety and general anxiety symptoms were reduced by a standardised mean difference (SMD) of 0.31 (95% CI 0.03–0.58) to 0.74 (95% CI 0.58–0.90) compared to no intervention or a waitlist. Depressive symptoms were also reduced [SMDs between 0.31 (95% CI 0.05–0.70) and 0.56 (95% CI 0.22–0.55)].
Damiano et al. (Reference Damiano, Di Santi, Beach, Pan, Lucchetti, Smith, Forlenza, Fricchione, Miguel and Lucchetti2021) gathered 125 qualitative studies addressing preventive or interventional strategies to improve mental health and three RCTs adapted to the context of the COVID-19 pandemic. Most involved psychological/psychiatric interventions (12.8%), technological/media interventions (7.2%) (e-health or digital or telephone-based interventions), psychological/psychiatric interventions associated with technology/media and education (5.6%), self-care (exercise, eating habits, leisure time, sleep hygiene) and governmental programmes (5.6%). Using data from three RCTs with a total of 128 participants, the meta-analysis highlighted improvements in symptoms of anxiety, depression, sleep quality, hostility and somatisation [SMD = 0.87 (95% CI 0.33–1.41), p < .001, I 2 = 69.2%]. The first trial was a 1-day group debriefing technique based on Asian philosophies and traditional Chinese medicine applied to persons who experience a chronic disease. The two other trials involved Internet-based interventions focusing on muscle and breathing relaxation for COVID-19 patients (30 minutes daily for 5 days; 2-week trial of daily 50-minute practices of breath relaxation techniques).
Rauschenberg et al. (Reference Rauschenberg, Schick, Hirjak, Seidler, Paetzold, Apfelbacher, Riedel-Heller and Reininghaus2021) and Strudwick et al. (2021) found some evidence of effectiveness of digital general public interventions, which could be used in the context of the COVID-19 pandemic. According to these authors, e-health (electronic health) and m-health (mobile health) interventions decreased levels of symptoms of common mental disorders such as anxiety and depression during the COVID-19 pandemic. Additionally, these analyses appear to be cost-effective, although the number of studies is limited. Strudwick et al. also showed evidence that digital interventions are scalable and well-suited to the COVID-19 pandemic. These interventions had a positive impact on the risk of anxiety, depression and PTSD. Notably, the authors included interventions directly designed for members of ethno-racial minority groups (3 articles) or groups experiencing socio-economic disadvantage (11 articles). The number of interventions tested in these marginalised groups is low, but this review showed the possibility of successful targeting. The key barriers to the implementation of such interventions are the difficulty to use technology, mistrust of technology or difficulty establishing a therapeutic alliance with healthcare providers due to technology-related challenges.
Discussion
This literature review summarises data on the impact of the COVID-19 pandemic on the mental health of persons belonging to marginalised groups. Indeed, socio-economic disadvantage, as measured by a low educational level, low income or unemployment, is linked with the occurrence of mental health disorders such as anxiety, depression and acute stress. Similarly, migrants and persons belonging to ethno-racial minorities or experiencing homelessness are also at increased risk of psychological distress. Regarding actions that mitigate psychological distress, we found no reviews regarding specific interventions aiming to improve mental health during COVID-19 pandemic in marginalised groups. Yet, we found evidence of interventions that can be relevant for persons who are often excluded from standard healthcare. The systematic reviews we examined point to improvements in the prevention and care of mental health difficulties among members of marginalised groups which should be the focus of future research testing innovative community-based designs.
Limitations
Our review has several limitations. First, we searched for relevant articles in PubMed and Google Scholar and may have bypassed some relevant publications. Nevertheless, Google Scholar covers multiple disciplines and fields, and it is unlikely that we missed important publications in the field. Second, the number of systematic reviews focused on the mental health of members of marginalised groups is limited, unlike healthcare workers, children, women, older people and people with pre-existing mental health disorders who have been widely studied (Sepúlveda-Loyola et al., Reference Sepúlveda-Loyola, Rodríguez-Sánchez, Pérez-Rodríguez, Ganz, Torralba, Oliveira and Rodríguez-Mañas2020; Thibaut and Van Wijngaarden-Cremers, Reference Thibaut and van Wijngaarden-Cremers2020; Vizheh et al., Reference Vizheh, Qorbani, Arzaghi, Muhidin, Javanmard and Esmaeili2020; Jones et al., Reference Jones, Mitra and Bhuiyan2021; Hards et al., Reference Hards, Loades, Higson-Sweeney, Shafran, Serafimova, Brigden and Reynolds2022). Third, there is a lack of variety among studies presented in the systematic reviews we examined. Most studies were cross-sectional, conducted online and come from industrialised countries such as China, USA or European countries. Therefore, there is need to additional high quality studies in the future. A notable systematic review performed by Jesline et al. (Reference Jesline, Romate, Rajkumar and George2021) focused on India and involved migrants, giving some information about the situation in a middle-income country. Fourth, marginalised groups were not equally represented in the scientific literature: we found few reviews dedicated to persons experiencing homelessness. Future research should take care to involve designs which make it possible to study marginalised groups which are often excluded from standard designs.
Interpretation of study findings
Our findings imply a degree of universality in the relationship between membership in a marginalised group and mental health difficulties in the context of the COVID-19 pandemic in Western countries. A relevant element, which was not discussed in the systematic reviews we analysed, is that marginalised groups may have experienced high levels of mental health difficulties prior to COVID-19 (Businelle et al., Reference Businelle, Mills, Chartier, Kendzor, Reingle and Shuval2014; Silva et al., Reference Silva, Loureiro and Cardoso2016). The COVID-19 outbreak may have exacerbated these pre-existing difficulties and highlighted the mental health needs in these high-risk groups. It is also relevant to point out that marginalised group may cumulate different forms of disadvantage (Wright et al., Reference Wright, Steptoe and Fancourt2021). For example, a study conducted by Scarlett et al. (Reference Scarlett, Davisse-Paturet, Longchamps, El Aarbaoui, Allaire, Colleville, Convence-Arulthas, Crouzet, Ducarroz and Melchior2021) shows that among persons experiencing homelessness, being unemployed was associated with the likelihood of depression alongside migrant status.
Interestingly, the COVID-19 pandemic led to unprecedented levels of resources for research on mental health. For example, the European Preparedness of health systems to reduce mental health and psychosocial concerns resulting from the COVID-19 pandemic (the RESPOND project) aims to identify vulnerable groups at highest risk of mental health problems and test an innovative stepped care intervention programme (Self-Help Plus and Problem-Management Plus developed by the World Health Organisation). The RESPOND project also examines the cost-effectiveness of this programme to identify effective strategies to improve health system preparedness in the event of a future pandemic (RESPOND Project, 2022). The RESPOND project aims to answer to several issues raised in this review: the need for screening tools which make it possible to identify groups at risk of suffering of psychological issues and the ways of addressing them, as indicated by Mendes-Santos et al. (Reference Mendes-Santos, Andersson, Weiderpass and Santana2020); the necessity to test the use of digital and in-person psychosocial support interventions, as pointed out by Rauschenberg et al. (Reference Rauschenberg, Schick, Hirjak, Seidler, Paetzold, Apfelbacher, Riedel-Heller and Reininghaus2021). The intervention being tested in the context of the RESPOND trial may be well-suited for populations who are marginalised and have difficulty accessing mental healthcare, and this aspect will be specifically examined. Finally, our literature review reveals the lack of data on marginalised populations in low- and middle-income countries, and the need for additional research in these settings (Table 2).
Table 2. Interventions aiming to address mental health needs in the context of COVID-19 suitable for marginalised groups
Nevertheless, despite existing gaps in knowledge, several recommendations can be made to healthcare professionals, on the basis on our findings as well as existing literature. First, given the increase in mental health problems and special vulnerability identified among persons who experience socio-economic disadvantage, homelessness or who are migrant, screening for symptoms of anxiety and depression in these groups should be disseminated as much as possible. Second, given difficulties in access to mental healthcare among members of socio-economically marginalised groups, there is need to develop innovative interventions to prevent but also address symptoms of anxiety and depression, are cost-effective and can be widely disseminated (Stewart and Appelbaum, Reference Stewart and Appelbaum2020). In the aftermath of the COVID-19 pandemic, when the economic consequences start being evaluated, mental health professionals also need to be present on the public scene and in face of decision makers to indicate that even if the number of COVID-19 infections and death have decreased, the psychiatric consequences are far from over, particularly among marginalised groups, and will require budgetary and personnel commitments to be addressed (McDaid, Reference McDaid2021).
Conclusion
The mental health of marginalised groups was severely affected during the COVID-19 pandemic. Symptoms of mental health disorders reported and studied predominantly included anxiety, depression and stress. Public authorities should be aware of the role of socio-economic disadvantage, being a migrant, being a minority and/or being homeless with regard to poor mental health, especially during a pandemic such as COVID-19. This should alert healthcare providers and policy makers as to the need regarding specific support required by these groups. Mental health interventions should also better target these marginalised groups in order to mitigate psychological distress. Indeed, interventions mitigating mental health distress in times of crisis exist and should be developed and rendered appropriate to marginalised populations. Although marginalised groups were disproportionally impacted, few studies and interventions specifically target this group. More targeted studies and interventions are needed to reduce social inequalities with regard to mental health difficulties in the aftermath of the COVID-19 pandemic and to prepare possible future outbreaks.
Open peer review
To view the open peer review materials for this article, please visit https://doi.org/10.1017/gmh.2022.56.
Data availability statement
All data used in this publication are available upon request.
Author contributions
M.M. had the original idea for the study and discussed it at length with all authors. C.C. conducted the literature review, synthesised the studies found and drafted an initial version of the manuscript. M.M. finalised the manuscript, which was read, revised and approved by all authors.
Financial support
This study was made possible owing to funding by the EU Horizon 2020 H2020-SC1-PHE-CORONAVIRUS-2020-2 programme (RESPOND – Improving the Preparedness of Health Systems to Reduce Mental Health and Psychosocial Concerns resulting from the COVID-19 Pandemic project, Grant Agreement 101016127). P.S. benefitted from support from the Paris Institute for Advanced Study (France).
Competing interests
The authors declare no competing interests exist.






Comments
No accompanying comment.