Impact statement
This systematic review is the first to explore the implementation research outcomes of the Friendship Bench to identify and evaluate the barriers and facilitators to its systematic uptake to narrow the mental health treatment gap for common mental disorders. The review highlights that there is high acceptability, appropriateness, feasibility, and scalability in Zimbabwe. There is an opportunity to understand the implementation efforts of the Friendship Bench in other countries. Although the Friendship Bench has been adapted for other health conditions (e.g., HIV), this is the first review to systematically explore implementation efforts specific to mental health conditions.
Introduction
Depressive and anxiety disorders are collectively referred to as common mental disorders (CMDs), which impact the mood or feelings of affected persons. These diagnosable health conditions are termed “common” because of the relatively high prevalence in the population, with symptoms ranging in their severity and duration (Health NCCfM, 2011). Globally, depressive disorders are estimated to impact 4.4% of the population, and anxiety disorders are estimated at 3.6%, with both categories having higher prevalence among females (World Health Organization, 2017). CMDs are one of the leading causes of burden and disability globally, particularly when approximately 75% of those living with CMDs reside in low- and middle-income countries (LMICs) (Moitra et al., Reference Moitra, Santomauro, Collins, Vos, Whiteford, Saxena and Ferrari2022). The 2019 Global Burden of Disease Study ranked depressive disorders as the 13th leading cause of overall burden (Lancet, 2020). Furthermore, there is an alarming treatment gap for CMDs in LMICs. Up to 90% of those needing mental health care do not receive it, and among those who utilize mental health services do not receive adequate treatment (Patel et al., Reference Patel, Maj, Flisher, De Silva, Koschorke and Prince2010; Alonso et al., Reference Alonso, Liu, Evans-Lacko, Sadikova, Sampson, Chatterji, Abdulmalik, Aguilar-Gaxiola, Al-Hamzawi, Andrade, Bruffaerts, Cardoso, Cia, Florescu, de Girolamo, Gureje, Haro, He, de Jonge, Karam, Kawakami, Kovess-Masfety, Lee, Levinson, Medina-Mora, Navarro-Mateu, Pennell, Piazza, Posada-Villa, Ten Have, Zarkov, Kessler and Thornicroft2018).
Global mental health efforts to address this treatment gap have utilized task-sharing strategies to expand mental health care and improve access to the most vulnerable populations (van Ginneken et al., Reference van Ginneken, Tharyan, Lewin, Rao, Meera, Pian, Chandrashekar and Patel2013; Patel et al., Reference Patel, Saxena, Lund, Thornicroft, Baingana, Bolton, Chisholm, Collins, Cooper, Eaton, Herrman, Herzallah, Huang, Jordans, Kleinman, Medina-Mora, Morgan, Niaz, Omigbodun, Prince, Rahman, Saraceno, Sarkar, De Silva, Singh, Stein, Sunkel and UnÜtzer2018). Task-sharing is the redistribution of care normally provided by mental health specialists (e.g., psychologists, psychiatrists) to non-mental health specialists or those with no prior mental health training (e.g., lay/community health workers) (Raviola et al., Reference Raviola, Naslund, Smith and Patel2019). While there is demonstrated evidence of the effectiveness of task-sharing mental health interventions to address CMDs in a variety of settings in LMICs (Karyotaki et al., Reference Karyotaki, Araya, Kessler, Waqas, Bhana, Rahman, Matsuzaka, Miguel, Lund, Garman, Nakimuli-Mpungu, Petersen, Naslund, Schneider, Sikander, Jordans, Abas, Slade, Walters, Brugha, Furukawa, Amanvermez, Mello, Wainberg, Cuijpers and Patel2022; Prina et al., Reference Prina, Ceccarelli, Abdulmalik, Amaddeo, Cadorin, Papola, Tol, Lund, Barbui and Purgato2023), there remains a need to understand how to implement and scale up these interventions broadly in all communities and countries that need more mental health services to address the treatment gap.
The Friendship Bench is a task-sharing mental health intervention that utilizes concepts of Problem-Solving Therapy (PST) to address CMDs. Developed from Cognitive Behavioral Therapy concepts, PST is a brief, step-by-step approach to cognitive problem solving that involves focusing on practical solutions and skill-building (Zhang et al., Reference Zhang, Park, Sullivan and Jing2018). The Friendship Bench was first developed by Dr. Dixon Chibanda in Zimbabwe (Chibanda et al., Reference Chibanda, Mesu, Kajawu, Cowan, Araya and Abas2011). The intervention is delivered through six sessions by lay health workers (LHWs) who are trained in a manualized script and supervised by a mental health professional in primary care facilities. LHWs include trusted elders in the community, with some being referred to as “grandmothers.” The Friendship Bench intervention is delivered on a physical bench in a discreet area outside of a health facility (Chibanda et al., Reference Chibanda, Mesu, Kajawu, Cowan, Araya and Abas2011; Reference Chibanda, Bowers, Verhey, Rusakaniko, Abas, Weiss and Araya2015; Reference Chibanda, Verhey, Munetsi, Cowan and Lund2016b). In Zimbabwe, depressive symptoms are referred to as kufungisisa (the concept of “thinking too much” in Shona – a Bantu language widely spoken in Zimbabwe). Key components of the Friendship Bench include kuvhura pfungwa (“opening of the mind”), kusimudzira (“uplifting”) and kusimbisa (“strengthening”). The full description of the intervention and how it was developed is described elsewhere (Chibanda et al., Reference Chibanda, Mesu, Kajawu, Cowan, Araya and Abas2011; Reference Chibanda, Bowers, Verhey, Rusakaniko, Abas, Weiss and Araya2015; Reference Chibanda, Verhey, Munetsi, Cowan and Lund2016b).
Since it was first developed in 2006, the Friendship Bench has been scaled up in over 100 urban health facilities in Zimbabwe. Improvements in CMD symptoms were demonstrated and measured by a reduction in the Shona Symptom Questionnaire, a locally validated screening tool for CMDs (Chibanda et al., Reference Chibanda, Verhey, Gibson, Munetsi, Machando, Rusakaniko, Munjoma, Araya, Weiss and Abas2016a; Reference Chibanda, Weiss, Verhey, Simms, Munjoma, Rusakaniko, Chingono, Munetsi, Bere, Manda, Abas and Araya2016d; Chibanda, Reference Chibanda2017). One study has evaluated its reach (Verhey et al., Reference Verhey, Chitiyo, Mboweni, Turner, Murombo, Healey, Chibanda, Wagenaar and Araya2022), with several more exploring areas for future application in addressing anxiety (Abas et al., Reference Abas, Weiss, Simms, Verhey, Rusakaniko, Araya and Chibanda2020), trauma (Verhey et al., Reference Verhey, Chibanda, Vera, Manda, Brakarsh and Seedat2020; Reference Verhey, Brakarsh, Gibson, Shea, Chibanda and Seedat2021), suicide (Munetsi et al., Reference Munetsi, Simms, Dzapasi, Chapoterera, Goba, Gumunyu, Weiss, Verhey, Abas, Araya and Chibanda2018) and rural areas in Zimbabwe (Fernando et al., Reference Fernando, Brown, Datta, Chidhanguro, Tavengwa, Chandna, Munetsi, Dzapasi, Nyachowe, Mutasa, Chasekwa, Ntozini, Chibanda and Prendergast2021; Brown et al., Reference Brown, Datta and Fernando2022). The Friendship Bench has also been formatively adapted to a variety of other health conditions including: people living with HIV and adherence to antiretroviral therapy (Chinoda et al., Reference Chinoda, Mutsinze, Simms, Beji-Chauke, Verhey, Robinson, Barker, Mugurungi, Apollo, Munetsi, Sithole, Weiss, Chibanda and Willis2020; Stockton et al., Reference Stockton, Udedi, Kulisewa, Hosseinipour, Gaynes, Mphonda, Maselko, Pettifor, Verhey, Chibanda, Lapidos-Salaiz and Pence2020; Haas et al., Reference Haas, Kunzekwenyika, Hossmann, Manzero, van Dijk, Manhibi, Verhey, Limacher, von Groote, Manda, Hobbins, Chibanda and Egger2021; Ouansafi et al., Reference Ouansafi, Chibanda, Munetsi and Simms2021; Simms et al., Reference Simms, Bernays, Chibanda, Chinoda, Mutsinze, Beji-Chauke, Mugurungi, Apollo, Sithole, Verhey, Weiss and Willis2021; Stockton et al., Reference Stockton, Minnick, Kulisewa, Mphonda, Hosseinipour, Gaynes, Maselko, Pettifor, Go, Udedi and Pence2021; Wogrin et al., Reference Wogrin, Willis, Mutsinze, Chinoda, Verhey, Chibanda and Bernays2021; Simms et al., Reference Simms, Weiss, Chinoda, Mutsinze, Bernays, Verhey, Wogrin, Apollo, Mugurungi, Sithole, Chibanda and Willis2022; Bengtson et al., Reference Bengtson, Filipowicz, Mphonda, Udedi, Kulisewa, Meltzer-Brody, Gaynes, Go, Chibanda, Verhey, Hosseinipour and Pence2023; Garriott et al., Reference Garriott, Gulubane, Poku, Archibald, Entaile, Tshume, Phoi, Matshaba, Ahmed, Lowenthal and Brooks2023; Haas et al., Reference Haas, Kunzekwenyika, Manzero, Hossmann, Limacher, van Dijk, Manhibi, von Groote, Hobbins, Verhey and Egger2023); people living with HIV and on methadone maintenance (Tran et al., Reference Tran, Nong, Tran, Filipowicz, Landrum, Pence, Le, Nguyen, Chibanda, Verhey, Go, Ho and Gaynes2022); noncommunicable diseases (Kamvura et al., Reference Kamvura, Turner, Chiriseri, Dambi, Verhey and Chibanda2021; Reference Kamvura, Dambi, Chiriseri, Turner, Verhey and Chibanda2022); youth in need of mental health care – aptly named the “Youth Friendship Bench” (Brostrom et al., Reference Brostrom, Johansson, Verhey and Landgren2021; Wallén et al., Reference Wallén, Eberhard and Landgren2021; Brooks et al., Reference Brooks, Phetogo, Schwennesen, Phoi, Tshume, Matshaba and Lowenthal2022); and a digital application of the Friendship Bench named “Inuka” (Dambi et al., Reference Dambi, Norman, Doukani, Potgieter, Turner, Musesengwa, Verhey and Chibanda2022; Doukani et al., Reference Doukani, van Dalen, Valev, Njenga, Sera and Chibanda2023). The Friendship Bench has been extensively researched in Zimbabwe, with other research conducted in Botswana (Brooks et al., Reference Brooks, Phetogo, Schwennesen, Phoi, Tshume, Matshaba and Lowenthal2022; Garriott et al., Reference Garriott, Gulubane, Poku, Archibald, Entaile, Tshume, Phoi, Matshaba, Ahmed, Lowenthal and Brooks2023), Kenya (Doukani et al., Reference Doukani, van Dalen, Valev, Njenga, Sera and Chibanda2023), Malawi (Stockton et al., Reference Stockton, Udedi, Kulisewa, Hosseinipour, Gaynes, Mphonda, Maselko, Pettifor, Verhey, Chibanda, Lapidos-Salaiz and Pence2020; Reference Stockton, Minnick, Kulisewa, Mphonda, Hosseinipour, Gaynes, Maselko, Pettifor, Go, Udedi and Pence2021; Bengtson et al., Reference Bengtson, Filipowicz, Mphonda, Udedi, Kulisewa, Meltzer-Brody, Gaynes, Go, Chibanda, Verhey, Hosseinipour and Pence2023) and Vietnam (Tran et al., Reference Tran, Nong, Tran, Filipowicz, Landrum, Pence, Le, Nguyen, Chibanda, Verhey, Go, Ho and Gaynes2022). While the Friendship Bench can act as a tool to narrow the treatment gap for CMDs in LMICs, an understanding of its implementation determinants (i.e., barriers and facilitators) and successes (i.e., implementation outcomes) is needed to inform scale-up of the Friendship Bench in other LMICs.
To our knowledge, no systematic review has ever been conducted on the Friendship Bench, which highlights the importance and timely manner of this investigation. Therefore, the aim of this systematic review is to identify and evaluate the implementation research outcomes of the Friendship Bench and understand the barriers and facilitators to its systematic uptake to narrow the CMD treatment gap.
Proctor et al.’s (Reference Proctor, Silmere, Raghavan, Hovmand, Aarons, Bunger, Griffey and Hensley2011) implementation research outcomes taxonomy has defined how the implementation science field conceptualizes and evaluates implementation success: acceptability, adoption, appropriateness, costs, feasibility, fidelity, penetration, and sustainability (Proctor et al., Reference Proctor, Silmere, Raghavan, Hovmand, Aarons, Bunger, Griffey and Hensley2011). A recent scoping review by Proctor et al. (Reference Proctor, Bunger, Lengnick-Hall, Gerke, Martin, Phillips and Swanson2023) highlighted that the term “scaling up” emerged as a new concept over the past 10 years (Proctor et al., Reference Proctor, Bunger, Lengnick-Hall, Gerke, Martin, Phillips and Swanson2023). Scalability, defined as efforts to increase the impact of an intervention widely, posits that there can be a guided process for maximum implementation of an intervention (Zamboni et al., Reference Zamboni, Schellenberg, Hanson, Betran and Dumont2019). Implementation researchers have advocated the importance of scalability/scaling-up as a needed measurement for effective uptake and sustainability (Gyamfi et al., Reference Gyamfi, Ojo, Iwelunmor, Ogedegbe, Ryan, Diawara, Nnodu, Wonkam, Royal and Peprah2021; Reference Gyamfi, Vieira, Iwelunmor, Watkins, Williams, Peprah, Ogedegbe and Allegrante2022).
A comprehensive systematic review by Le et al. (Reference Le, Eschliman, Grivel, Tang, Cho, Yang, Tay, Li, Bass and Yang2022) developed the “Barriers and Facilitators in Implementation of Task-Sharing Mental Health Interventions” (BeFITS-MH) conceptual framework which is comprised of 37 constructs across eight domains: (1) patient/client characteristics, (2) provider characteristics, (3) family and community factors, (4) organizational characteristics, (5) societal factors, (6) mental health system factors, (7) intervention characteristics and (8) stigma (Le et al., Reference Le, Eschliman, Grivel, Tang, Cho, Yang, Tay, Li, Bass and Yang2022). The factors most amenable to change were most cited as facilitators, including intervention characteristics (i.e., setting, format) and provider characteristics (i.e., knowledge, skills). Conversely, barriers consisted of factors at the macro-level, including societal factors (i.e., sociocultural norms, economic conditions) and stigma to mental illness (Le et al., Reference Le, Eschliman, Grivel, Tang, Cho, Yang, Tay, Li, Bass and Yang2022). The BeFITS-MH framework highlights an ongoing challenge in global mental health efforts that calls for more implementation strategies to integrate task-sharing mental health interventions across a variety of settings.
Methods
Search strategy
We developed a comprehensive search strategy to identify published articles that met predefined inclusion criteria using the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) (Appendix 1, Supplementary Material – PRISMA checklist) (Moher et al., Reference Moher, Liberati, Tetzlaff and Altman2009). The World Bank criteria in 2023 was used to define LMICs (The World Bank, 2023). We identified articles using medical subject headings and keywords including “common mental disorders,” “mental health,” “Friendship Bench,” “LMIC”, and all implementation research outcome terms (Appendix 2, Supplementary Material – Search strategy). We searched the following databases: APA PsycINFO, Cochrane, CINAHL, EMBASE, Global Health, OVID, PubMed/Medline, Science Direct, Web of Science, and gray literature (Google Scholar). The article search was initially conducted in February 2023 and ran again in December 2023 to capture any additional articles. This systematic review was registered on the Open Science Framework on February 10, 2023 (https://doi.org/10.17605/OSF.IO/D8PE7).
Inclusion and exclusion criteria
Articles were included if they met the following inclusion criteria: (1) reported on the Friendship Bench in LMICs, (2) reported on CMDs, (3) reported on implementation research outcomes defined by Proctor et al. (Reference Proctor, Silmere, Raghavan, Hovmand, Aarons, Bunger, Griffey and Hensley2011), and (4) reported using experimental, observational, or qualitative study designs, including case studies. Protocols, commentaries, reviews of any type, and studies that reported on the Friendship Bench as a model for other health outcomes (e.g., antiretroviral adherence for HIV care) were excluded. There were no restrictions on publication date or language.
Data extraction
All citations were downloaded to Covidence. Titles and abstracts of all articles were independently screened and rated by two reviewers to determine if they met inclusion criteria (JP, NO, SZ, CR, SS, DT, EN, BA). Discrepancies were resolved by consensus. A full-text article review was then conducted, and relevant information was extracted by two reviewers (JP, PL, SK, NO, SZ, CR, SS, DT, EN, BA). Specifically, the following study characteristics were retrieved and coded: study location, study design, description of how the Friendship Bench was implemented, implementation research outcome, and barriers and facilitators to implementation. All data were extracted and stored in Covidence.
Quality assessment
To assess the risk of bias, “A comprehenSive tool to Support rEporting and critical appraiSal of qualitative, quantitative and mixed methods implementation reSearch outcomes” (ASSESS Tool) was utilized (Ryan et al., Reference Ryan, Vieira, Gyamfi, Ojo, Shelley, Ogedegbe, Iwelunmor and Peprah2022). The 24-item tool helps to standardize the synthesis and reporting of implementation efforts and to describe studies evaluating implementation research outcomes. After selecting the study design, five questions use criterion to evaluate the design. As an example, qualitative studies use the following criteria: (1) Is the qualitative approach appropriate to answer the research question?; (2) Are the qualitative data collection methods adequate to address the research question?; (3) Are the findings adequately derived from the data?; (4) Is the interpretation of results sufficiently substantiated by data?; and (5) Is there coherence between qualitative data sources, collection, analysis, and interpretation? Criteria differ for each kind of study design. Each question receives a binary score to indicate whether each criterion was met (1) or not met (0). After summing scores across the five criteria, the risk of bias is categorized as high bias (score of 1–2), low bias (score of 3–5), or unclear (unable to be assessed). Two reviewers independently assessed each article and rated for risk of bias (JP and TH).
Results
A total of 685 articles were identified. After removing duplicates, 641 titles and abstracts were screened. Of those, 595 were excluded, yielding 46 articles for which full texts were obtained and reviewed. During the full text review and data extraction, 39 were excluded for wrong study design, wrong intervention, or no implementation outcome. Thus, only 7 articles met all study inclusion criteria and were included for the final analysis (Figure 1).
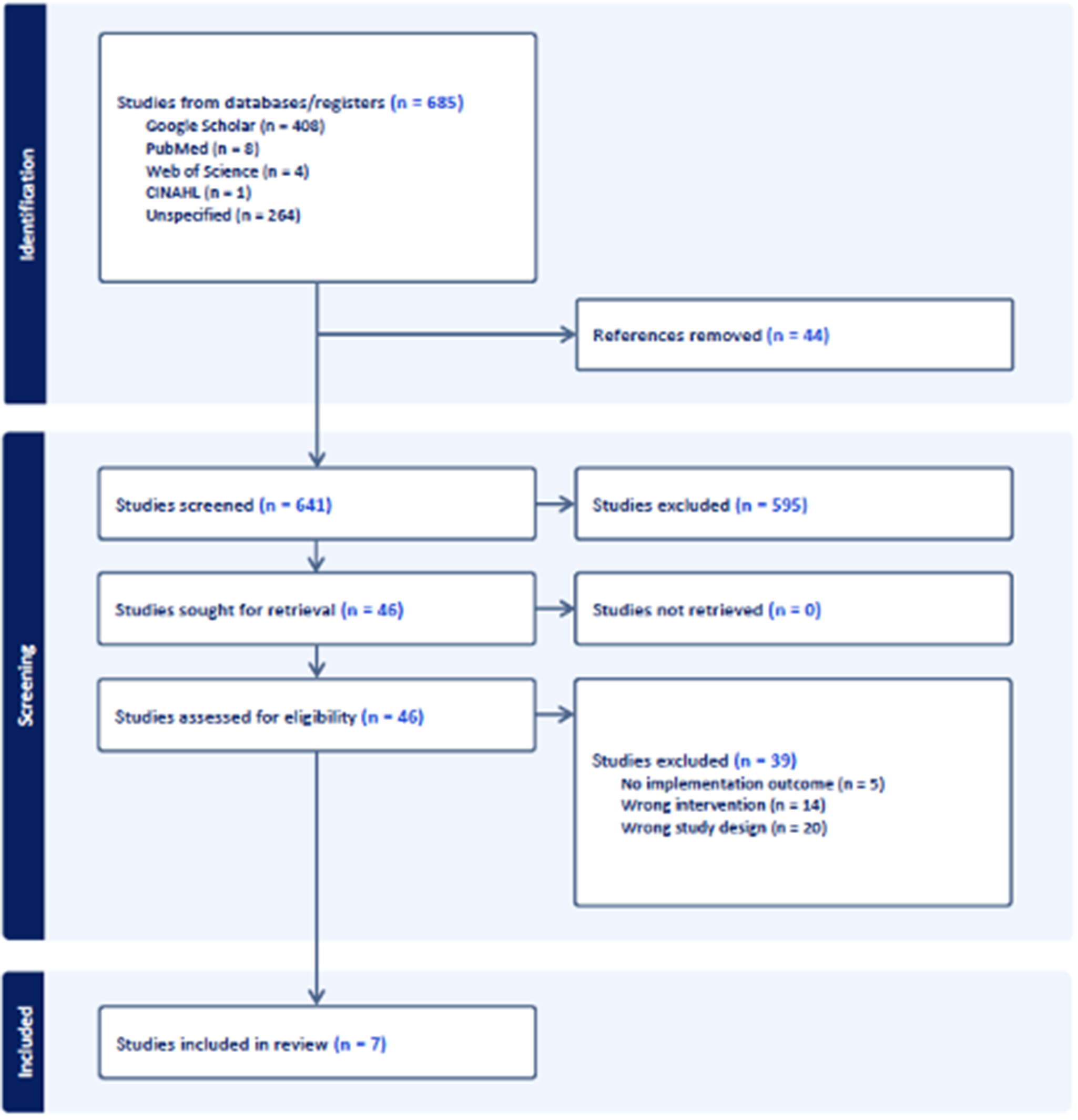
Figure 1. PRISMA flow diagram.
Study characteristics
All seven included articles were conducted in Zimbabwe and published within the past 8 years of this systematic review (Abas et al., Reference Abas, Bowers, Manda, Cooper, Machando, Verhey, Lamech, Araya and Chibanda2016; Chibanda et al., Reference Chibanda, Verhey, Munetsi, Rusakaniko, Cowan and Lund2016c; Reference Chibanda, Weiss, Verhey, Simms, Munjoma, Rusakaniko, Chingono, Munetsi, Bere, Manda, Abas and Araya2016d; Chibanda, Reference Chibanda2017; Fernando et al., Reference Fernando, Brown, Datta, Chidhanguro, Tavengwa, Chandna, Munetsi, Dzapasi, Nyachowe, Mutasa, Chasekwa, Ntozini, Chibanda and Prendergast2021; Healey et al., Reference Healey, Verhey, Mosweu, Boadu, Chibanda, Chitiyo, Wagenaar, Senra, Chiriseri, Mboweni and Araya2022; Verhey et al., Reference Verhey, Chitiyo, Mboweni, Turner, Murombo, Healey, Chibanda, Wagenaar and Araya2022). More than half of the studies (n = 4) utilized qualitative study design components, including focus group discussions and in-depth, semi-structured interviews with either patients, LHWs, or community stakeholders as either a standalone qualitative study (Fernando et al., Reference Fernando, Brown, Datta, Chidhanguro, Tavengwa, Chandna, Munetsi, Dzapasi, Nyachowe, Mutasa, Chasekwa, Ntozini, Chibanda and Prendergast2021), case study (Chibanda, Reference Chibanda2017) or part of a mixed-methods analysis (Abas et al., Reference Abas, Bowers, Manda, Cooper, Machando, Verhey, Lamech, Araya and Chibanda2016; Chibanda et al., Reference Chibanda, Verhey, Munetsi, Rusakaniko, Cowan and Lund2016c). Quantitative, non-randomized study designs components (n = 4) included: conducting descriptive analyses of routine intervention attendance data (Abas et al., Reference Abas, Bowers, Manda, Cooper, Machando, Verhey, Lamech, Araya and Chibanda2016) and a needs assessment and skills assessment (Chibanda et al., Reference Chibanda, Verhey, Munetsi, Rusakaniko, Cowan and Lund2016c) – both as part of a mixed-methods analysis; an economic threshold analysis which used a modeling-based deterministic threshold analysis using a cost-utility framework (Healey et al., Reference Healey, Verhey, Mosweu, Boadu, Chibanda, Chitiyo, Wagenaar, Senra, Chiriseri, Mboweni and Araya2022); and evaluating implementation reach, adoption, and implementation by developing indicators using the “Reach, Efficacy, Adoption, Implementation, Maintenance Framework” (RE-AIM) (Verhey et al., Reference Verhey, Chitiyo, Mboweni, Turner, Murombo, Healey, Chibanda, Wagenaar and Araya2022) – a widely used implementation science framework to evaluate outcomes on the process of scaling up evidence-based interventions (Gaglio et al., Reference Gaglio, Shoup and Glasgow2013). Only one study utilized a clustered randomized control trial with the Friendship Bench as the intervention and enhanced care as control (Chibanda et al., Reference Chibanda, Weiss, Verhey, Simms, Munjoma, Rusakaniko, Chingono, Munetsi, Bere, Manda, Abas and Araya2016d). The study characteristics are provided in Table 1.
Table 1. Characteristics of the studies included in the systematic review
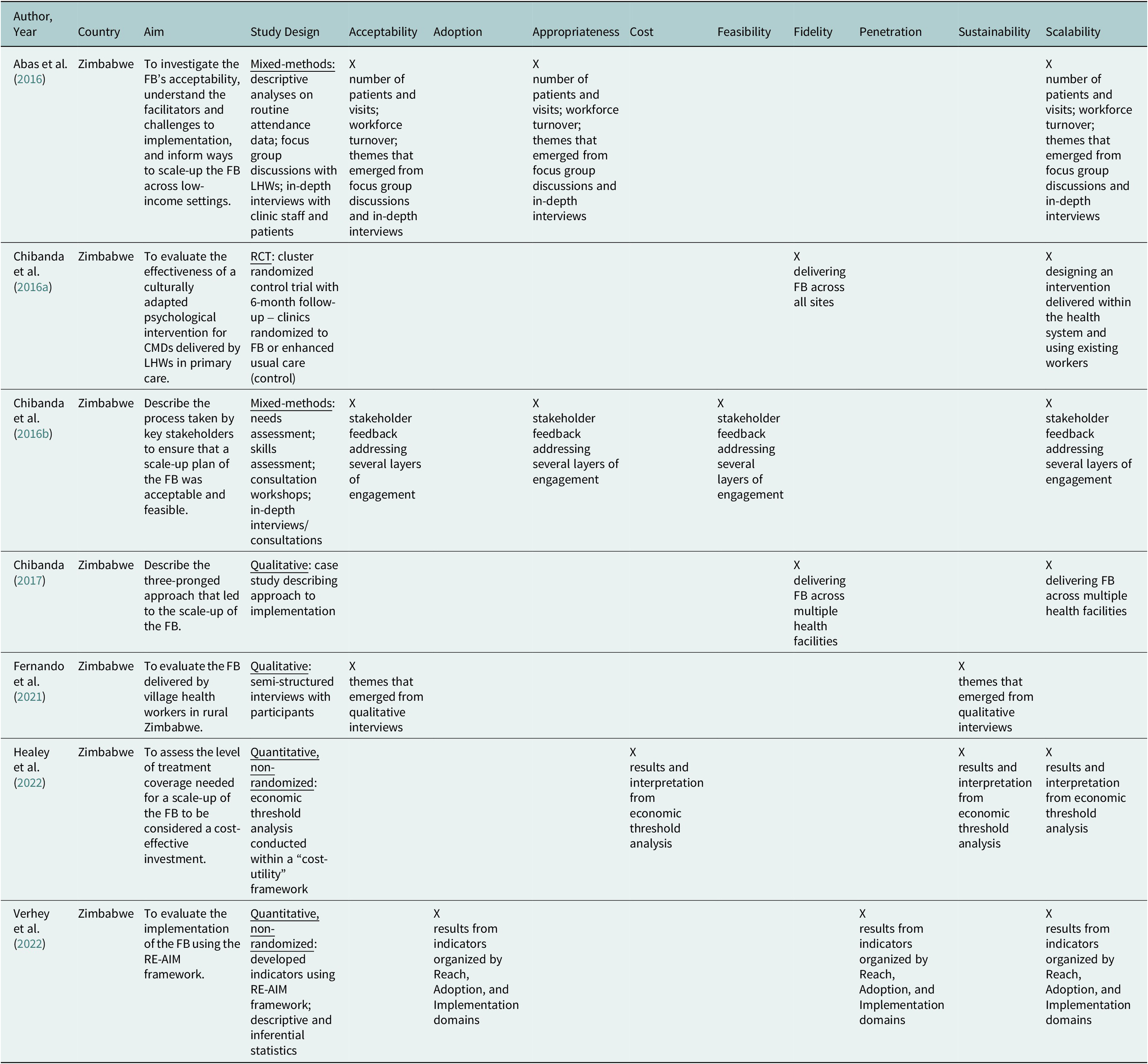
Implementation of research outcomes
All included articles were assessed on the explicit reporting or description of the concept for the following implementation research outcomes: acceptability, adoption, appropriateness, costs, feasibility, fidelity, penetration, and sustainability, with additional attention to scalability or “scaling-up”. Of the studies included, three reported on acceptability (Abas et al., Reference Abas, Bowers, Manda, Cooper, Machando, Verhey, Lamech, Araya and Chibanda2016; Chibanda et al., Reference Chibanda, Verhey, Munetsi, Rusakaniko, Cowan and Lund2016c; Fernando et al., Reference Fernando, Brown, Datta, Chidhanguro, Tavengwa, Chandna, Munetsi, Dzapasi, Nyachowe, Mutasa, Chasekwa, Ntozini, Chibanda and Prendergast2021), one reported on adoption (Verhey et al., Reference Verhey, Chitiyo, Mboweni, Turner, Murombo, Healey, Chibanda, Wagenaar and Araya2022), two reported on appropriateness (Abas et al., Reference Abas, Bowers, Manda, Cooper, Machando, Verhey, Lamech, Araya and Chibanda2016; Chibanda et al., Reference Chibanda, Verhey, Munetsi, Rusakaniko, Cowan and Lund2016c), one reported on costs (Healey et al., Reference Healey, Verhey, Mosweu, Boadu, Chibanda, Chitiyo, Wagenaar, Senra, Chiriseri, Mboweni and Araya2022), one reported on feasibility (Chibanda et al., Reference Chibanda, Verhey, Munetsi, Rusakaniko, Cowan and Lund2016c), two reported on fidelity (Chibanda et al., Reference Chibanda, Weiss, Verhey, Simms, Munjoma, Rusakaniko, Chingono, Munetsi, Bere, Manda, Abas and Araya2016d; Chibanda, Reference Chibanda2017), one reported on penetration (Verhey et al., Reference Verhey, Chitiyo, Mboweni, Turner, Murombo, Healey, Chibanda, Wagenaar and Araya2022) and two reported on sustainability (Fernando et al., Reference Fernando, Brown, Datta, Chidhanguro, Tavengwa, Chandna, Munetsi, Dzapasi, Nyachowe, Mutasa, Chasekwa, Ntozini, Chibanda and Prendergast2021; Healey et al., Reference Healey, Verhey, Mosweu, Boadu, Chibanda, Chitiyo, Wagenaar, Senra, Chiriseri, Mboweni and Araya2022). Even though scalability is not part of the original Proctor et al. (Reference Proctor, Silmere, Raghavan, Hovmand, Aarons, Bunger, Griffey and Hensley2011) taxonomy (Proctor et al., Reference Proctor, Silmere, Raghavan, Hovmand, Aarons, Bunger, Griffey and Hensley2011), it was mentioned or described in all but one study, highlighting the significance of its consideration as an implementation outcome.
Acceptability – the perception that an evidence-based intervention is agreeable or satisfactory – constitutes a wide range from explicitly being reported as the number of patients who utilized the Friendship Bench, workforce retention and themes from qualitative feedback (Abas et al., Reference Abas, Bowers, Manda, Cooper, Machando, Verhey, Lamech, Araya and Chibanda2016; Chibanda et al., Reference Chibanda, Verhey, Munetsi, Rusakaniko, Cowan and Lund2016c; Fernando et al., Reference Fernando, Brown, Datta, Chidhanguro, Tavengwa, Chandna, Munetsi, Dzapasi, Nyachowe, Mutasa, Chasekwa, Ntozini, Chibanda and Prendergast2021). One study that implemented the Friendship Bench in Zimbabwe reported that between 2010 and 2014, there were 5,434 total visits, averaging 505 per year, including multiple visits. A small percentage (5.7%) of patients received 4 or more sessions. In those 4 years, 14 out of 15 LHWs continued to deliver the Friendship Bench, demonstrating strong workforce retention. The study reports that these two statistics are an indicator of high acceptability (Abas et al., Reference Abas, Bowers, Manda, Cooper, Machando, Verhey, Lamech, Araya and Chibanda2016). Patient feedback from focus groups and in-depth interviews found that the Friendship Bench had high socio-cultural acceptability because (1) the intervention used local terminology for emotional distress (kufungisisa – the concept of “thinking too much” in Shona) instead of using stigmatizing terms such as depression; (2) the intervention focused on identifying problems and behavioral activation (what to do about it) – as opposed to identifying their challenges as “feelings”; and (3) the perception that LHWs were like family – in some contexts as “grandmothers” – who shared similar social and economic problems as the patients, perceiving the LHWs as more relatable and more suitable to deliver the intervention (Abas et al., Reference Abas, Bowers, Manda, Cooper, Machando, Verhey, Lamech, Araya and Chibanda2016; Chibanda et al. Reference Chibanda, Verhey, Munetsi, Rusakaniko, Cowan and Lund2016c; Fernando et al., Reference Fernando, Brown, Datta, Chidhanguro, Tavengwa, Chandna, Munetsi, Dzapasi, Nyachowe, Mutasa, Chasekwa, Ntozini, Chibanda and Prendergast2021). Patients welcomed the Friendship Bench as a way to “open up the mind” and expressed wanting the intervention to keep going beyond the initial research study (Abas et al., Reference Abas, Bowers, Manda, Cooper, Machando, Verhey, Lamech, Araya and Chibanda2016; Chibanda et al., Reference Chibanda, Verhey, Munetsi, Rusakaniko, Cowan and Lund2016c; Fernando et al., Reference Fernando, Brown, Datta, Chidhanguro, Tavengwa, Chandna, Munetsi, Dzapasi, Nyachowe, Mutasa, Chasekwa, Ntozini, Chibanda and Prendergast2021). LHWs reported that the Friendship Bench was patient-centered, allowing patients to drive the direction of how they wanted to be helped, while reporting a sense of personal reward and satisfaction being an “agent of change” (Abas et al., Reference Abas, Bowers, Manda, Cooper, Machando, Verhey, Lamech, Araya and Chibanda2016).
Adoption – the intentional action to employ an evidence-based intervention, sometimes referred to as “uptake” – was one of the main, explicitly named indicators created in the RE-AIM study (Verhey et al., Reference Verhey, Chitiyo, Mboweni, Turner, Murombo, Healey, Chibanda, Wagenaar and Araya2022). Sources for the adoption indicator included the number of community health workers who attended a Friendship Bench training, the number of supervisors available, the number of participants seen per month, and whether the clinic had the bench installed. The aggregate scores indicated high adoption overall, ranging from 59% (small clinics) to 71% (large clinics) (Verhey et al., Reference Verhey, Chitiyo, Mboweni, Turner, Murombo, Healey, Chibanda, Wagenaar and Araya2022).
Appropriateness – the perceived fit of the evidence-based intervention for a setting, provider, or consumer – while not explicitly reported on, was captured broadly and jointly with acceptability (Abas et al., Reference Abas, Bowers, Manda, Cooper, Machando, Verhey, Lamech, Araya and Chibanda2016; Chibanda et al., Reference Chibanda, Verhey, Munetsi, Rusakaniko, Cowan and Lund2016c). It can be inferred from studies that discuss patient perceptions that the Friendship Bench helped improve their problems of “thinking too much,” feel more valued in their community, and feel less stigmatized. Feedback from LHWs highlights that the Friendship Bench has a supportive supervision structure and that being trained in PST supported their own lives and the challenges they were experiencing (Abas et al., Reference Abas, Bowers, Manda, Cooper, Machando, Verhey, Lamech, Araya and Chibanda2016; Chibanda et al., Reference Chibanda, Verhey, Munetsi, Rusakaniko, Cowan and Lund2016c).
Cost was reported as the level of treatment coverage needed for the scale-up of the Friendship Bench to be considered cost-effective (Healey et al., Reference Healey, Verhey, Mosweu, Boadu, Chibanda, Chitiyo, Wagenaar, Senra, Chiriseri, Mboweni and Araya2022). A modeling-based deterministic threshold analysis was conducted within a “cost-utility” framework. The authors estimated that an additional 3,413 “service users” (participants who would use the Friendship Bench) would need to be treated each year, estimated to be an additional 10 service users per known active LHW. The associated incremental cost-effective ratio was $191 per year lived with disability avoided. The study concluded that this calculation was reasonable and a convincing reason to scale up the Friendship Bench (Healey et al., Reference Healey, Verhey, Mosweu, Boadu, Chibanda, Chitiyo, Wagenaar, Senra, Chiriseri, Mboweni and Araya2022).
Feasibility – the extent to which an evidence-based intervention can be successfully used or implemented – was reported broadly in terms of the Friendship Bench being “feasible to implement” from stakeholder feedback through qualitative interviews. It was reported jointly with acceptability, emphasizing that ongoing training sessions and securing funding from capacity-building grants help with its feasibility (Chibanda et al., Reference Chibanda, Verhey, Munetsi, Rusakaniko, Cowan and Lund2016c).
Fidelity – the extent to which an evidence-based intervention is implemented as it was originally intended or created – was reported to be a challenge, especially when outside the contexts of a clinical trial (Chibanda et al. Reference Chibanda, Verhey, Munetsi, Rusakaniko, Cowan and Lund2016c; Chibanda, Reference Chibanda2017). One study describes communication challenges between LHWs and their supervisors, along with the hope that using mobile phone features such as texting (e.g., short-message-service, WhatsApp) and communication management tools (e.g., Slack) will mitigate the issue (Chibanda, Reference Chibanda2017). The main paper that assessed overall Friendship Bench effectiveness describes audio recording sessions to ensure adherence to the intervention (Chibanda et al., Reference Chibanda, Weiss, Verhey, Simms, Munjoma, Rusakaniko, Chingono, Munetsi, Bere, Manda, Abas and Araya2016d). Both studies emphasize the need to investigate fidelity more as the Friendship Bench scales up (Chibanda et al., Reference Chibanda, Weiss, Verhey, Simms, Munjoma, Rusakaniko, Chingono, Munetsi, Bere, Manda, Abas and Araya2016d; Chibanda, Reference Chibanda2017).
Penetration – the integration of an evidence-based intervention within a service setting – was not explicitly reported, though its concept was reported as “reach” in the study using the RE-AIM framework (Verhey et al., Reference Verhey, Chitiyo, Mboweni, Turner, Murombo, Healey, Chibanda, Wagenaar and Araya2022). The reach indicator was calculated as the percent of participants registered at the clinic receiving the Shona Symptom Questionnaire, and of those who met a screening threshold, the percent of participants who received the Friendship Bench intervention. Small clinics achieved 34% reach, medium clinics at 9% reach and large clinics at 15% reach, which the authors reported as overall low (Verhey et al., Reference Verhey, Chitiyo, Mboweni, Turner, Murombo, Healey, Chibanda, Wagenaar and Araya2022).
Sustainability – the extent to which an evidence-based intervention is maintained or institutionalized within a setting – was reported by one study as the percentage of patients still engaged with the Friendship Bench after 1 year of the initial research study (Fernando et al., Reference Fernando, Brown, Datta, Chidhanguro, Tavengwa, Chandna, Munetsi, Dzapasi, Nyachowe, Mutasa, Chasekwa, Ntozini, Chibanda and Prendergast2021). Fifty-two percent of patients were still actively engaged and reported that the Friendship Bench continued to “relax their mind.” Additionally, 67% maintained or expanded their income-generating projects as a result of improved mental health, a factor that the study explained as a positive long-term outcome (Fernando et al., Reference Fernando, Brown, Datta, Chidhanguro, Tavengwa, Chandna, Munetsi, Dzapasi, Nyachowe, Mutasa, Chasekwa, Ntozini, Chibanda and Prendergast2021). The economic analysis threshold described in Costs advocates that the Friendship Bench has the potential to be a cost-effective intervention, which supports long-term sustainability (Healey et al., Reference Healey, Verhey, Mosweu, Boadu, Chibanda, Chitiyo, Wagenaar, Senra, Chiriseri, Mboweni and Araya2022).
Scalability – the efforts to increase the impact of an evidence-based intervention widely – was mentioned explicitly in all but one of the studies, highlighting the importance of “scaling up” the Friendship Bench (Abas et al., Reference Abas, Bowers, Manda, Cooper, Machando, Verhey, Lamech, Araya and Chibanda2016; Chibanda et al., Reference Chibanda, Verhey, Munetsi, Rusakaniko, Cowan and Lund2016c; Reference Chibanda, Weiss, Verhey, Simms, Munjoma, Rusakaniko, Chingono, Munetsi, Bere, Manda, Abas and Araya2016d; Chibanda, Reference Chibanda2017; Healey et al., Reference Healey, Verhey, Mosweu, Boadu, Chibanda, Chitiyo, Wagenaar, Senra, Chiriseri, Mboweni and Araya2022; Verhey et al., Reference Verhey, Chitiyo, Mboweni, Turner, Murombo, Healey, Chibanda, Wagenaar and Araya2022). Themes that emerged included (1) needing to integrate the intervention within existing health systems and workflows (Chibanda et al., Reference Chibanda, Weiss, Verhey, Simms, Munjoma, Rusakaniko, Chingono, Munetsi, Bere, Manda, Abas and Araya2016d; Verhey et al., Reference Verhey, Chitiyo, Mboweni, Turner, Murombo, Healey, Chibanda, Wagenaar and Araya2022); (2) utilizing LHWs with their existing competencies and connections with the community (Abas et al., Reference Abas, Bowers, Manda, Cooper, Machando, Verhey, Lamech, Araya and Chibanda2016; Chibanda et al., Reference Chibanda, Verhey, Munetsi, Rusakaniko, Cowan and Lund2016c); (3) maximizing community engagement by involving stakeholders as partners and focusing on building trust (Abas et al., Reference Abas, Bowers, Manda, Cooper, Machando, Verhey, Lamech, Araya and Chibanda2016; Chibanda, Reference Chibanda2017); (4) political buy-in from local health authorities (Chibanda et al., Reference Chibanda, Verhey, Munetsi, Rusakaniko, Cowan and Lund2016c; Chibanda, Reference Chibanda2017); and (5) demonstrating how cost-effective the intervention is (Healey et al., Reference Healey, Verhey, Mosweu, Boadu, Chibanda, Chitiyo, Wagenaar, Senra, Chiriseri, Mboweni and Araya2022).
Facilitators to implementing the Friendship Bench
Patient/client characteristics – The most relevant personal attributes that facilitated implementation success were a patient’s motivation or readiness to participate in the Friendship Bench. The evidence on acceptability and appropriateness highlights that patients were eager to try the Friendship Bench. As illustrated by the BeFITS-MH framework, this is the most cited facilitator and, as a result, predictor for success. While a patient’s baseline skills and self-efficacy for help-seeking behaviors are also important facilitators in this domain, it was not explicitly measured in the included studies.
Task-sharing provider characteristics – The personal attributes of the task-sharing provider (e.g., LHWs) were also highly cited as facilitators to implementation. LHWs’ skills, self-efficacy, and knowledge were measured in the skills assessment and showed high levels of competency in being approachable, trustworthy, mature, “motherly,” and having listening skills. Additionally, LHWs’ other personal attributes, being perceived as family members, their trusted role in the community, and being perceived as having the same social and economic problems as the patients all contribute to facilitation. LHWs are deeply integrated in the community and have a deep sense of local norms, culture, context, and understanding of the issues faced by the community. The social role and identity that LHWs perceived themselves to be “agents of change” also contributes significantly (Abas et al., Reference Abas, Bowers, Manda, Cooper, Machando, Verhey, Lamech, Araya and Chibanda2016; Chibanda, Reference Chibanda2017). The BeFITS-MH framework highlights these attributes as top facilitators in this domain and therefore leads to increased acceptability of the intervention.
Intervention characteristics – Unsurprisingly, components of the Friendship Bench intervention itself were overwhelmingly discussed as facilitators. From using local terminology to describe emotional distress, to focusing on “problems” as opposed to “feelings,” to having a patient-centered approach allowing the patient to be the driver of their treatment, the Friendship Bench resonated positively for both patients and LHWs. The supportive supervision structure – having access to peer LHWs and mental health professionals – led to the top-cited LHW perspective of feeling well-supported. Using the Friendship Bench as a separate entity to healthcare facilities – dyads meet in a discreet area on a physical bench – was also a facilitator. The BeFITS-MH framework reports that these intervention characteristics are the most amenable to change: having the most agency in changing components of the intervention that will support the intended population. These factors lead to the acceptability of the components of the Friendship Bench.
Organizational factors – Broader factors at the organizational level include collaboration across community organizations and health authorities. Included studies described how there was governmental buy-in for the Friendship Bench when it was presented as (1) emphasizing the added value of treating CMDs as a comorbid condition to existing public health programs (e.g., HIV, malaria, non-communicable diseases), (2) emphasizing utilizing existing resources of LHWs and other infrastructure resources, and (3) when policymakers were invited as part of the stakeholder engagement process. These factors lead to the feasibility of implementing the Friendship Bench.
Barriers to implementing the Friendship Bench
Intervention characteristics – While an extensive list of Friendship Bench intervention characteristics served as facilitators, there were also key barriers to successful implementation. LHWs overwhelmingly noted that there was insufficient training for assessing and managing more serious mental health conditions such as suicide, domestic violence, and hostile patients. There is also a lack of comprehensive documentation and follow-up, making it challenging to monitor who has received the intervention. This highlights key barriers in task-sharing mental health interventions in general and asks the question: is task-sharing “enough”? One perspective advocates that task-sharing mental health interventions provide help for those experiencing mild to moderate CMD symptoms (Karyotaki et al., Reference Karyotaki, Araya, Kessler, Waqas, Bhana, Rahman, Matsuzaka, Miguel, Lund, Garman, Nakimuli-Mpungu, Petersen, Naslund, Schneider, Sikander, Jordans, Abas, Slade, Walters, Brugha, Furukawa, Amanvermez, Mello, Wainberg, Cuijpers and Patel2022; Prina et al., Reference Prina, Ceccarelli, Abdulmalik, Amaddeo, Cadorin, Papola, Tol, Lund, Barbui and Purgato2023). Those that may require more comprehensive care, including pharmacological treatments and therapy, would not receive that level of care from task-sharing. Additionally, although the Friendship Bench is intended for a low-intensity psychological intervention, there could be an opportunity to expand to other mental and behavioral health conditions, such as post-traumatic stress disorder and substance use disorders.
Mental health system factors – Unsurprisingly, the infrastructure-related factors of the mental health system contribute significantly to barriers. Similar to the barriers noted above, if patients require more comprehensive services in primary care or medication management to address their mental health conditions, the Friendship Bench is limited to what it can offer. Included studies highlight that the overall lack of mental health training and resources, unreliable referral systems and lack of mental health professionals perpetuate the mental health treatment gap. The BeFITS-MH model reinforces these concepts by illustrating that the human resources needed for sufficient mental health care is deficient and task-sharing mental health interventions cannot be the only source of support for populations who need it. To address these issues, a coordinated effort among local health authorities and communities needs to be conducted. Establishing referral systems and capacity for mental health facilities will strengthen the task-sharing model.
Stigma – Perhaps the most complicated and complex factor in implementation, stigma is solely reported as hindering implementation success and cuts across all domains and levels of the BeFITS-MH framework (Le et al., Reference Le, Eschliman, Grivel, Tang, Cho, Yang, Tay, Li, Bass and Yang2022). Mental illness stigma in LMICs has been an ongoing challenge in the mental health treatment gap (Mascayano et al., Reference Mascayano, Armijo and Yang2015). Termed as a “universal phenomenon,” stigma is perhaps the strongest barrier as it originates from personal, cultural, and societal mindsets of what “mental health” is. The Friendship Bench, while noting its many positive attributes, is still not immune to some populations’ hesitancy to engage in an intervention that discusses personal problems and experiences.
Quality assessment
The ASSESS Tool was used to determine the risk of bias based on the type of study design for each included article: mixed-methods, qualitative, quantitative, non-randomized and randomized control trial. The risk of bias is categorized as high bias (score of 1–2), low bias (score of 3–5), or unclear (unable to be assessed). Six of the included articles were rated between a score of 4 and 5, thus having low bias – an indicator of being a high-quality study. The remaining article, Chibanda et al.’s (Chibanda, Reference Chibanda2017) case study (Chibanda, Reference Chibanda2017), was deemed as unable to be assessed, given there was no epidemiologic study design used (Figure 2).
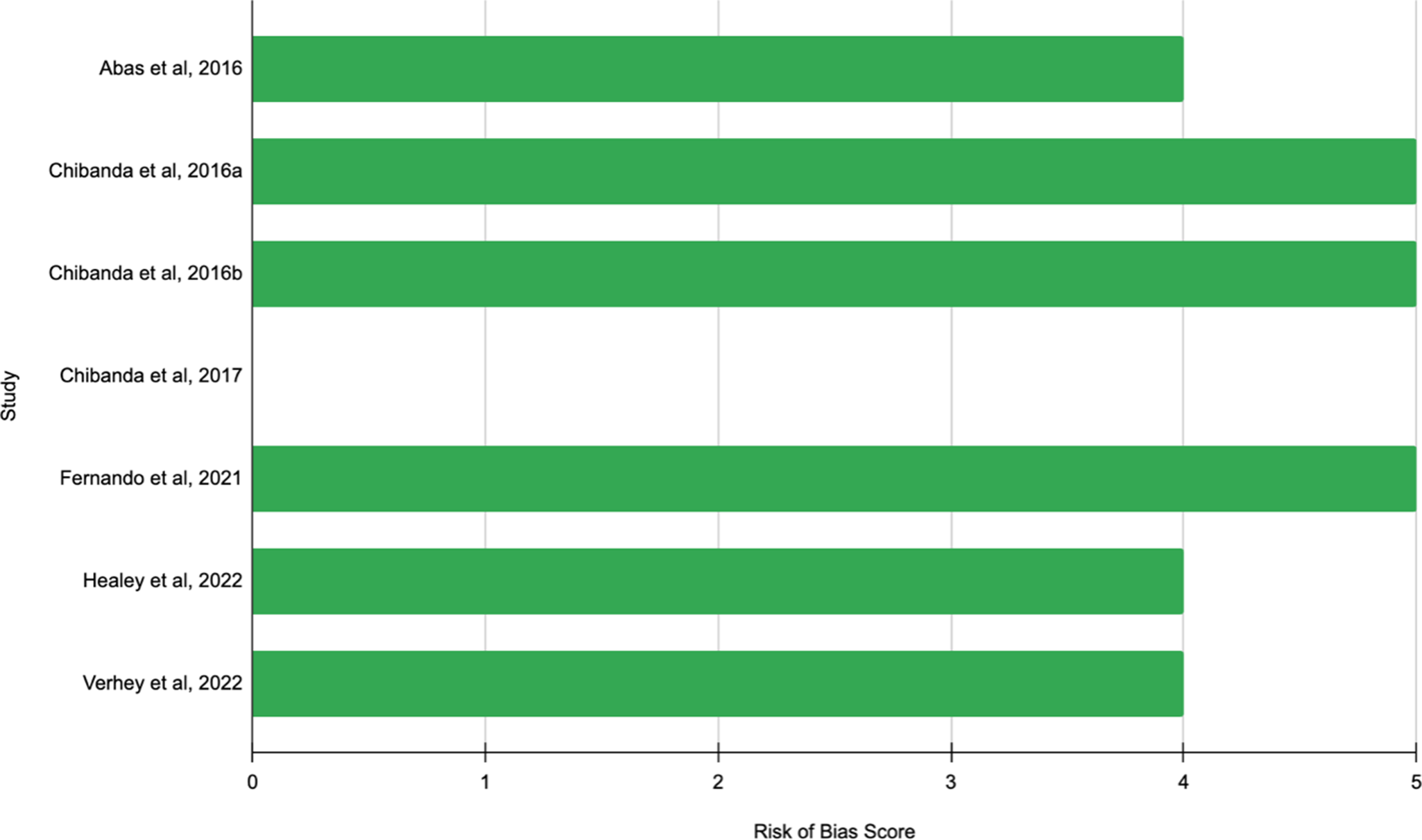
Figure 2. Risk of bias.
Discussion
To our knowledge, this is the first systematic review to synthesize the findings on the implementation determinants and outcomes of the Friendship Bench as a task-sharing intervention to address common mental disorders. While LMICs were included in the search strategy, results only featured work in Zimbabwe, highlighting the implementation outcomes associated with the Friendship Bench for this setting only.
The seven articles included in this review reported on all implementation research outcomes per Proctor et al.’s (Reference Proctor, Silmere, Raghavan, Hovmand, Aarons, Bunger, Griffey and Hensley2011) taxonomy (Proctor et al., Reference Proctor, Silmere, Raghavan, Hovmand, Aarons, Bunger, Griffey and Hensley2011) – acceptability (n = 3), adoption (n = 1), appropriateness (n = 2), costs (n = 1), feasibility (n = 1), fidelity (n = 2), penetration (n = 1), and sustainability (n = 2) – with an additional focus on scalability (n = 6), a burgeoning implementation research outcome that deserves attention. While included studies reported on the full taxonomy list, some are reported more explicitly while others are inferred. Acceptability is the most reported on (Abas et al., Reference Abas, Bowers, Manda, Cooper, Machando, Verhey, Lamech, Araya and Chibanda2016; Chibanda et al., Reference Chibanda, Verhey, Munetsi, Rusakaniko, Cowan and Lund2016c; Fernando et al., Reference Fernando, Brown, Datta, Chidhanguro, Tavengwa, Chandna, Munetsi, Dzapasi, Nyachowe, Mutasa, Chasekwa, Ntozini, Chibanda and Prendergast2021), and clearly defined in studies on how it was measured and evaluated. Acceptability is one of the most widely evaluated implementation outcomes (Proctor et al., Reference Proctor, Bunger, Lengnick-Hall, Gerke, Martin, Phillips and Swanson2023) and is one of the most common questions to ask when implementing an intervention: how acceptable is this to the intended population? Similarly, adoption was explicitly created as an implementation indicator (Verhey et al., Reference Verhey, Chitiyo, Mboweni, Turner, Murombo, Healey, Chibanda, Wagenaar and Araya2022) and cost is a straightforward outcome to measure (Healey et al., Reference Healey, Verhey, Mosweu, Boadu, Chibanda, Chitiyo, Wagenaar, Senra, Chiriseri, Mboweni and Araya2022). On the other hand, appropriateness and feasibility were not outcomes that were explicitly reported on or measured, but could be inferred based on how it was described in the studies; interestingly both were broadly jointed with acceptability (Abas et al., Reference Abas, Bowers, Manda, Cooper, Machando, Verhey, Lamech, Araya and Chibanda2016; Chibanda et al., Reference Chibanda, Verhey, Munetsi, Rusakaniko, Cowan and Lund2016c). While the term “penetration” was not explicitly reported on, “reach” is an accurate measurement of the level of integration within a service setting and was formally evaluated using the RE-AIM framework (Verhey et al., Reference Verhey, Chitiyo, Mboweni, Turner, Murombo, Healey, Chibanda, Wagenaar and Araya2022). Sustainability was also reported on by name, emphasizing the need to maintain the implementation of the Friendship Bench beyond the research study (Fernando et al., Reference Fernando, Brown, Datta, Chidhanguro, Tavengwa, Chandna, Munetsi, Dzapasi, Nyachowe, Mutasa, Chasekwa, Ntozini, Chibanda and Prendergast2021; Healey et al., Reference Healey, Verhey, Mosweu, Boadu, Chibanda, Chitiyo, Wagenaar, Senra, Chiriseri, Mboweni and Araya2022). Overall, there is high acceptability, appropriateness, and feasibility of the Friendship Bench, with lower evidence demonstrating its overall reach and sustainability. To enhance the measurement and evaluation of these implementation research outcomes, studies could employ validated and reliable measures. Mettert et al. (Reference Mettert, Lewis, Dorsey, Halko and Weiner2020) published a systematic review that identified 102 measures that could be used to quantitatively assess implementation outcomes for mental health and behavioral health studies (Mettert et al., Reference Mettert, Lewis, Dorsey, Halko and Weiner2020). None of the included studies for this review on the Friendship Bench utilized these measures.
Interestingly, although the Friendship Bench has been formatively researched in Botswana (Brooks et al., Reference Brooks, Phetogo, Schwennesen, Phoi, Tshume, Matshaba and Lowenthal2022; Garriott et al., Reference Garriott, Gulubane, Poku, Archibald, Entaile, Tshume, Phoi, Matshaba, Ahmed, Lowenthal and Brooks2023), Kenya (Doukani et al., Reference Doukani, van Dalen, Valev, Njenga, Sera and Chibanda2023), Malawi (Stockton et al., Reference Stockton, Udedi, Kulisewa, Hosseinipour, Gaynes, Mphonda, Maselko, Pettifor, Verhey, Chibanda, Lapidos-Salaiz and Pence2020; Reference Stockton, Minnick, Kulisewa, Mphonda, Hosseinipour, Gaynes, Maselko, Pettifor, Go, Udedi and Pence2021; Bengtson et al., Reference Bengtson, Filipowicz, Mphonda, Udedi, Kulisewa, Meltzer-Brody, Gaynes, Go, Chibanda, Verhey, Hosseinipour and Pence2023) and Vietnam (Tran et al., Reference Tran, Nong, Tran, Filipowicz, Landrum, Pence, Le, Nguyen, Chibanda, Verhey, Go, Ho and Gaynes2022), all included studies were in Zimbabwe because studies from these other locations address adaptations to the Friendship Bench for other health conditions. This review focused on the implementation research outcomes of the Friendship Bench as it addresses CMDs. Moreover, beyond research, the Friendship Bench has established itself as a non-governmental organization (www.friendshipbenchzimbabwe.org) registered in Zimbabwe as a Private Voluntary Organization with the Department of Social Service. The Friendship Bench organization provides the intervention as a manualized toolkit that can be implemented globally. According to their 2023 Annual Impact Report, the Friendship Bench has been implemented in Zimbabwe, Jordan, Kenya, Malawi, Tanzania, the United Kingdom, the United States of America, and Vietnam to over 482,000 people delivered by 2,000 LHWs since 2016 (Bench, Reference Bench2023). However, there is no published research on these implementation efforts.
This lack of reporting on implementation research outcomes highlights a challenge in the field: there are not enough studies being conducted to explicitly examine the full taxonomy of implementation outcomes. Only 1 of the 7 studies used an implementation science framework to formally evaluate an implementation outcome – the Verhey et al. (Reference Verhey, Chitiyo, Mboweni, Turner, Murombo, Healey, Chibanda, Wagenaar and Araya2022) study which utilized RE-AIM (Verhey et al., Reference Verhey, Chitiyo, Mboweni, Turner, Murombo, Healey, Chibanda, Wagenaar and Araya2022). As Proctor et al. (Reference Proctor, Bunger, Lengnick-Hall, Gerke, Martin, Phillips and Swanson2023) explained, implementation researchers are not as equipped or prepared to achieve implementation success when there is not enough research on outcomes such as penetration, sustainability or appropriateness using rigorous, analytical study designs (Proctor et al., Reference Proctor, Bunger, Lengnick-Hall, Gerke, Martin, Phillips and Swanson2023).
Strengths and limitations
This study used a rigorous search strategy. Pre-specified inclusion and exclusion criteria were used to retrieve articles across multiple databases. No restrictions were placed on article publication date or language published in order to capture all relevant articles. A limitation included the exclusive focus on the Friendship Bench as it relates to addressing CMDs. There were several articles discussing implementation efforts; however, as they related to other health conditions, it was excluded from this review. Information from these other studies could have also contributed to understanding the Friendship Bench’s scalability, especially since it was conducted in countries outside of Zimbabwe.
Conclusion
This systematic review examined the implementation efforts of the Friendship Bench to address CMDs in LMICs. There is strong evidence that the Friendship Bench is acceptable, appropriate, and feasible to address the CMD treatment gap in Zimbabwe. Facilitators include that the Friendship Bench is culturally adaptable, utilizes trusted LHWs, and has relatively strong community and political buy-in. Conversely, barriers include a lack of a reliable mental health system, limitations in its ability to treat more serious mental conditions, and mental health stigma. The presented information on the facilitators and barriers is limited to the context of Zimbabwe. There is an opportunity to explore the application of the Friendship Bench for CMDs in other countries. Additionally, there is an opportunity to evaluate the implementation outcomes of the Friendship Bench as a basis for novel task-sharing interventions for other health conditions. The evidence demonstrates that the Friendship Bench holds promise for bridging the mental health treatment gap, however, more research is required.
Open peer review
To view the open peer review materials for this article, please visit http://doi.org/10.1017/gmh.2025.10025.
Supplementary material
The supplementary material for this article can be found at http://doi.org/10.1017/gmh.2025.10025.
Data availability statement
Data sharing is not applicable – no new data generated.
Author contribution
All authors contributed to the development of this manuscript. JP: conceptualization, formal analysis, project administration, writing – original draft. DA: formal analysis, writing – review & editing. PL: formal analysis, writing – review & editing. TH: formal analysis, writing – review & editing. SK: formal analysis, writing – review & editing. DT: formal analysis, writing – review & editing. EN: formal analysis, writing – review & editing. BA: formal analysis, writing – review & editing. DV: data curation, writing – review & editing. JG: writing – review & editing. EP: supervision, writing – review & editing.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Competing interests
The authors declare none.






Comments
No accompanying comment.