1. Introduction
Population ageing affects the long-term care (LTC) sector since older persons, considered the demand side for LTC services, are increasing in number. In contrast, the supply side of LTC services (especially for informal care) such as family members, relatives, friends and neighbours is in decline due to lower fertility and higher women's labour participation (Norton, Reference Norton, Piggott and Woodland2016). This profound demographic change requires many countries to make various attempts to address the increasing needs for LTC by expanding their public schemes (Morel, Reference Morel, Armingeon and Bonoli2007) while reducing their public policy interventions in pension, labour market, health care, etc. (Pavolini and Ranci, Reference Pavolini, Ranci, Ranci and Pavolini2013). Although the specifics of the LTC system, such as benefit package and coverage and the mix of financing arrangements, vary across different countries, public LTC services are available in most high-income countries and substitute increasingly for informal caregiving (Norton, Reference Norton, Piggott and Woodland2016).
A majority of previous studies have demonstrated that public (or formal) LTC had an effect on the reduction of informal caregiving or vice versa (Tennstedt et al., Reference Tennstedt, Crawford and McKinlay1993; Van Houtven and Norton, Reference Van Houtven and Norton2004; Charles and Sevak, Reference Charles and Sevak2005; Bolin et al., Reference Bolin, Lindgren and Lundborg2008; Bakx et al., Reference Bakx, De Meijer, Schut and Van Doorslaer2015; Kim and Lim, Reference Kim and Lim2015). There is a consensus that public LTC and informal care have a substitution relationship, while the magnitude of substitution can differ depending on the social norms on family responsibility and characteristics of the public LTC system (e.g. eligibility criteria and benefit package) in different countries (Bakx et al., Reference Bakx, De Meijer, Schut and Van Doorslaer2015). Despite considerable evidence that formal care substitutes for informal care, only a few studies describe the association between public LTC and medical services (Gaughan et al., Reference Gaughan, Gravelle and Siciliani2015; Spiers et al., Reference Spiers, Matthews, Moffatt, Barker, Jarvis, Stow, Kingston and Hanratty2019). Furthermore, such studies show mixed results that are not consistent (Spiers et al., Reference Spiers, Matthews, Moffatt, Barker, Jarvis, Stow, Kingston and Hanratty2019).
The most common explanation of the association between public LTC and medical services is that utilisation of medical services leads to falling demand for LTC. For instance, medical treatment through antithrombotic drugs following a stroke or hip replacement could reduce the risk of cognitive and functional impairments deriving from sequelae of disease and surgery (Forder, Reference Forder2009). Also, increasing the supply of LTC can decrease the utilisation of medical services. Delayed discharges, which refer to unnecessary longer stays in hospitals by patients who are clinically ready for discharge, can occur because an in-home caregiver is not available after discharge or a long-term care facility (LTCF) is not readily accessible (Victor et al., Reference Victor, Healy, Thomas and Seargeant2000). Sufficient provision of LTC services drives down delayed discharges and reduces the length of stay in hospitals (Konetzka et al., Reference Konetzka, Spector and Limcangco2008; Forder, Reference Forder2009). From a long-term perspective, the provision of LTC services enables older people to maintain and improve their cognitive/physical function and health and eventually decrease their utilisation of medical services (Deraas et al., Reference Deraas, Berntsen, Hasvold and Førde2011).
On the other hand, the increasing use of LTC can positively influence the utilisation of medical services by older people. LTC services provide improved access to health care for people whose medical condition prevents them from visiting hospitals or clinics. They also allow caregivers to grasp older people's latent medical care needs while delivering service. Therefore, it will result in an increase in the utilisation of medical services in the short term (Deraas et al., Reference Deraas, Berntsen, Hasvold and Førde2011; Park et al., Reference Park, Jeon, Lee, Ko, Kim, Kim, Lee, Jung, Jo, Kim, Jung, Lee and Kwon2011), although future medical demand can be decreased by early intervention.
Previous studies undertaken in various countries reveal the effects of LTC services on medical service utilisation. In the United Kingdom, increasing expenditures and supply of LTC services lead to falling utilisation of hospital services, such as delayed discharge, the average length of stay and re-admissions to the emergency room (Forder, Reference Forder2009; Gaughan et al., Reference Gaughan, Gravelle and Siciliani2015). The expansion of public subsidies for LTC in Spain reduced hospital admissions and length of stay (Costa-Font et al., Reference Costa-Font, Jimenez-Martin and Vilaplana2018). Although most empirical studies show that increased LTC utilisation is associated with reduced medical service utilisation, a national population-based observational study in Norway has demonstrated evidence of a positive correlation between LTC and medical care (Deraas et al., Reference Deraas, Berntsen, Hasvold and Førde2011).
In South Korea, public long-term care insurance (LTCI) was introduced in July 2008 in order to provide formal care for older people with cognitive and functional impairment and limitations in activities of daily living. The main purpose of LTCI is to help seniors enjoy healthy ageing by providing them with timely and appropriate care services. Furthermore, the LTCI in South Korea is expected to improve efficiency by reducing older people's prolonged stay in hospitals (also referred to as social admissions) (Kwon, Reference Kwon2008), which is considered medically unnecessary for social reasons such as the absence of an in-home caregiver. However, although the use of medical services by older people has partially reduced after the launch of LTCI (Kim et al., Reference Kim, Sunwoo, Lee, Choi, Lee and Kim2013a, Reference Kim, Kwon and Kim2013b; Hyun et al., Reference Hyun, Kang and Lee2014; Kim and Lim, Reference Kim and Lim2015), the number of hospitalisations has increased [especially in long-term care hospitals (LTCHs)] (Kim et al., Reference Kim, Sunwoo, Lee, Choi, Lee and Kim2013a, Reference Kim, Kwon and Kim2013b) and it is uncertain whether social admissions of older people have reduced or not after the introduction of LTCI. Therefore, further study is needed to investigate the effects of the introduction of LTCI on social admissions.
This study aims to evaluate the effects of the introduction of LTCI on older people's medical service use, including outpatient visits, inpatient services and long-term hospital stays (181 days or longer) in South Korea.
2. Institutional background
2.1 LTCI in South Korea
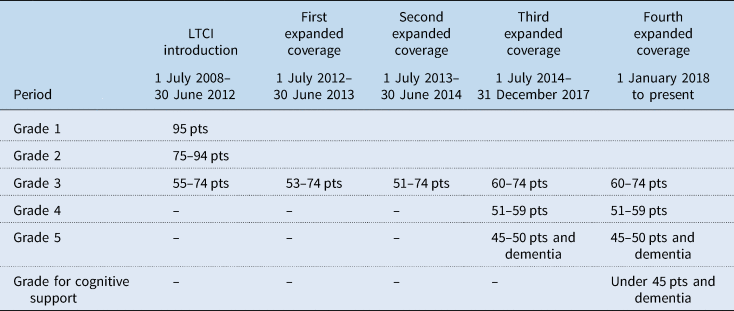
All persons covered by the National Health Insurance (NHI), contribution-based mandatory health insurance for all citizens in South Korea, are automatically enrolled in LTCI. LTCI covers all types of LTC needs of older people aged 65 years or older and age-related LTC needs (e.g. dementia) of those under 65 years once they become eligible through an LTC approval process. An LTC needs assessment team visits the applicant's residence to assess his/her physical/cognitive functions (the availability of informal care was not considered to evaluate the need for public LTC services in South Korea). The assessment results are aggregated and converted into an LTC approval score ranging from 0 to 100. The LTC grade of an applicant is determined based on the LTC approval score and the decision of the LTC eligibility committee. There were three LTC grades in the early years of introduction: grade 1 (95–100 pts) as the most severe case, grade 2 (75–94 pts) and grade 3 (55–74 pts) as the least severe case. As of 2020, there are a total of six grades since the criteria for LTC benefit eligibility have been eased to cover more beneficiaries (Table 1).
Table 1. History of change in the criteria for LTC grades
The benefit package mainly consists of in-kind benefits, i.e. home care and institutional care services. Home care services include home-visit care/nursing/bathing and provision of assistive devices such as a wheelchair, walker, bath chair, etc. Institutional care services are provided through LTCF and congregate housing for older people. In principle, recipients of LTC grade 3 are not eligible for institutional care. Cash benefits are only granted under exceptional circumstances, e.g. residents in remote places, patients with communicable diseases or mental problems including social phobia, and under the circumstances following natural disasters. Ceiling on benefit coverage for home care ranges from ₩566,600 (about 480 USD) to ₩1,498,300 (about 1270 USD) per month, depending on the LTC grades as of 2020.
2.2 Social admission in South Korea
Prior to the introduction of LTCI in South Korea in 2008, the LTC sector relied on informal care for older people, and the only channel for older people with LTC needs to receive public support was the national basic livelihood security welfare system (public assistance), which provided senior care services for citizens living in absolute poverty. The majority of older people, who did not fall under this case, had to receive care support from their families or meet their LTC needs by staying in hospitals for a prolonged period (because they are paid by NHI) or paying for using (private) nursing homes. In many cases, these older people stay in LTCHs, which are subject to lower requirements for medical staffing and provide medical services such as management of sequelae/side effects of disease or surgery for subacute patients before they return to their communities. Meanwhile, older people can choose formal care covered by social insurance after the introduction of LTCI. They can use public LTC services, including home care or institutional care, as long as they are eligible through the LTC approval process. As a result, older people with LTC needs in South Korea have the following service options to address their needs. The first is informal care, which older people use when available. The second is home care service or institutional services provided by public LTCI. Older people who cannot stay at home due to high LTC needs would choose institutional service, while home care services would be sufficient for those with relatively mild LTC needs. Lastly, a long-term stay in an LTCH is one of the possible options in the South Korean context. The reason for using an LTCH is similar to that of an LTCF. However, there are additional motivations for choosing an LTC hospital.
One of the reasons behind choosing admissions in LTCHs is that going to LTCHs by even mild case patients is easier than entering LTCFs, which require an LTC approval process (Hwang et al., Reference Hwang, Shin, Lee, Choi, Kim, Park and Kim2016). Patients with LTC needs should be recognised through an LTC eligibility assessment to receive institutional or home-based care services. However, they can be admitted to an LTCH at the discretion of a health care professional even though their cases are mild (Korea has very limited gatekeeping and patients have substantial freedom of choice). The second reason is that even though medical services are not immediately necessary and LTC hospitals cost more than that of LTC facilities, older people (and their families) prefer LTC hospitals that have strength in providing medical services for potential medical needs since older people's health status is uncertain (Kim et al., Reference Kim, Jung and Kwon2015). The third reason was related to the policy for relieving the financial burden of medical expenditures. Thanks to a ceiling on cumulative out-of-pocket (OOP) payments in the NHI, patients were exempted from paying medical expenses above 2 million Korean won (KRW) as of 2008. However, making LTCH inpatients responsible for their payments only up to a pre-designated ceiling incentivises more patients to choose (social) admissions in LTCHs for the purpose of receiving even simple recuperation or care service rather than medical service. While there is no big difference in the cost of using services from LTCHs and LTCFs due to the exemption of OOP payments for LTCH inpatients, patients with prolonged hospitalisation can use medical services covered under NHI and a pre-designated ceiling on their cumulative OOP payments from LTCHs but no such ceiling on OOP payments from LTCF.
Consequently, patients, who do not require medical services, stay in hospitals unnecessarily (Roh et al., Reference Roh, Sunwoo, Yoon, Won, Lee, Lee, Gi, Jo and Oh2010) and, thereby, cause increasing public expenditures on health insurance (Kim, Reference Kim2015). The two institutions, i.e. LTCHs and LTCFs, are vying for senior patients rather than complementing and integrating different natures of their geriatric services for older adults (Jeon and Kwon, Reference Jeon and Kwon2017).
3. Method
3.1 Data
The data sources used for this study were the NHI Service's (NHIS) claim data of people aged 65 and older in South Korea. The NHIS's claim data include information on the uses of medical services and LTC services covered under the NHIS and information on the insurees' status, such as age, sex, income level, disability, death date, etc. In addition, the database for LTC contains an LTC eligibility checklist, LTC service use and LTC providers. This study has analysed three periods (every six months) of data from January 2008 to June 2009 (i.e. before and after the introduction of LTCI).
3.2 Identification strategy and target population
As shown in Table 1, the LTC eligibility for older people in South Korea is determined by LTC grades based on LTC assessment scores. The criteria and assessment system for LTC eligibility was used for the identification strategy in this research design. When LTCI was introduced in July 2008, LTC grade 3 was granted to applicants who attained a score of 55 points and above, meaning that if applicants did not reach the 55-point threshold, they were disqualified for LTC coverage. The non-eligible group with an LTC score nearing 55 points and the beneficiary group with an LTC score of 55 points shared similar aspects of LTC needs, but the former group was excluded from the policy target. In order to evaluate the effects of LTCI in South Korea, we selected older people with scores of 51 or 52 points as the comparison groupFootnote 1 and those scoring 55 or 56 points as the treatment group.
We conducted an analysis to evaluate the effect of benefits for LTC grade 2 in comparison with that of grade 3. Institutional care services were available for beneficiaries of LTC grade 2 or 1, whereas LTC grade 3 could receive only home care services in general. We identified how the difference in benefit packages between LTC grade 2 and grade 3 affected medical service use. LTC grade 2 was granted to applicants who reached the threshold of 75 points. The same identification strategy as the previous method was applied, i.e. the treatment group was defined by beneficiaries with LTC scores of 75 and 76 points, and the comparison group with LTC scores of 71 and 72 points.Footnote 2
The target population was older people aged 65 years or older who applied for LTC services in 2008. We ruled out those who met the following exclusion criteria. First, people under the age of 65 were excluded from this study. Second, those who died within one year after the introduction of LTCI were excluded to take into account a follow-up period of at least one year. Third, those who applied for LTC services in 2008 but had their grades determined in 2009 were excluded from this study. Lastly, those who omitted their income level and disability data were excluded.
The final inclusion of the target population for this study is shown in Figure 1.
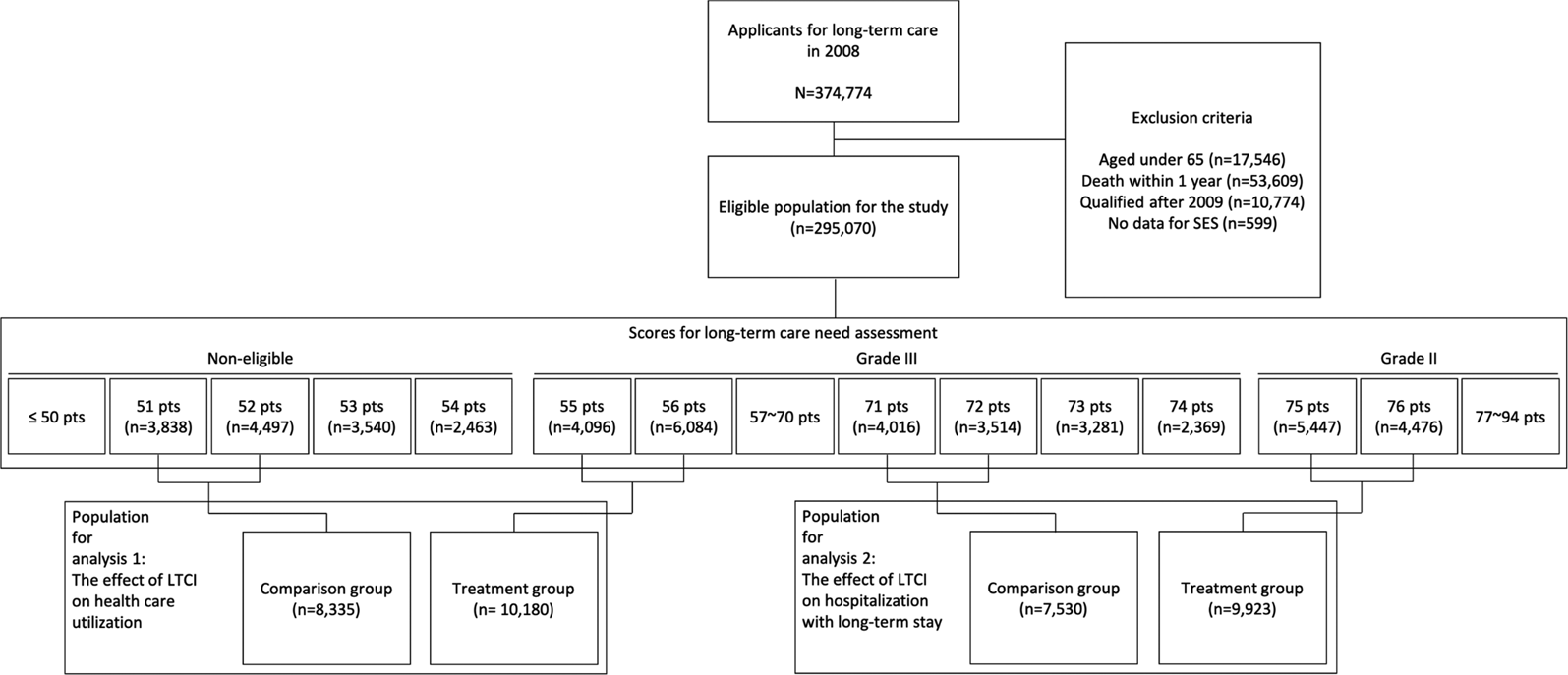
Figure 1. Flow chart of inclusion process for the target population.
3.3 Econometric model
The generalised difference-in-difference (GDD) method was adopted to evaluate the effects of the introduction of LTCI on older people's medical service uses, including outpatient visits, hospitalisations and longer stays in hospitals. In addition, the two-part model was applied since medical expenditures were zero-inflated. The first part estimated the probability of medical service use based on a regression with the logit (or probit) function.Footnote 3 The second part estimated the medical service costs (or the amount of medical services) conditional on having positive costs incurred (or the positive amount of medical services). The second part estimation used the log-transformed dependent variables due to skewed distribution. (Descriptive statistics of dependent variables are provided in the online Appendix.)
Also, two types of analysis were conducted. The first one estimated the effects of the introduction of LTCI by comparing the medical service use by beneficiaries of LTC grade 3 with that of non-beneficiaries. The second one compared the inpatient care uses between LTC grade 2 and grade 3.
Following is the first regression model:
where HUT it is the medical service use by older people (i) at a certain point of time (t); α is the constant; γ t is the time effect; D it is the eligibility for LTC grade 3 by older people (i) at a certain point of time (t); X i is the vector of control variables including age, sex, income level, residential site, Charlson comorbidity index (CCI) and proximity to death.
Following is the second model:
where HADM it is the inpatient services use by older people (i) at a certain point of time (t); α is the constant; γ t is the time effect, D it is the eligibility for LTC grade 2 by older people (i) at a certain point of time (t) and X i is the vector of control variables. Outcome variables (HADM it) of the second model include hospitalisation, length of stay and social admission (hospitalisation for 181 days or longer). Inpatient services included all types of hospitalisation in both acute hospitals and LTCHs. We operationally defined social admission (also known as delayed discharge) as hospitalisation for 181 days or longer to take into account South Korea's disincentive system, which reduces fees to providers in the case of patients hospitalised for more than 181 days.
4. Results
4.1 General characteristics
Table 2 shows the basic characteristics of the target population, with the characteristics of the treatment and comparison groups presented in columns 1 and 2. In the treatment group of LTC grade 3 (scoring 55, 56 points), the probability of becoming eligible for LTC was 89.4%. While it is typical to grant LTC grade 3 to applicants scoring 55 points or higher, there were some exceptional cases, such as failure to submit the required documents or dropping out of the eligibility process in the middle. In these cases, 10.6% of the treatment group became ineligible for LTC despite their 55 points or higher LTC scores. Meanwhile, approximately 23.2% of the comparison group (scoring 51, 52 points) were found to receive LTC grade 3, decided by the LTC eligibility committee in case such applicants' desperate needs for LTC benefits were recognised in spite of their LTC scores lower than 55 points.
Table 2. Basic characteristics
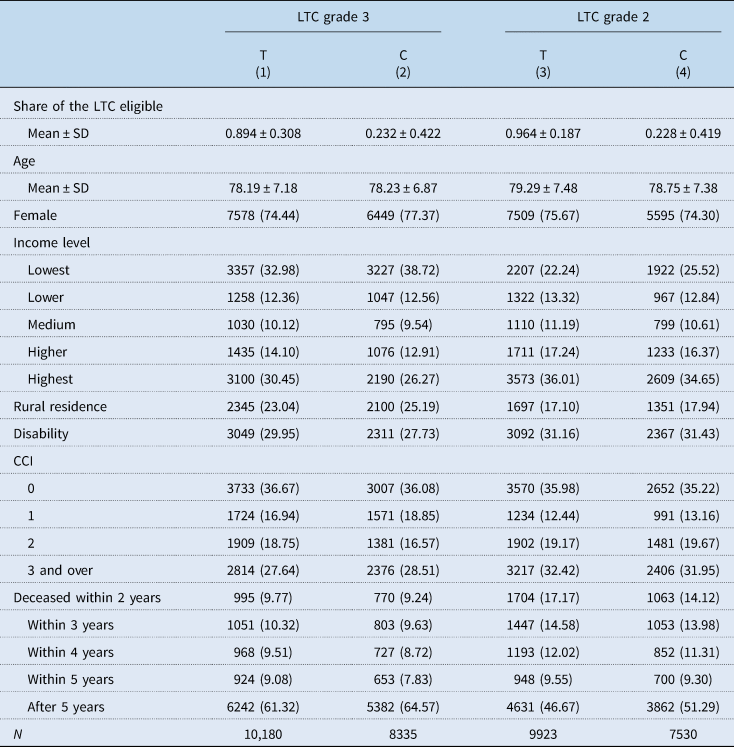
LTC, long-term care; T, treatment group; C, comparison group; SD, standard deviation; CCI, Charlson comorbidity index.
% of N in parentheses.
The characteristics of the treatment and comparison groups analysed to find out the availability of institutional care to beneficiaries are presented in columns 3 and 4. In total, 96.4 and 22.8% of the treatment group (scoring 75, 76 points) and comparison group (scoring 71, 72 points) received LTC grade 2, respectively.
4.2 Impact of the introduction of LTCI on the medical service use
4.2.1 LTC grade 3 vs non-beneficiary
The first four columns in Table 3 show the findings of the two-part model on the effects of the introduction of LTCI. The LTCI itself did not affect medical service use (columns 1 and 2 of Table 3), but the size of medical expenditures of older people who used medical services at least once decreased by 10.6% (column 3 of Table 3). According to the result of the analysis, medical expenditures decreased to 9.4% (column 4 of Table 3). Our analysis also used a log-transformed variable, which added a constant value (+1) to each value of medical expenditure so as not to omit the subjects paying zero value of medical expenditure as a dependent variable. Such analysis did not reveal any statistically significant results from both the pooled ordinary least square (POLS) and the model with fixed effect.
Table 3. Effects of the introduction of LTCI on medical care use (LTC grade 3 vs non-beneficiary)
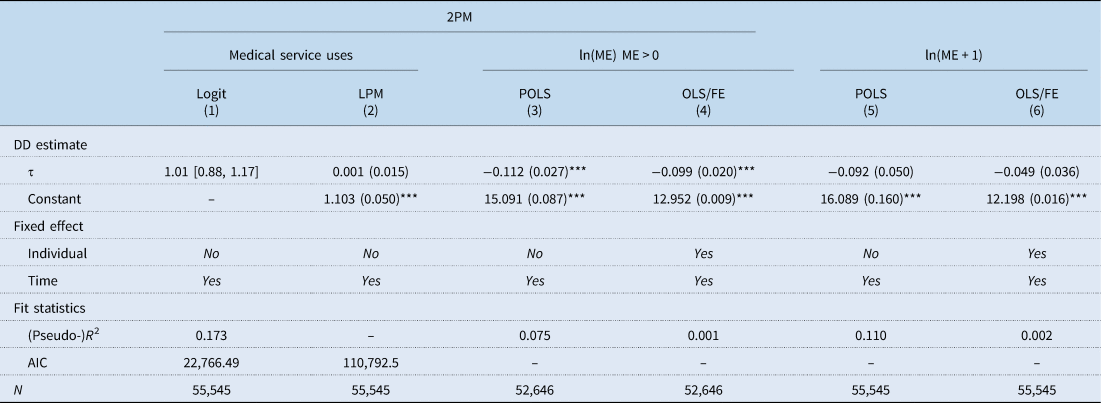
2PM, 2-part model; ln, natural logarithm; ME, medical service expenditure; LPM, linear probability model; POLS, pooled ordinary least square; FE, fixed effect; DD, difference-in-difference; AIC, Akaike information criterion.
Odds ratio presented for logit model (95% confidence limits in square brackets) and coefficients presented for log-transformed HCE (standard error in parentheses).
*Significant at the 5% level (p-value <0.05).
**Significant at the 1% level (p-value <0.01).
***Significant at the 0.1% level (p-value <0.001).
In order to examine the effects on medical service use in more detail, medical services were classified into outpatient and inpatient services. The change in medical service use affected by the LTCI showed the difference between outpatient and inpatient services. With regards to outpatient services (Table 4), the introduction of LTCI did not have an effect on the probability of outpatient visits nor the number of visits. On the other hand, it turned out that the medical expenditure per outpatient visit decreased by 3.0%. Regarding inpatient services (Table 5), the results showed that elderly hospitalisations declined after the introduction of LTCI. According to the difference-in-difference (DD) estimate in the linear probability model (LPM), the probability of hospitalisation decreased by 2.7% (p-value <0.001). The second part analysis of the length of stay and inpatient expenditure showed different results between the POLS and the fixed effect model. The results of POLS regression (columns 3 and 5 of Table 5) showed no effect of the LTCI on the length of stay and inpatient expenditure. However, the fixed effect model showed a statistically significant correlation between the LTCI introduction and a decrease in the length of stay and inpatient expenditure by 6.2 and 9.5%, respectively (columns 4 and 6 in Table 5).
Table 4. Effects of the introduction of LTCI on outpatient service use (LTC grade 3 vs non-beneficiary)
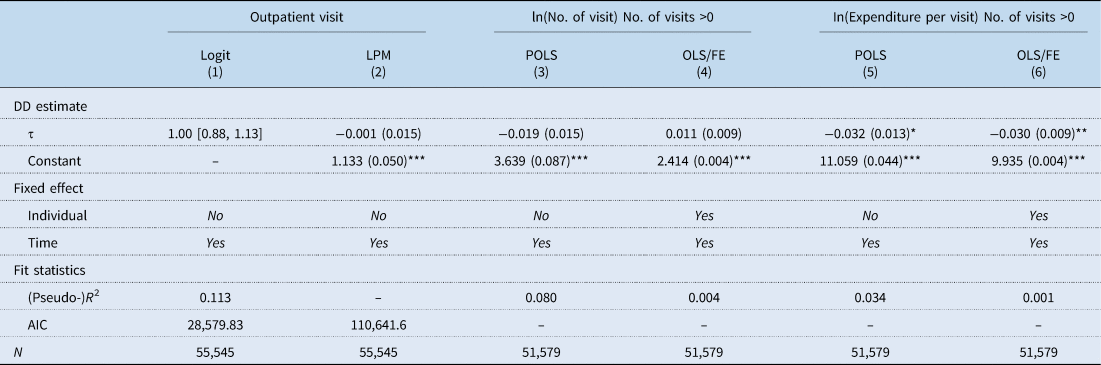
ln, natural logarithm; LPM, linear probability model; POLS, pooled ordinary least square; FE, fixed effect; DD, difference-in-difference; AIC, Akaike information criterion.
Odds ratio presented for logit model (95% confidence limits in square brackets) and coefficients presented for LPM and OLS (standard error in parentheses).
*Significant at the 5% level (p-value <0.05).
**Significant at the 1% level (p-value <0.01).
***Significant at the 0.1% level (p-value <0.001).
Table 5. Effects of the introduction of LTCI on inpatient service use (LTC grade 3 vs non-beneficiary)
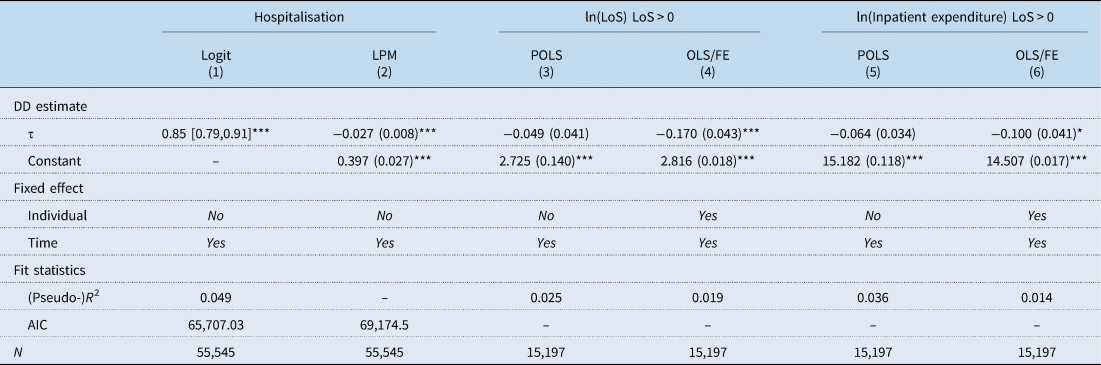
ln, natural logarithm; LoS, length of stay; LPM, linear probability model; POLS, pooled ordinary least square; FE, fixed effect; DD, difference-in-difference; AIC, Akaike information criterion.
Odds ratio presented for logit model (95% confidence limits in square brackets) and coefficients presented for LPM and OLS (standard error in parentheses).
*Significant at the 5% level (p-value <0.05).
**Significant at the 1% level (p-value <0.01).
***Significant at the 0.1% level (p-value <0.001).
4.2.2 LTC grade 2 vs grade 3
The LTCI in South Korea provides different benefit packages depending on recipients' LTC grades. Beneficiaries of LTC grade 2 can receive institutional care, but those of LTC grade 3 are eligible only for home-based care. We identified the effects of institutional care availability on the use of inpatient services by beneficiaries of LTC grade 2 in comparison with those of LTC grade 3. According to Table 6, the availability of institutional care significantly negatively affects on the use of inpatient services as the probability of hospitalisations declined by 6.9%, length of stay by 21.7% and inpatient care expenditure by 21.6%. Lastly, the last two columns of Table 6 provide estimates for the effects of institutional care availability on a longer stay in hospitals, defined by hospitalisation for 181 days or longer. The availability of institutional care correlates with the 1.6% decrease in the probability of older people's long-term hospital stay.
Table 6. Effects of institutional care availability on inpatient service use (LTC grade 2 vs grade 3)

ln, natural logarithm; LoS, length of stay; LPM, linear probability model; POLS, pooled ordinary least square; FE, fixed effect; DD, difference-in-difference; AIC, Akaike information criterion.
Odds ratio presented for logit model (95% confidence limits in square brackets) and coefficients presented for LPM and OLS (standard error in parentheses).
*Significant at the 5% level (p-value <0.05).
**Significant at the 1% level (p-value <0.01).
***Significant at the 0.1% level (p-value <0.001).
4.2.3 Sub-group analysis
In the institutional background, the ceiling on cumulative OOP payments as part of South Korea's health insurance policy was mentioned as an institutional driver for older people's choice of social admissions. However, even after the introduction of LTCI, older people whose cumulative OOP payment exceeds a predefined ceiling may not want to be discharged from the hospital to be admitted to an LTC facility because they can receive a waiver of cost by NHI. Therefore, we conducted a sub-group analysis to see if the effects of the introduction of LTCI on prolonged hospitalisation differ among older people depending on whether their OOP expenses in the hospital exceeding the ceiling or not. For the sub-group analysis, we distinguished patients group exceeding the OOP maximum (2 million KRW, approx. US$1800) from those not exceeding it over a period of t − 1 (1 January 2008–30 June 2008), which is before the introduction of LTCI in South Korea.
With regards to the patient group not exceeding the OOP maximum over a period of t − 1, the sub-group analysis showed similar results to the base analysis, i.e. prolonged hospitalisation decreased [odds ratio (OR): 0.79, p-value = 0.011]. On the other hand, the patient group exceeding the OOP maximum did not show a reduction in prolonged hospitalisation (OR: 0.83, p-value = 0.126) (Table 7).
Table 7. Effects of institutional care availability on hospitalisation with 181 days+: sub-group analysis

Note: t − 1 refers to the first 6 months in 2008, period before introducing the LTCI.
LPM, linear probability model; OOP, out-of-pocket payment; M, million; AIC, Akaike information criterion.
Odds ratio presented for logit model (95% confidence limits in square brackets) and coefficients presented for LPM (standard error in parentheses).
*Significant at the 5% level (p-value <0.05).
**Significant at the 1% level (p-value <0.01).
***Significant at the 0.1% level (p-value <0.001).
5. Robustness check
5.1 Parallel trends
The parallel trend assumption is the most critical assumption to ensure the internal validity of the DD model, i.e. the difference in outcome between the treatment and comparison groups should remain constant over time in the absence of intervention. Therefore, in order to check the potential violations of the parallel trends, we examined the trends in the outcome variables such as the probability of medical service use, hospitalisation and medical expenditure from 1 July 2007 to 30 June 2009, as presented in Figures 2 and 3. Both figures include quarterly average and 95% confidence interval and confirm that the parallel trend assumption is fulfilled.
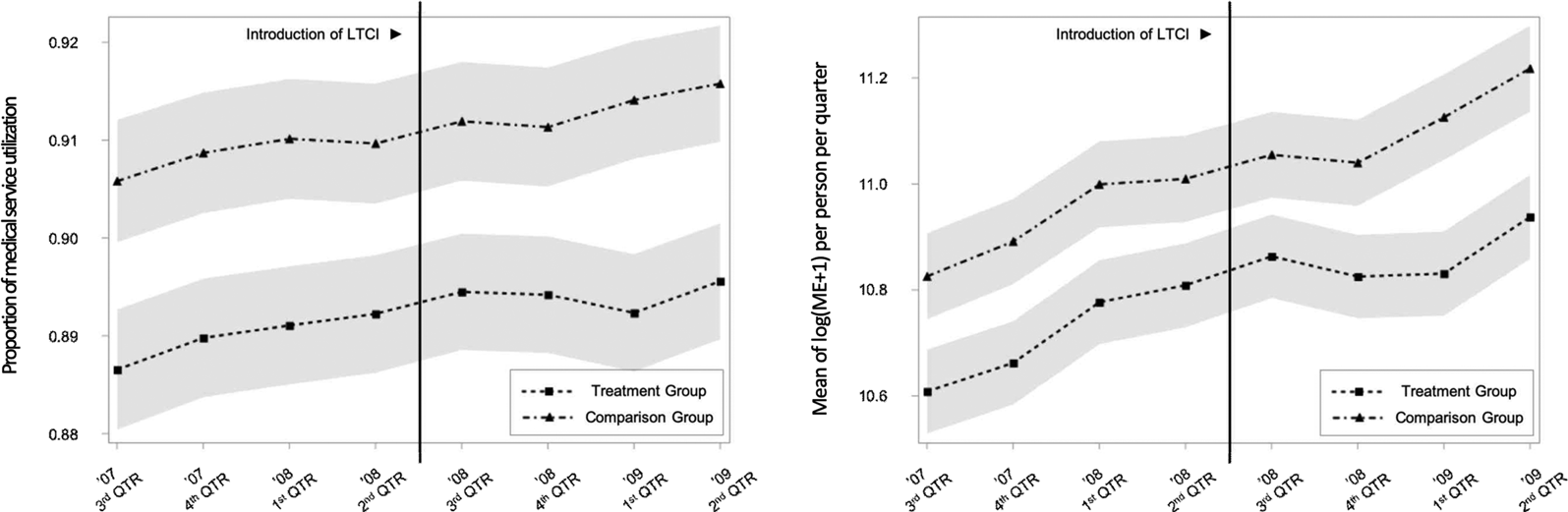
Figure 2. Parallel trends in outcome between the beneficiary of LTC grade 3 vs non-beneficiary.
Note: The grey-shaded area represents the 95% confidence interval.
LTCI, long-term care insurance; ME, medical service expenditure; QTR, quarter.
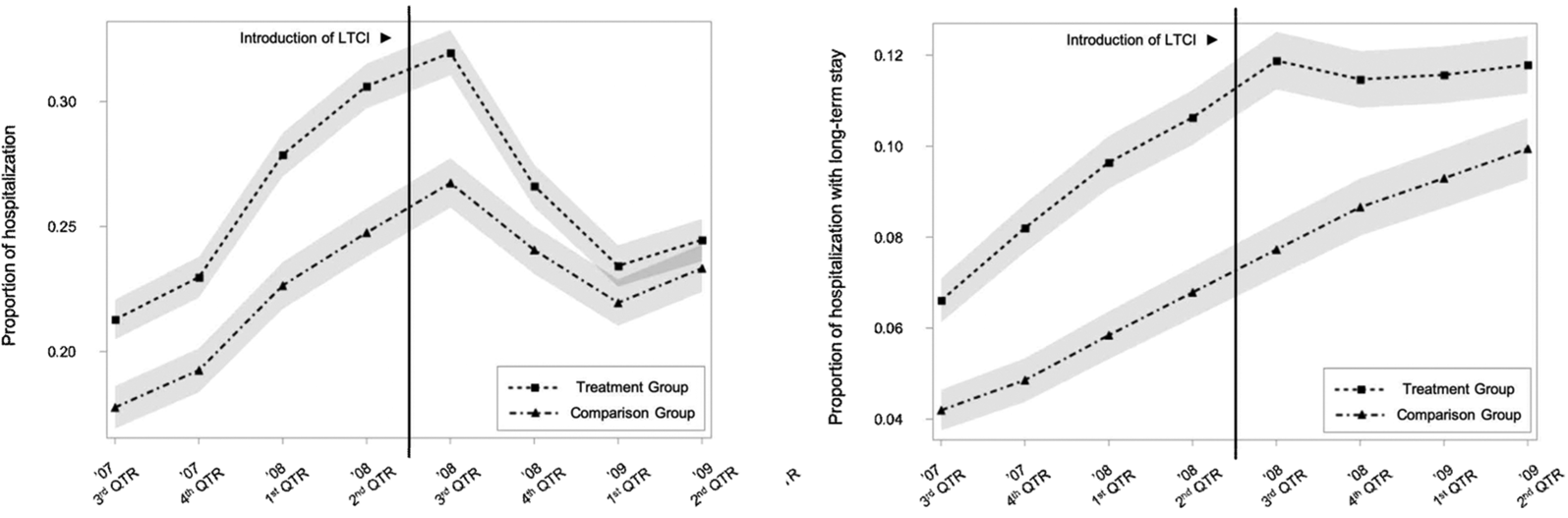
Figure 3. Parallel trends in outcome between the beneficiary of LTC grade 2 vs grade 3.
Note: The grey-shaded area represents the 95% confidence interval.
LTCI, long-term care insurance; QTR, quarter.
5.2 Evaluating the effects of the expansion of population coverage
The population coverage of LTCI in South Korea was expanded by relaxing the eligibility criteria for LTC grade 3 in 2012 and 2013. The LTC approval score for LTC grade 3 was lowered from 55 to 53 in 2012 and 53 to 51 in 2013. We performed a robustness check by comparing the result for 2008 with the results for 2012 and 2013 in order to see if the same results were reproduced. The same identification strategy for the base analysis was applied. Accordingly, the applicants with LTC approval scores of 53, 54 points in 2012 (or 51, 52 points in 2013) were set up as a treatment group, while those with LTC approval scores of 49, 50 points in 2012 (or 47, 48 points in 2013) as a comparison group. However, comparing LTC grade 2 and grade 3 was not feasible because there was no change in the eligibility for LTC grade 2. As demonstrated in Table 8, the robustness check results were similar to the base analysis results despite a slight difference in the magnitude of coefficients. The availability of LTC services had no effect on the probability of medical service use while associated with a decrease in the elderly's medical expenditures by 9.4, 10.5 and 8.5% in 2008, 2012 and 2013, respectively.
Table 8. Effects of the expansion of population coverage in 2012 and 2013
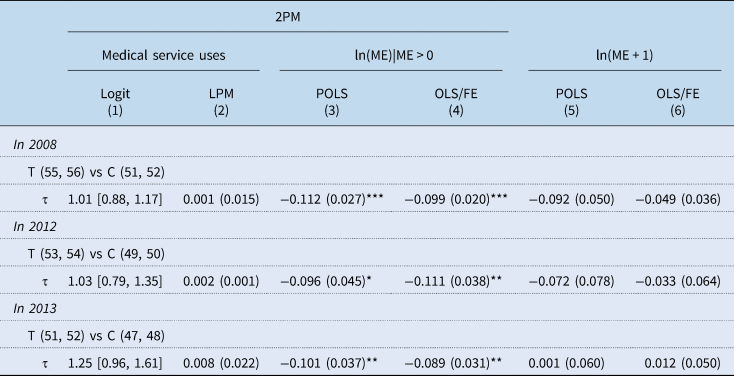
2PM, 2-part model; ln, natural logarithm; ME, medical service expenditure; LPM, linear probability model; POLS, pooled ordinary least square; FE, fixed effect; T, treatment group; C, comparison group.
Odds ratio presented for logit model (95% confidence limits in square brackets) and coefficients presented for OLS (standard error in parentheses).
*Significant at the 5% level (p-value <0.05).
**Significant at the 1% level (p-value <0.01).
***Significant at the 0.1% level (p-value <0.001).
6. Discussion
The result of this study showed that the introduction of LTCI did not affect the medical service use but decreased the medical expenditures of older people who used medical services at least once by 9.4% (estimates from POLS: 10.6%). These results were similar to those of the previous analysis exhibiting the effects of public LTC subsidy for home care on the reduction of medical expenditures by approximately 11% (Costa-Font et al., Reference Costa-Font, Jimenez-Martin and Vilaplana2018).
For a better understanding, we divided medical services into outpatient and inpatient services and estimated the effects of the LTCI on the uses of each service. According to the result of our analysis, the introduction of LTCI affected the use of outpatient and inpatient services differently. First of all, the introduction of LTCI showed no significant effect on outpatient service in terms of the possibility of medical service uses and the number of visits but brought about a decrease in medical expenditures per visit. On the other hand, the introduction of LTCI reduced the rate of inpatient hospitalisations by 2.7%. It revealed a statistically significant impact on decreasing inpatients' length of hospital stay and hospital expenses, confirming a negative correlation between LTC service and inpatient service. In conclusion, the introduction of LTCI showed a significant decline in the use of inpatient services while not having much influence on outpatient services in South Korea.
A previous study has reported that outpatient services could show a tendency to increase due to the introduction of LTCI. According to a study by Costa-Font et al. (Reference Costa-Font, Jimenez-Martin and Vilaplana2018), the use of LTC services increased the number of hospital visits for outpatient services and primary health care expenditures, revealing a potential positive correlation between LTC service and outpatient service (Costa-Font et al., Reference Costa-Font, Jimenez-Martin and Vilaplana2018). Such findings may be based on the observation that the introduction of LTC service led to the growing use of medical services as patients who had difficulty moving around have better access to care, and those who have not yet recognised their disease status become conscious of their medical needs. However, unlike the previous study, our analysis could not ascertain the effects of LTCI on growing outpatient services.
Meanwhile, the decrease in inpatient services after the introduction of LTCI implies that LTC service and medical service are substitutes for each other. Especially, in an analysis looking at eligible applicants for LTC grade 3 who can use home care services only and not institutional care services, it was found that the use of inpatient services by LTC grade 3 beneficiaries decreased, meaning that home care services of LTCI replaced inpatient services (covered by NHI). The fact that LTC service is a substitute for medical service was confirmed by previous studies (Fernandez and Forder, Reference Fernandez and Forder2008; Lichtenberg, Reference Lichtenberg2012; Costa-Font et al., Reference Costa-Font, Jimenez-Martin and Vilaplana2018), which showed that public scheme for LTC service enabled older patients to opt for home-based care and no longer remain in the hospital and be discharged earlier. The fact that LTC service is the substitute for medical service was also confirmed by an analysis of eligible applicants for LTC grade 2 who could use both institutional care and home care in Korea. In particular, the correlation between the LTCI introduction and the decrease in social admissions (defined in this study as hospitalisation for 181 days or longer) was identified. Most previous studies, which explain the relationship between LTC service and medical care, report the effect of LTC services on the decline in inpatient care and bed blocking (Forder, Reference Forder2009; Gaughan et al., Reference Gaughan, Gravelle and Siciliani2015).
Bringing on LTC services as the substitute for social admissions by older people at hospitals, a social problem and a big concern for NHI, was one of the expected effects of the public LTCI in South Korea. Still, there remains a lack of empirical evidence on reducing social admission, even though one relevant study showed the descriptive trend of decreasing long-term hospitalisations in LTCH after the LTCI introduction (Jeon et al., Reference Jeon, Kim and Kwon2016). Long-term hospitalisation was the only way to receive publicly subsidised care under NHI before the LTCI introduction. The introduction of public LTCI provided an alternative to institutional services that older people with LTC needs but no medical needs could choose. According to a previous study examining the composition of patients in LTCH, it was found that a significant number of patients were hospitalised for a long time without medical needs (Kim et al., Reference Kim, Jung and Kwon2015). LTCF could be more attractive for these patients. The result of our study has suggested the possibility of some achievements of a decline in social admissions as a result of the LTCI introduction. In addition, one notable outcome of this study was that the decline in social admissions caused by the introduction of LTCI was not observed among those who benefit from the ceiling on OOP payment. In other words, the patient group exceeding the OOP maximum in the hospital over a period prior to the introduction of LTCI did not show a reduction in prolonged hospitalisation. The OOP payment ceiling policy is one of the representative protection mechanisms of NHI to relieve severely ill patients of their burden of catastrophic health expenditures. However, once the inpatient expenses of a long-stay patient exceed a pre-designated ceiling (as a result of prolonged hospitalisation), s/he becomes exempt from hospital costs and has little financial incentive to be discharged. The current situation in which the OOP payment ceiling policy discourages older people from shifting to LTC services by detracting the cost advantage of LTCF is an unexpected consequence that undermines social efficiency in the Korean health system for older people. Therefore, it is urgent to revise the OOP payment ceiling policy to reduce social admissions and prevent unnecessary hospitalisations associated with no acute medical needs.
Our study has limitations. First is the possibility of underestimation of the effect of LTCI introduction. Although the LTC assessment score of 55 points is the minimum criteria for LTC grade 3, some applicants scoring less than 54 points have attained LTC grade 3 approved by the assessment committee. For this reason, 23.2% of applicants scoring 51 or 52 points, initially defined as the non-beneficiaries group, were granted LTC grade 3. Hence, there is a possibility that the effect of LTCI introduction was underestimated by the GDD method. Still, the estimated result is derived from the intention-to-treat (ITT) method, which evaluates the policy effects on the basis of the initial policy intentions (LTC approval scores of 55 points and 75 points in this study). The ITT method is stricter than the per protocol method, which evaluates the policy effects based on the possibility of actually receiving benefits.
Second, our study does not grasp the effects of the introduction of LTCI on the health of older people as the policy's medium to long-term effect. This study has identified the effects of the LTCI system on the uses of LTC services and medical services, including longer hospital stays, but has not been able to understand the effects on health, which requires a long observation period. In this case, a cross-over from the non-beneficiary group to the beneficiary group becomes a huge problem. For such reason, our study had limitations, such as observing the transition of medical service use over only one year since the implementation of the LTCI policy and identifying the policy's short-term effects.
7. Conclusion
This study estimated the effects of the introduction of LTCI in 2008 on the uses of LTC services and medical services using the GDD method. In particular, our study has assessed the LTCI introduction effects with a focus on older people's longer hospital stays. Even in the case of South Korea, LTC services were found to be a substitute for medical services and especially effective in reducing older people's prolonged hospitalisations, which have become a major social problem. However, the reducing effect of prolonged hospitalisations caused by the introduction of LTCI was not observed from beneficiaries of the OOP payment ceiling policy. It thus seemed inevitable to revise the OOP payment ceiling policy given the distributional inefficiency arising from social admissions.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S174413312200024X.
Financial support
The authors received no financial support for the research, authorship and/or publication of this article.
Conflict of interest
No competing financial interests exist.














