Introduction
Radiotherapy is a vital cancer treatment modality, enhanced by technological advancements like the Elekta Versa HD linear accelerator and its X-ray Volume Imaging (XVI) system. These innovations enable precise and adaptive treatments by allowing real-time monitoring of internal motion. Elekta’s XVI imaging system enhances treatment precision by improving patient positioning, supporting techniques that help reduce radiation dose to organs such as the heart and lung in left-sided breast cancer. 1
This study identified an issue of higher-than-expected frame counts during Cone Beam Computed Tomography (CBCT) exposures at Singleton Hospital, introducing a variation into the expected imaging dose delivered to patients. Imaging dose from XVI is typically low compared to treatment dose, unnecessary variation may contribute to cumulative exposure to healthy tissues and the appropriate monitoring should be done to uphold radiation protection principles. 2 This investigation focusses on higher-than-expected frames per scan which can cause dose uncertainty for every patient. While this problem does not affect patient set-up accuracy, operational efficiency, or notable image quality as confirmed by radiographers, it can indicate underlying issues such as system inefficiencies, increased patient exposure to radiation or the need for protocol optimisation.
This investigation aimed to analyse frame count data from multiple linacs, identify conditions leading to increased counts and evaluate their impact. Addressing these discrepancies is crucial for ensuring precise, safe, and effective radiotherapy, thereby enhancing patient care and treatment outcomes.
Method
The issue of higher-than-expected frame counts during Cone Beam Computed Tomography (CBCT) exposures at Singleton Hospital was initially identified by radiographers in various UK centres. Alerts indicating that delivered frames exceeded the expected number by over 10 % were observed, potentially leading to increased patient radiation doses.
To address this, log files were gathered from the Elekta XVI system (R5.07) and followed with the flow chart in Figure 1 to record instances when frame counts exceed Elekta’s 10 % tolerance threshold. 3

Figure 1. Flow chart of data collection steps method.
A Python script was developed using Spyder 5.5.5 to automate the extraction and analysis of relevant information from these logs. This script matched occurrences of excessive frame counts with specific patients and CBCT presets by aligning date and time stamps from multiple log files.
AI tools enhanced our data processing capabilities and enabled rapid generation of visualisations such as histograms to assess the frequencies of the errors. Patient confidentiality was ensured by anonymising identifiable information before utilising AI tools. Additionally, the delivered imaging dose was calculated per CBCT protocol using established measurements and effective dose calculations from PCXMC software 4 , accounting for variations in exposure.
This method allowed the identification of the conditions that led to increased frame counts, the evaluation of their impact on patient safety and system performance, and the consideration of necessary adjustments to protocols or system settings to mitigate the issue.
Results & Discussion
To focus the scope of data analysis for this report, only the 3 imaging presets associated with the highest frame counts on a single linac system (Linac 2 at Singleton Hospital) are presented. Linac 2 was selected as it showed the highest frequency of higher-than-expected frame counts in the log data. This is likely due to its more frequent use for breast cancer patients, whose imaging presets involve higher gantry speeds and common pauses during imaging of patients due to Deep Inspiration Breath-hold (DIBH) strategies. This targeted analysis is expected to provide clear insights into the specific conditions under which these errors are most prevalent.
Breast Linac (Versa HD)
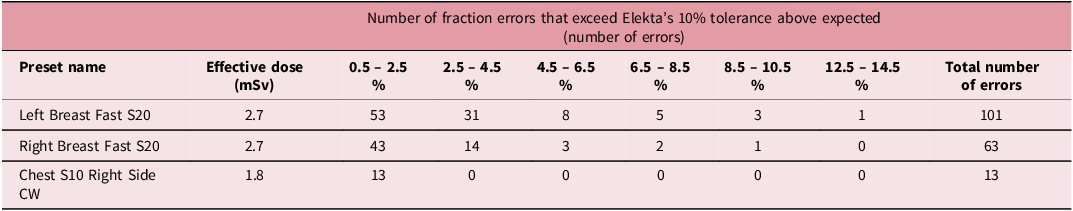
Figure 2 shows a histogram for the locally developed left breast protocol which has the highest occurrences of the frame error. A noticeable factor to consider is that this is a fast protocol, meaning the gantry speed is 360 degrees per minute compared to 180 degrees per minute which is set for all non-breast protocols. The percentage range above the tolerance is 0.5 % to 13.6%. Between 0.5% and 2.5%, 53 fractions were captured, and between 2.5–4.5% there were 31 fractions. The left breast protocol preset alone has 101 entries, which is more than the total number of entries for all presets combined on each linac without fast protocols enabled.
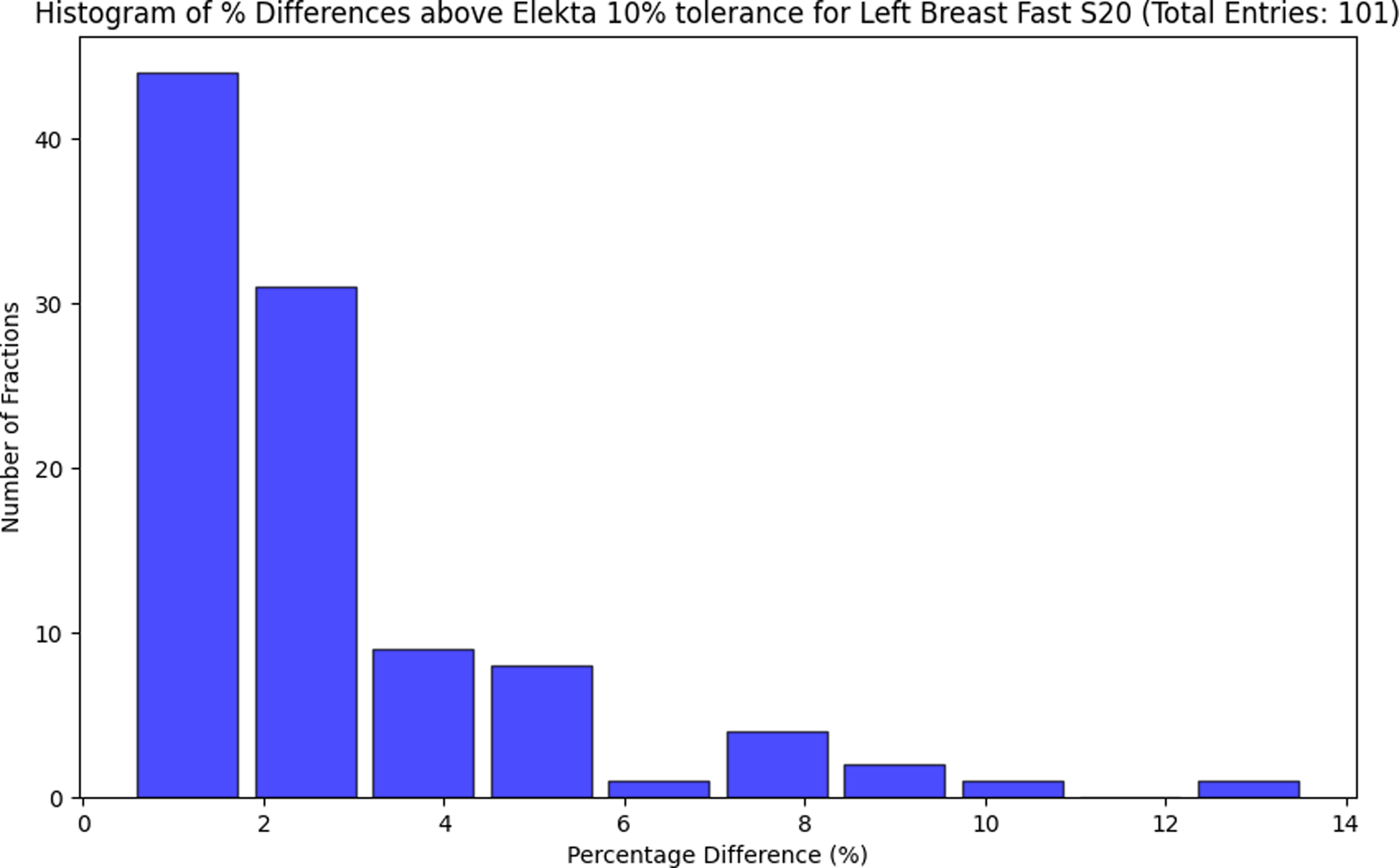
Figure 2. Histogram showing the number of affected fractions for each frame percentage difference group for the Breast linac Left Breast Fast S20 preset.
Figure 3 shows a fast breast preset for the right side for comparison to the left shown in Figure 2. The percentage difference ranges between 0.5% and 9.1% and there are noticeably less entries, 63 in comparison to 101 in Figure 2. The left breast technique uses the DIBH technique to reduce dose to the heart in comparison to the right breast technique.

Figure 3. Histogram showing the number of affected fractions for each frame percentage difference group for the breast linac Right Breast Fast S20 preset.
Figure 4 shows 13 entries for the ‘Chest S10 Right Side CW’ protocol. The percentage difference ranges between 0.3% and 1.5%. As previous figures show, most entries here are marginally above the Elekta tolerance where most in Figure 4 are under 0.9 %. Although it’s only just above the tolerance, cumulatively across each linac, this is a consistent occurrence.
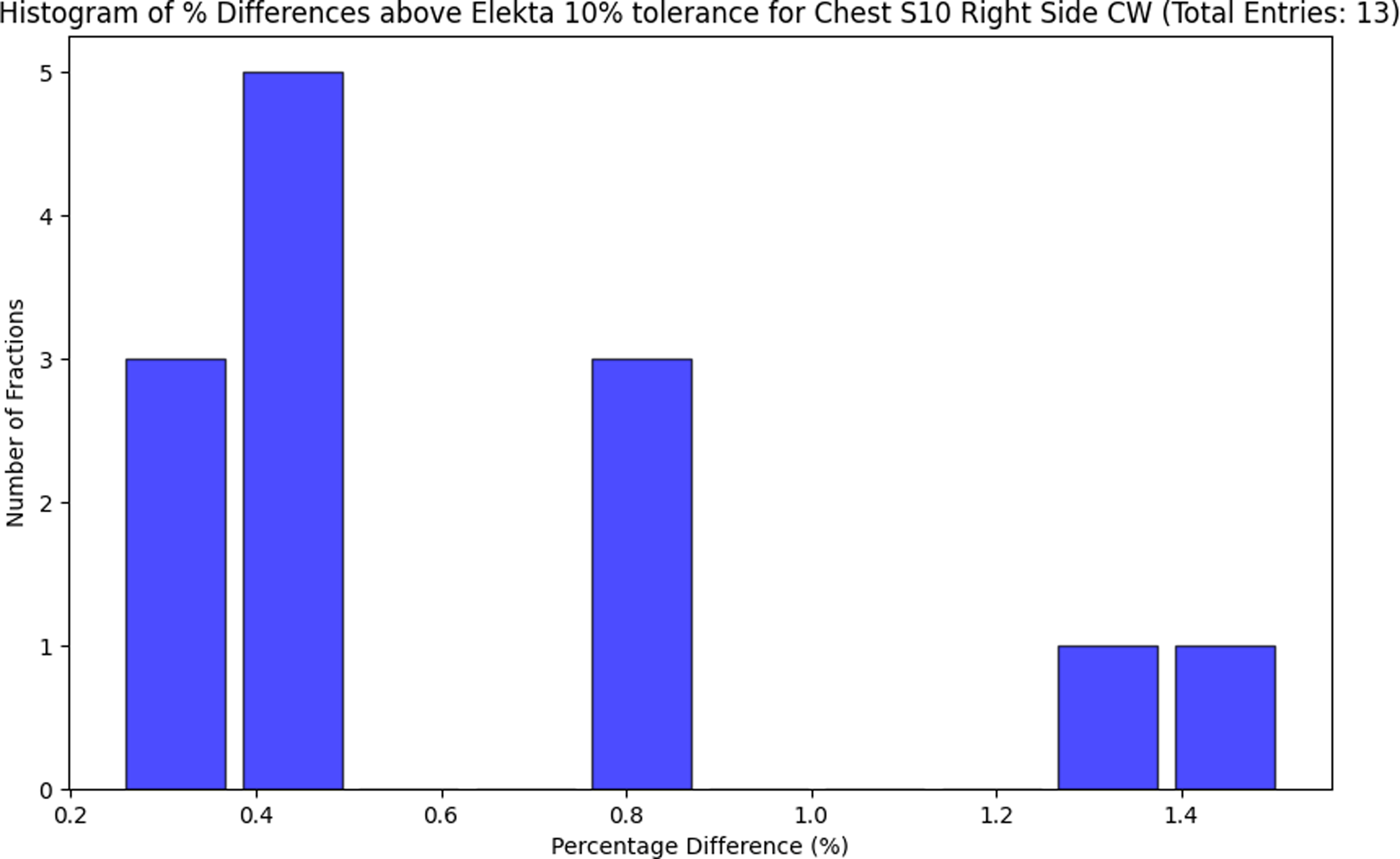
Figure 4. Histogram showing the number of affected fractions for each frame percentage difference group for the breast linac Chest S10 Right Side CW preset.
Table 1 shows the top 3 presets for the breast linac. It displays data for the 3 most affected presets, specifically analysing the Left Breast Fast S20, Right Breast Fast S20, and Chest S10 Right Side CW. Each preset indicates an effective dose in millisieverts (mSv) with further error analysis across several percentage ranges from 0.5% to 14.5% above the Elekta 10 % tolerance. Both fast breast protocols have a high number of entries marginally above the Elekta tolerances, which has a very low impact regarding effective dose on the fractions given to the patient. The potential reason for this similar occurrence with fast breast protocols is that there are pauses during imaging; this is due to breast patients using the DIBH technique and gantry speed.
Table 1. Total number of errors for 3 highest preset for the breast linac
Other presets not covered in this report also exhibit the same pattern, possibly increasing the total imaging dose. The analysed presets exceeded Elekta’s tolerance levels, suggesting uncertainty with the XVI system may be consistently delivering more frames than the nominal value set in the imaging preset.
Following the initial analysis on Linac 2, the same audit method was applied to the remaining clinical linacs at Singleton Hospital. A total of 417 out of approximately 24,000 CBCT imaging fractions (1.7 %) exceeded Elekta’s 10 % frame count tolerance. The maximum excess dose delivered in a single imaging fraction was 0.7 mSv, which is equivalent to approximately 3 months of background radiation. 5 For context, the affected patient received 2.7 mSv as part of their standard imaging procedure and 3.4 mSv in total during that session. Although these excess doses are minor in relation to therapeutic doses, they still highlight the importance of maintaining imaging exposures As Low As Reasonably Practicable (ALARP). Notably, image quality and treatment delivery were unaffected.
The excess frames can be seen on all clinical linacs at the hospital, and it has been decided to perform regular frame count audits to actively monitor this issue and further investigate how to reduce the number of excess frames on all protocols. This ensures optimal imaging accuracy and compliance with IR(ME)R 24, Regulation 11 and 12. 6
Conclusion
This study has highlighted the importance of closely monitoring and managing XVI frame counts within Elekta systems at Singleton Hospital to ensure compliance with IR(ME)R 2024. All local linacs deliver excess frame counts, showing recurrent deviations that exceeded Elekta’s specified tolerance for frames of 10 %. 3
These deviations are not isolated incidents but appear to be indicative of potential systemic issues related to the design of the XVI system. For instance, the data analysis from the breast linac has shown an unusually high number of frame count errors, particularly in fast protocol imaging for breasts. However, the exact reasons behind this occurrence on all linacs warrants further study. High gantry rotation speed in fast imaging protocols may be a contributing factor.
The manufacturer, Elekta, is aware of the problem and solutions are being developed. Our study suggests that the regular frame count audit should be repeated routinely to actively monitor this issue and ensure that frame counts remain within expected thresholds for safe and effective patient care.
Competing interests
The authors declare no conflict of interest.







