Donepezil was launched in the UK by Pfizer in March 1997 as the first readily available pharmacological treatment to slow the rate of cognitive decline in Alzheimer's disease Donepezil increases the available acetylcholine by inhibition of the enzyme acetylcholinesterase (AChE). This was followed in 1998 by the launch of rivastigmine by Novartis and in 2000 by galantamine from Shire Pharmaceuticals. There is also evidence that these drugs may have some benefit in the cognitive decline associated with cerebrovascular dementia (Reference Malouf and BirksMalouf & Birks, 2004) and behavioural disturbance in Lewy body dementia (Reference McKeith, Del Ser and SpanoMcKeith et al, 2000).
About the time of the launch of these drugs there were a number of initiatives designed to improve the care of older adults with mental health problems. These included the Forget Me Not reports (Audit Commission, 2000, 2002) and the National Service Framework for Older People (Department of Health, 2001). Arguably, however, it was the review of the AChE inhibitors by the National Institute for Clinical Excellence (NICE) in January 2001 that brought a new mood of optimism in the diagnosis and management of dementia (Reference O'Brien and BallardO’Brien & Ballard, 2001). NICE recommended that the three drugs should be available for National Health Service (NHS) patients with mild or moderate Alzheimer's disease, whose Mini-Mental State Examination (MMSE; Reference Folstein, Folstein and McHughFolstein et al, 1975) score is above 12, with an assessment of effectiveness after 2–4 months. The value of these drugs in other forms of dementia was not assessed.
The advent of treatments that are both effective and available on the NHS for early Alzheimer's disease should have led to a profound alteration in patterns of referral from primary care to specialist services for patients with dementia to allow diagnosis and initiation of treatment early in their illness. This effect has not, to our knowledge, ever been studied. In addition, it is possible that the proportion of dementias diagnosed as Alzheimer's, vascular, Lewy body, etc. may have altered since the publication of the NICE guidelines, either because of a different patient population being referred or to maximise the use of the AChE inhibitors. The impact of the NICE recommendations on healthcare provision has recently been brought into question (Reference Sheldon, Cullum and DawsonSheldon et al, 2004; Reference WhiteWhite, 2004), and the efficacy of AChE inhibitors continues to be debated (AD2000 Collaborative Group, 2004).
Old age psychiatry services in the West Suffolk area cover a mixed urban and rural population with approximately 42 000 people aged 65 years and over. This study examines the effect the availability of the AChE inhibitors and the publication of the NICE guidelines have had on referrals to old age psychiatrists in the West Suffolk region from primary care, examining the MMSE score on referral, diagnosis and the use of AChE inhibitors. The primary null hypothesis is that the MMSE scores at referral have not changed between 1996 and 2003.
Method
We retrospectively examined records of all patients referred from primary care to specialist old age psychiatry services in West Suffolk during two 6-month periods - from July to December 1996, before AChE inhibitors were available, and the same months in 2003. The details of all patients referred from primary care are kept centrally and subsequent records are computerised. We looked at the diagnoses for all new referrals following the patient's first appointment and collected data from the record of this first appointment if the diagnosis included cognitive impairment thought to be a result of any form of dementia. This would include those patients diagnosed with mild cognitive impairment, although this was not used clinically.
For this study, we obtained patients’ age and gender, recorded diagnosis, MMSE score if measured and whether an AChE inhibitor was prescribed at the first consultation. If the MMSE score was out of less than 30 (owing, for example, to poor eyesight) the score was converted to an equivalent score out of 30. The MMSE scores in the two samples were compared with a two-tailed Student's t-test, and the diagnoses compared with a χ2 test.
Results
In the first sample (6 months in 1996), 237 new patients were referred to the old age psychiatry service. Of these, 7 did not see an old age psychiatrist (3 died, 1 was admitted to the acute hospital, 3 records were not available) and of the remaining 230, 112 had a new diagnosis of dementia at referral (40 men (36%) and 72 women (64%)). The mean age was 81.7 years, with a range of 66-96 years. The MMSE scores were available for 86 patients (77%).
In the second sample (6 months in 2003), 275 new patients were referred. Of these, 19 did not see an old age psychiatrist (2 died, 3 were admitted to the acute hospital, 4 were seen in a different area, 7 were seen by other professionals and no records were available for 3). Of the remaining 256 patients, 148 had a new diagnosis of dementia (62 men (42%) and 86 women (58%)). The mean age of the second sample was 81.6 years with a range of 60-97 years. The MMSE scores were available for 133 patients (90%).
The MMSE scores increased from a mean score of 18.8 (range 2-27, s.d.=6.32) in 1996 to a mean score of 21.5 (range 8-29, s.d.=4.95) in 2003 (P=0.0005; see Fig. 1). The diagnoses in the two samples are recorded in Table 1 and show considerable similarity between the two samples, with Alzheimer's disease as the most common (55% and 49%, NS) followed by vascular dementia (26% and 30%, NS) and mixed dementia.
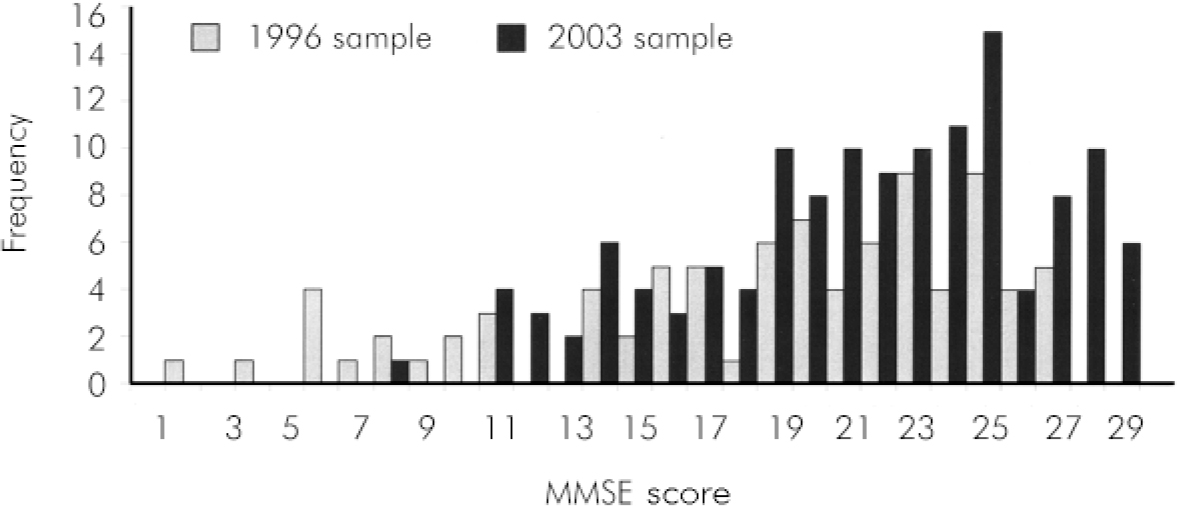
Fig. 1. Frequency of Mini-Mental State Examination (MMSE) scores in the 1996 and 2003 samples
Table 1. Diagnoses in the 1996 and 2003 samples
| Diagnosis* | 1996 sample n (%) | 2003 sample n (%) |
|---|---|---|
| Alzheimer's disease | 62 (55) | 73 (49) |
| Vascular dementia | 29 (26) | 45 (30) |
| Mixed dementia | 5 (4.5) | 6 (4.1) |
| Lewy body dementia | 5 (4.5) | 5 (3.4) |
| Frontotemporal dementia | 1 (0.89) | 2 (1.4) |
| Unknown | 10 (8.9) | 17 (11.5) |
| Total | 112 | 148 |
A total of 52 of 148 patients with a new diagnosis of dementia (2003 sample) were prescribed an AChE inhibitor at the first consultation, 45 donepezil (30%), 5 rivastigmine (3.4%) and 2 galantamine (1.4%); 96 patients were not prescribed these medications (65%). There were 51 recorded MMSE scores in those patients prescribed AChE inhibitors with a mean of 23.1 (s.d.=3.76), and 82 recorded MMSE scores in patients not prescribed these drugs, with a lower mean of 20.6 (s.d.=5.36; P=0.004).
AChE inhibitors were prescribed for 43 patients with Alzheimer's disease (61.4% of diagnostic group), 4 patients with vascular dementia (8.9%), 3 patients with Lewy body dementia (60%), 2 patients with an unknown diagnosis (11.7%) but no patient with mixed dementia or frontotemporal dementia.
Of those patients to whom the NICE guidelines would apply (a diagnosis of Alzheimer's dementia and a MMSE score above 12, total number=72), 42 (58%) received a prescription for an AChE inhibitor after the first consultation.
Discussion
There has been a consistent campaign through the Audit Commission's reports and the National Service Framework for Older People for the earlier diagnosis and treatment of dementia, a key aim if the NICE recommendations for the use of AChE are to be implemented. This study is the first to examine the changing pattern of referrals from primary care to specialist services since the NICE guidelines were published in 2001 and confirms that patients are being referred for specialist treatment earlier in the course of the disease.
Overall, the number of new referrals of patients with dementia rose between 1996 and 2003 from 112 to 148, a rise of approximately 30%. It is beyond the scope of this paper to examine the longer term trends in referring to specialist services, although clearly there are resource implications for the service if this referral rate continues to rise. The MMSE is a widely used guide to the severity of cognitive impairment in dementia and there was a strongly statistically significant rise in the MMSE score between the two samples, from 18.8 to 21.5. The study included all patients whose assessment led to a diagnosis of cognitive impairment secondary to a process of dementia, and the wide range of MMSE scores in both samples shows that the diagnosis is based on factors other than simply the MMSE score itself.
The number of patients seen initially by a healthcare professional other than a doctor, such as a community psychiatric nurse, increased between 1996 and 2003 and could be a source of bias if these patients had more severe dementia. It was usual practice, however, in this area for patients without a formal diagnosis of dementia to see a medical professional initially for diagnosis and, when available, consideration of medication. The service model remained identical between the sample periods, with a slight expansion in consultant numbers that we consider unlikely to substantially influence referral patterns.
More patients in 2003 had their cognitive function assessed formally with the MMSE than in 1996, which is likely to be in part a response to the need to assess cognitive decline more accurately to determine the effectiveness of medication. Reasons for not using the MMSE were not recorded but would include failure of patients to cooperate with testing, severe dementia and prominent language skill deficits. The different use of the MMSE in the two samples would therefore tend to decrease any difference found through an apparent raising of the mean MMSE scores in 1996.
The mean age at referral remained similar between 1996 and 2003, as did the proportion of different diagnoses causing dementia. This suggests that there has not been a change in the way patients are diagnosed in order to facilitate the use of the AChE inhibitors.
The patients who received AChE inhibitors had a higher mean MMSE score than those in the 2003 sample who did not, although the mean MMSE score was still 20.6 in those not prescribed AChE inhibitors, which is well within the current NICE guidelines for patients with Alzheimer's disease. Reasons for non-prescription were not examined formally but included patient preference, contraindications and further investigations. Overall, 58% of patients who would have been eligible for AChE inhibitors received them at first consultation.
This study shows that between 1996 and 2003 more people with suspected dementia were referred to specialist services and diagnosed earlier in their illness. A study like this is unable to directly attribute the cause of this change to NICE guidelines or associated initiatives, but it is clearly encouraging to specialists in this field that patients are seen earlier when treatments may have significant benefit to their lives.
Declaration of interest
None.





eLetters
No eLetters have been published for this article.