What is already known on this subject?
• There is a growing concern about the mental health and well-being of children and young people (CYP) in the UK, with increasing demand for counselling services, hospital admissions for self-harm and referrals to specialist Child and Adolescent Mental Health Services.
• Few national data on trends or the prevalence of psychological distress or mental health conditions among CYP have been published in the UK since 2007.
What this study adds
• Our study found a striking increase in the reported prevalence of long-standing mental health conditions since 1995.
• There was no consistent increase in reported psychological distress among CYP over the last two decades, when measured using scores in validated questionnaires.
• However, there was some evidence of worsening trends in psychological distress and well-being of young adults in recent years (since 2011).
Introduction
There has been a growing global concern about the mental health and well-being of children and young people (CYP) (0–24 years). Increasing rates of anxiety and depression have been reported among adolescents and young adults in a number of developed countries, 1990–2010, although wide variation exists between different countries (Murray et al., Reference Murray, Vos, Lozano, Naghavi, Flaxman, Michaud, Ezzati, Shibuya, Salomon, Abdalla, Aboyans, Abraham, Ackerman, Aggarwal, Ahn, Ali, Alvarado, Anderson, Anderson, Andrews, Atkinson, Baddour, Bahalim, Barker-Collo, Barrero, Bartels, Basáñez, Baxter, Bell, Benjamin, Bennett, Bernabé, Bhalla, Bhandari, Bikbov, Bin Abdulhak, Birbeck, Black, Blencowe, Blore, Blyth, Bolliger, Bonaventure, Boufous, Bourne, Boussinesq, Braithwaite, Brayne, Bridgett, Brooker, Brooks, Brugha, Bryan-Hancock, Bucello, Buchbinder, Buckle, Budke, Burch, Burney, Burstein, Calabria, Campbell, Canter, Carabin, Carapetis, Carmona, Cella, Charlson, Chen, Cheng, Chou, Chugh, Coffeng, Colan, Colquhoun, Colson, Condon, Connor, Cooper, Corriere, Cortinovis, de Vaccaro, Couser, Cowie, Criqui, Cross, Dabhadkar, Dahiya, Dahodwala, Damsere-Derry, Danaei, Davis, De Leo, Degenhardt, Dellavalle, Delossantos, Denenberg, Derrett, Des Jarlais, Dharmaratne, Dherani, Diaz-Torne, Dolk, Dorsey, Driscoll, Duber, Ebel, Edmond, Elbaz, Ali, Erskine, Erwin, Espindola, Ewoigbokhan, Farzadfar, Feigin, Felson, Ferrari, Ferri, Fèvre, Finucane, Flaxman, Flood, Foreman, Forouzanfar, Fowkes, Fransen, Freeman, Gabbe, Gabriel, Gakidou, Ganatra, Garcia, Gaspari, Gillum, Gmel, Gonzalez-Medina, Gosselin, Grainger, Grant, Groeger, Guillemin, Gunnell, Gupta, Haagsma, Hagan, Halasa, Hall, Haring, Haro, Harrison, Havmoeller, Hay, Higashi, Hill, Hoen, Hoffman, Hotez, Hoy, Huang, Ibeanusi, Jacobsen, James, Jarvis, Jasrasaria, Jayaraman, Johns, Jonas, Karthikeyan, Kassebaum, Kawakami, Keren, Khoo, King, Knowlton, Kobusingye, Koranteng, Krishnamurthi, Laden, Lalloo, Laslett, Lathlean, Leasher, Lee, Leigh, Levinson, Lim, Limb, Lin, Lipnick, Lipshultz, Liu, Loane, Ohno, Lyons, Mabweijano, MacIntyre, Malekzadeh, Mallinger, Manivannan, Marcenes, March, Margolis, Marks, Marks, Matsumori, Matzopoulos, Mayosi, McAnulty, McDermott, McGill, McGrath, Medina-Mora, Meltzer, Mensah, Merriman, Meyer, Miglioli, Miller, Miller, Mitchell, Mock, Mocumbi, Moffitt, Mokdad, Monasta, Montico, Moradi-Lakeh, Moran, Morawska, Mori, Murdoch, Mwaniki, Naidoo, Nair, Naldi, Narayan, Nelson, Nelson, Nevitt, Newton, Nolte, Norman, Norman, O'Donnell, O'Hanlon, Olives, Omer, Ortblad, Osborne, Ozgediz, Page, Pahari, Pandian, Rivero, Patten, Pearce, Padilla, Perez-Ruiz, Perico, Pesudovs, Phillips, Phillips, Pierce, Pion, Polanczyk, Polinder, Pope, Popova, Porrini, Pourmalek, Prince, Pullan, Ramaiah, Ranganathan, Razavi, Regan, Rehm, Rein, Remuzzi, Richardson, Rivara, Roberts, Robinson, De Leòn, Ronfani, Room, Rosenfeld, Rushton, Sacco, Saha, Sampson, Sanchez-Riera, Sanman, Schwebel, Scott, Segui-Gomez, Shahraz, Shepard, Shin, Shivakoti, Singh, Singh, Singh, Singleton, Sleet, Sliwa, Smith, Smith, Stapelberg, Steer, Steiner, Stolk, Stovner, Sudfeld, Syed, Tamburlini, Tavakkoli, Taylor, Taylor, Taylor, Thomas, Thomson, Thurston, Tleyjeh, Tonelli, Towbin, Truelsen, Tsilimbaris, Ubeda, Undurraga, van der Werf, van Os, Vavilala, Venketasubramanian, Wang, Wang, Watt, Weatherall, Weinstock, Weintraub, Weisskopf, Weissman, White, Whiteford, Wiebe, Wiersma, Wilkinson, Williams, Williams, Witt, Wolfe, Woolf, Wulf, Yeh, Zaidi, Zheng, Zonies, Lopez, AlMazroa and Memish2012; Bor et al., Reference Bor, Dean, Najman and Hayatbakhsh2014; Collishaw, Reference Collishaw2015). In the UK, demand for counselling services, hospital admissions for self-harm and referrals to specialist Child and Adolescent Mental Health Services (CAMHS) have all increased significantly for this age group in recent years (Hagell et al., Reference Hagell, Coleman and Brooks2015; National Society for Prevention of Cruelty to Children, 2016; Page, Reference Page2016; Yeung et al., Reference Yeung, Weale and Perraudin2016). There is also some evidence from survey data of decreases in well-being and increases in emotional problems among teenage girls (Brooks et al., Reference Brooks, Magnusson, Klemera, Chester, Spencer and Smeeton2015; Fink et al., Reference Fink, Patalay, Sharpe, Holley, Deighton and Wolpert2015) and mental health disorders in young adult women (Pym, Reference Pym2016).
Many factors have been proposed as potentially contributing to increasing mental health problems in this age group. These include social and economic changes leading to a lengthening of dependence on parents and delay in reaching more adult levels of autonomy (Patton et al., Reference Patton, Sawyer, Santelli, Ross, Afifi, Allen, Arora, Azzopardi, Baldwin, Bonell, Kakuma, Kennedy, Mahon, Mcgovern, Mokdad, Patel, Petroni, Reavley, Taiwo, Waldfogel, Wickremarathne, Barroso, Bhutta, Fatusi, Mattoo, Diers, Fang, Ferguson, Ssewamala and Viner2016), effects of social media (Bell et al., Reference Bell, Bishop and Przybylski2015), the penetration of cyberbullying into all parts of young people's lives (Bottino et al., Reference Bottino, Bottino, Regina, Correia and Ribeiro2015; National Children’s Bureau and Association of School and College Leaders, 2016) and a more highly pressurised school culture (Lessof et al., Reference Lessof, Ross, Brind, Bell and Newton2016). More recently, the global financial crisis of 2008 has been linked to an increase in suicide and wider mental health problems among both young and older adults in Greece and other European countries (Divya et al., Reference Divya, Charitini and Ioannidis2016).
The need to understand and meet the mental health needs of CYP is reinforced by growing recognition of the importance of early life for lifetime mental health problems. Three-quarters of life-time mental health problems (excluding dementia) occur by age 24 years (Kessler et al., Reference Kessler, Berglund, Demler, Jin, Merikangas and Walters2005). High levels of unmet need for mental health services among CYP exist in most localities in the UK (McShane and Rouse, Reference Mcshane and Rouse2015). Failure to meet these needs may have economic as well as personal and social costs, as there is good evidence that early access to appropriate health services has a potential to improve outcomes of both mild/moderate and more serious mental health problems (Marshall et al., Reference Marshall, Lewis, Lockwood, Drake, Jones and Croudace2005; Hagell et al., Reference Hagell, Coleman and Brooks2015; Hargreaves et al., Reference Hargreaves, Elliott, Viner, Richmond and Schuster2015; National Institute for Health and Care Excellence (NICE) and NHS England, 2016).
Robust, national-level data on the prevalence and patterns of mental health problems among CYP are needed for planning and improving clinical services, understanding societal influences on mental health and evaluating the impact of different policies for CYP in UK countries. However, no detailed national studies have been done that specifically investigate trends in the mental health of CYP (0–24 years) in the UK since the studies performed in 2004 and 2007 (Green et al., Reference Green, Mcginnity, Meltzer, Fort and Goodman2005; Parry-Langdon, Reference Parry-Langdon2008). To address this gap, we aimed to analyse trends in mental health outcomes among CYP in national health surveys from England, Scotland and Wales over the last two decades. We also included data on total long-standing conditions (physical and mental health) and general health as mental health is a major component of each of these.
Methods
Design
Retrospective, secondary analysis of data from nationally representative, cross-sectional, repeated (mostly annual) surveys in the UK. Data were analysed from 140 830 participants (4–24 years) in 36 national surveys in England, Scotland and Wales, 1995–2014.
Data
All national health surveys conducted since 1995 in England, Scotland, Wales or Northern Ireland were accessed. These are repeated, household-based, surveys that use stratified random sampling of individuals from a sample of postcode sectors each year to collect nationally representative data using consistent methodology (Darlington et al., Reference Darlington, Norman and Ballas2014; Scottish_Government; Welsh_Government). The documentation of each survey was searched for all mental and physical health variables applicable to participants aged 0–24 years. At this stage, Northern Ireland was excluded as only one survey in 2007 contained relevant data, so trend analysis was not possible. Children under the age of 4 years were also excluded as no mental health variables were collected in this age group, with the exception of parent-reported long-standing mental health condition, which was very rare. For all measures, parents responded on behalf of children aged 4–12 years. Participants aged 13–15 years were invited to complete the survey themselves in England and Wales, while in Scotland, either parents or young people could complete the survey in this age group. In all countries, young people aged 16 years or over responded for themselves.
Table 1 presents the mental and physical health variables that were available for analysis by age, year and country. Data on 140 830 participants 4–24 years were analysed from the Health Survey for England (HSE) (18 surveys between 1995 and 2014, N = 92 422, 49.4% male), Scottish Health Survey (SHS) (eight surveys 2003–2014, N = 16 862, 49.0% male) and Welsh Health Survey (WHS) (eight surveys 2007–2014, N = 31 546, 49.9% male). See Appendix Table A for numbers of males and females in each survey. Response and missingness rates have been published previously and are fairly consistent over time and between countries. For example, in the HSE 2014, individual response rates were 63% (0–15 years) and 55% (16+ years); missingness rates were <0.5% for general health, long-standing illness and mental health condition; 2.9% for WEMWBS; and 13.0% for GHQ. Due to these low rates of missingness, missing data were not imputed. All data are publically available and were downloaded through the UK Data Service https://www.ukdataservice.ac.uk/. Data were merged and cleaned for time-series analysis following previously published guidance (Darlington et al., Reference Darlington, Norman and Ballas2014).
Table 1. Available mental health variables and selected physical health variables by country, age and year

Outcomes
General health (physical and mental)
– Self-/parent-reported health: dichotomised as very good/good v. fair/bad/very bad;
– Note that Welsh response options for adults were excellent/very good/good v. fair/poor;
– Presence of any long-standing condition: yes/no (England and Scotland only). In Wales, a similar but differently worded question was asked (presence of any currently treated chronic illness: yes/no).
Mental health
– Presence of any long-standing mental health condition: yes/no (England and Scotland only). Please note that long-standing mental health conditions are a subset of those who reported ‘any long-standing condition’. Depending on the survey and year, participants may have either chosen the category ‘mental health’ from a list of long-standing conditions or given an associated free-text response. Note that the ‘mental health’ category does not include problems related to memory, learning/understanding/concentrating or social/behavioural problems (examples given in the HSE are autism/attention-deficit disorder/Asperger's syndrome). Also note that in Wales, a slightly different question was asked;
- Presence of any currently treated mental health problem: yes/no;
- Strengths and Difficulties Questionnaire Total difficulties (SDQT) score (Goodman et al., Reference Goodman, Ford, Simmons, Gatward and Meltzer2000).
Both the total score and a dichotomised score of 0–16 v. 17–40 were analysed.
– Strengths and Difficulties Questionnaire Emotional difficulties (SDQE) score (Goodman et al., Reference Goodman, Ford, Simmons, Gatward and Meltzer2000): the full score and a dichotomised score of 0–4 v. 5–10 were analysed. We investigated the SDQE score separately to the total SDQ as previous studies have raised specific concerns about increasing rates of emotional distress, especially among adolescent girls (Fink et al., Reference Fink, Patalay, Sharpe, Holley, Deighton and Wolpert2015). Detailed analysis of other subscales was beyond the scope of this study. For both SDQT and SDQE, we used thresholds previously published for analysis of parent-reported SDQ scores for children aged 4–17 years (Youth_in_Mind, 2016). Individuals who scored above the described threshold were considered to have screened positive for significant mental health symptoms.
– General Health Questionnaire (GHQ) score (Goldberg et al., Reference Goldberg, Gater, Sartorius, Ustun, Piccinelli, Gureje and Rutter1997): the total score and a dichotomised score (0–3 v. 4–12) were analysed, following previous analysis of GHQ scores in the HSE (Reference KnottKnott).
– Warwick–Edinburgh Mental Wellbeing Scores (WEMWBS) (Clarke et al., Reference Clarke, Friede, Putz, Ashdown, Martin, Blake, Adi, Parkinson, Flynn, Platt and Stewart-Brown2011). No standard threshold has been published, so only the total score was analysed.
The wording of the questions and responses in each questionnaire is presented in Appendix Table B.
Analysis
For consistency between countries, the data were analysed in three age bands: children 4–12 years, early adolescents 13–15 years and young people 16–24 years. We limited ourselves to descriptive analyses of differences between countries and did not formally test these due to differences in survey methodology. Within each country, the proportion of males and females reporting each dichotomous variable was compared.
For each country, unweighted logistic regression models were performed for each dichotomous variable on time (in years). Similarly, unweighted linear regression models were performed for each scale variable on time (in years) for each country. Quadratic time function was included in each model where it was statistically significant (p < 0.05). No other covariates were included. Models were performed for all participants and then repeated for males and females separately. Some datasets included weights based on either sampling probability or a combination of sampling probability and non-response; for England, weighting data for adults were only available from 2002 onwards. Sensitivity analyses were performed comparing the outputs of regression models with weighted and unweighted data.
Additionally, sensitivity analyses were performed to investigate the recent trends from 2011 to 2014.
Due to the large number of comparisons, a p value of <0.01 was considered significant. All analyses were performed using SPSS version 22.
Ethics
No ethics review was needed for these secondary analyses of publically available, anonymised data. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Results
There was a consistent increase in long-standing mental health conditions over time (see Fig. 1). Across all participants aged 4–24 years, the prevalence increased sixfold over the 19-year period in England (from 0.8% to 4.8%, p < 0.001), more than doubled in Scotland over 11 years (2.8–6.5%, p < 0.001) and increased by more than half in Wales over 7 years (2.6–4.1%, p < 0.001). Over the corresponding time periods, the prevalence of total long-standing conditions decreased slightly in England (22.6–19.5%, p < 0.001), increased slightly in Scotland (19.3–22.0%, p < 0.001) and was unchanged in Wales (12.8% v. 13.5%, p = 0.10).
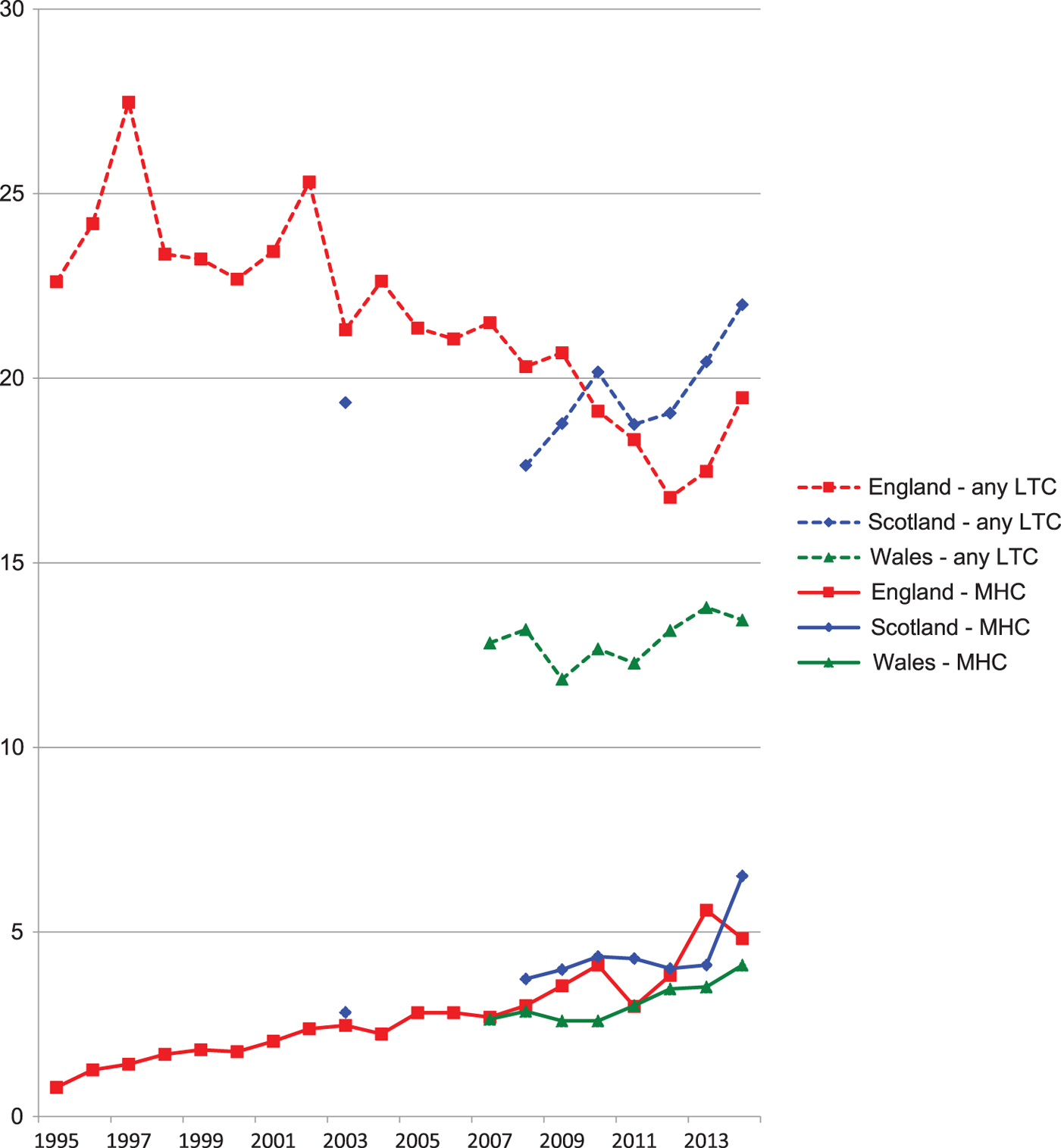
Fig. 1. Self-/parent-reported prevalence of mental health condition and any long-term condition, 4–24 years, UK countries, 1995–2014. Source: Health Survey for England (HSE), Scottish Health Survey (SHS), Welsh Health Survey (WHS). LTC, long-term condition; MHC, mental health condition. Note that wording differs between questionnaires – see Methods section and Appendix for details.
The prevalence of each health problem by country, age and sex is summarised below and presented in Appendix Table C. Findings from the regression models for each country are presented in Tables 2–4. All tables show unweighted data. Repeating the analyses with weighting (where available) had minimal impact on these findings (see Appendix Table D).
Table 2. Odds ratios for changes in mental health and well-being measures over time, by age group and sex. Scottish Health Survey, 2003–2014

SDQT, Strengths and Difficulties Questionnaire Total Score (binary score 0–16 v. 17–36); SDQE, Strengths and Difficulties Questionnaire Emotion Score (binary score 0–4 v. 5–10); GHQ, General Health Questionnaire (binary score 0–3 v. 4–12); WEMWBS, Warwick–Edinburgh Mental Health and Wellbeing Score.
For all binary variables, odds ratios show the change in odds per year over the study period. Values >1 indicate increasing odds of poor health over time. For scale variables (SDQE, SDQT, WEMWBS), the β coefficient represents the change in score per year over time. Positive values indicate increasing number of symptoms (SDQT, SDQE) or increasing well-being score (WEMWBS).
Table 3. Odds ratios for changes in mental health and well-being measures over time, by age group and sex. Welsh Health Survey, 2007–2014

SDQT, Strengths and Difficulties Questionnaire Total Score (binary score 0–16 v. 17–36); SDQE, Strengths and Difficulties Questionnaire Emotion Score (binary score 0–4 v. 5–10.
For all binary variables, odds ratios show the change in odds per year over the study period. Values >1 indicate increasing odds of poor health over time. For scale variables (SDQE, SDQT), the β coefficient represents the change in score per year over time. Positive values indicate increasing number of symptoms.
Table 4. Odds ratios for changes in mental health and well-being measures over time, by age group and sex. Health Survey for England, 1995–2014

SDQT, Strengths and Difficulties Questionnaire Total Score (binary score 0–16 v. 17–36); SDQE, Strengths and Difficulties Questionnaire Emotion Score (binary score 0–4 v. 5–10); GHQ, General Health Questionnaire (binary score 0–3 v. 4–12); WEMWBS, Warwick–Edinburgh Mental Health and Wellbeing Score.
For all binary variables, odds ratios show the change in odds per year over the study period. Values >1 indicate increasing odds of poor health over time. For scale variables (SDQE, SDQT, WEMWBS), the β coefficient represents the change in score per year over time. Positive values indicate increasing number of symptoms (SDQT, SDQE) or increasing well-being score (WEMWBS).
Scotland
Table 2 reported the long-standing mental health conditions increased between 2003 and 2014. This increase was seen in all age groups [4–12 years, 2.6% v. 4.8%, odds ratio (OR) 1.05, p = 0.004; 13–15 years, 3.0% v. 7.8%, OR 1.07, p = 0.02; 16–24 years, 3.1% v. 9.7%, OR 1.08, p < 0.001). This can be interpreted as a 5, 7 and 8% increase per year in the odds of having a long-standing mental health condition in each age group, respectively.
The prevalence of any long-standing condition increased in 16–24 years old (18.1% v. 25.6%, OR 1.04, p = 0.001). There was no change in general health, GHQ or well-being scores over time in any group. The only trend towards improved health was a significant reduction in high SDQT and SDQE scores among girls aged 4–12 years (SDQT: 7.2% v. 4.8%, OR 0.95, p = 0.009; SDQE: 9.6% v. 6.1%, OR 0.96, p = 0.005). No quadratic terms were significant.
In contrast to stable longer term trends, GHQ score increased (worsened) significantly for 16–24 year olds between 2011 and 2014 (OR 0.15, p = 0.003). Conversely, there was no change between 2011 and 2014 in the reported prevalence of any long-standing condition in any age group and self-reported general health improved significantly in 16–24 years old over this period (OR 1.18, p = 0.007). For all other variables, including long-standing mental health conditions, trends from 2011 to 2014 were broadly similar to the longer term trends (see Appendix Table E).
Wales
There was no change in any measure among the 4–12 years group. There was a significant increase in high SDQE scores among 13–15 years old (14.4% v. 24.2%, OR 1.07, p = <0.001) and in young adults reporting treatment for mental health conditions (4.1% v. 7.6%, OR 1.11, p < 0.001). In contrast, there was no change over time in general health or prevalence of any long-standing condition. There were no significant quadratic terms.
Data from 2011 to 2014 on 16–24 years old showed ongoing increased prevalence of mental health disorders (OR 1.14, p = 0.005) and also showed an increased prevalence of any chronic illness (OR 1.08, p = 0.007). Recent trends for all other variables were similar to longer term trends, showing a significant increase in SDQE and SDQT for 13–15 years old, and no change in other variables (see Appendix Table E).
England
There was a consistent increase in the reported prevalence of long-standing mental health conditions across all age and sex groups (range 5.5–9.1% year-on-year increase between 1995 and 2014) (4–12 years: 0.9% v. 3.9%, OR 1.070, p < 0.001; 13–15 years: 1.1% v. 5.4%, OR 1.08, p < 0.001; 16–24 years: 0.6% v. 5.9%, OR 1.09, p < 0.001). Conversely, there was a consistent reduction in the prevalence of any long-standing condition over the same period (4–12 years: 21.5% v. 18.2%, OR 0.98, p < 0.001; 13–15 years: 23.8% v. 18.8%, OR 0.97, p < 0.001; 16–24 years: 23.6% v. 21.7%, OR 0.98, p < 0.001).
The ORs of fair/bad general health decreased among younger participants (4–12 years: OR 0.97, p < 0.001; 13–15 years: OR 0.97, p < 0.001) but not among young adults (OR 0.99, p = 0.07). High SDQT and SDQE scores among young children became less common over time (SDQT: OR 0.98, p < 0.001; SDQE: OR 0.97, p < 0.001) as did high SDQE scores for 13–15 years old (OR 0.98, p = 0.006). There was no change in high SDQT or GHQ scores for 13–15 years old.
The proportion of young adults with high GHQ scores decreased over time (OR 0.99, p = 0.005); within the data available (2010–2014), no change was observed in well-being scores in this age group. Quadratic terms were significant for well-being and GHQ among 16–24 years old, suggesting that well-being and psychological distress may have initially improved between 2010 and 2012 before deteriorating from 2012 to 2014 (WEMWBS linear coefficient = 12.0, p < 0.001, quadratic coefficient = −0.336, p < 0.001; GHQ linear coefficient = 0.81, p < 0.001, quadratic coefficient = 1.01, p < 0.001). No other quadratic terms were significant.
Consistent with these quadratic findings, data from 2011 to 2014 showed a highly significant decrease in WEMWBS scores for 16–24 years old (β coefficient = −0.46, p = 0.001). However, there was no significant change in GHQ scores over this period. Recent trends for other variables largely reflected longer term trends, although the prevalence of any long-standing condition was stable rather than decreasing (please see Appendix Table E). Please note that SDQ data were not collected in the HSE after 2011.
Gender analyses
Analysis of all children aged 4–12 years across the total study period showed that long-standing mental health conditions were more common among boys than girls: England 3.5% v. 1.1% (p < 0.001), Scotland 5.3% v. 1.6% (p < 0.001), Wales 1.5% v. 0.8% (p < 0.001). High SDQT scores were also more common among boys than girls: England 10.6% v. 6.9% (p < 0.001), Scotland 9.8% v. 5.4% (p < 0.001), Wales 10.3% v. 6.1% (p < 0.001).
Gender differences for the 13–15 age group were less consistent. Boys were more likely than girls to report long-standing mental health conditions (England 3.4% v. 1.7%, p < 0.001; Scotland 5.1% v. 2.6%, p < 0.001), any long-standing condition (England 24.8% v. 21.4%, p = <0.001; Scotland 21.2% v. 18.3%, p = 0.05) and high SDQT (England 9.1% v. 7.3%, p = 0.002). Conversely, girls were more likely than boys to report high SDQE (England 12.9% v. 7.7%, p < 0.001), high GHQ (England 13.9% v. 7.3%, p < 0.001; Scotland 11.9% v. 7.0%, p < 0.001) and lower well-being (Scotland 50.0% v. 52.1%, p < 0.001). Sex differences were smaller in Wales in this age group, with the exception of high SDQE scores, which were more common among girls than boys (23.8% v. 11.4%, p < 0.001).
Among young adults, high GHQ scores were more common, and mean WEMWBS scores were lower, among women than men: [GHQ: England 19.2% v. 10.9% (p < 0.001), Scotland 19.2% v. 11.9% (p < 0.001); WEMWBS: England 50.7% v. 52.0 (p < 0.001), Scotland 49.1% v. 50.5 (p < 0.001)]. Long-standing mental health conditions were more common among women than men in Wales [6.6% v. 3.6% (p < 0.001)] but not in England [2.7% v. 2.5% (p = 0.2)], or Scotland [6.2% v. 4.6% (p = 0.02)].
Discussion
To our knowledge, this is the first national-level study to investigate the UK time trends in mental health problems in CYP since 2007. We found a consistent and striking increase in the reported prevalence of a long-standing mental health condition in all three countries. Among CYP aged 4–24 years, the reported prevalence of long-standing mental health conditions increased sixfold between 1995 and 2014 in England and more than doubled between 2003 and 2014 in Scotland. In Wales, where participants were asked to report only conditions for which they were receiving treatment, mental health conditions increased by around half among young adults over the period 2007–2014. Over the same period, reported prevalence of any long-standing condition (of which long-standing mental health conditions are a growing subset) decreased significantly in England. Scales measuring psychological distress showed inconsistent trends, with improvements in SDQT, SDQE and GHQ scores for some age groups in England and Scotland, but deterioration in Welsh SDQE scores for 13–15 years old. Sex differences were as expected from previous studies.
Where direct comparisons were possible, the trends for 2011–2014 were broadly similar to the longer term trends for most variables, although as expected, the recent trends were less statistically significant in many cases. However, there was some evidence of worsening trends in the health of young adults in recent years (increased GHQ scores in Scotland, increased chronic illnesses in Wales and lower well-being scores in England).
There are some limitations to this study arising from the survey content and methodology. The Welsh and Scottish surveys only provide consistent data from 2007 and 2008 onwards, respectively. In comparison, the HSE data provide good coverage over a 19-year period but analysis is limited by some inconsistencies in the content and methodology. For example, GHQ data were not collected in 1996, 2007 and 2013; SDQ data were not collected in 1998, 2000, 2001, 2003, 2009 and/or from 2012 onwards; WEMWBS data were only available from 2010 onwards. While the questions about long-standing illness were included in every survey, the wording and structure has evolved over time. For example, the question changed from ‘Do you have any long-standing illness, disability or infirmity?’ (used until 2011) to ‘Do you have any have any physical or mental health conditions or illnesses lasting or expected to last 12 months or more?’ (used from 2012 onwards).
However, there was no evidence from the quadratic analyses, the separate analyses of recent trends or from Fig. 1 that this wording change had any significant impact on the trend to increased mental health disorders.
Another significant limitation to interpreting these findings is the lack of data on the impact or nature of a mental health condition. Validated items on impact are available as an additional part of the SDQ and could usefully be included in future surveys. Regarding the nature of mental health conditions, it is not possible to investigate how self-/parents’ understanding of mental health conditions compares to clinical definitions or whether these understandings have changed over time. However, there is little evidence to suggest that increases in developmental or behavioural disorders can explain the greater reported prevalence of long-standing mental health conditions, especially as the increases are more pronounced among young adults. Lastly, weighting was not available for adult participants of the HSE before 2002, and weighting methodology has subsequently changed over time. However, the high level of agreement between unweighted and weighted analyses, where direct comparison is possible, provides some reassurance that lack of weighting information and/or changing composition of the sample over time are unlikely to affect our findings significantly. Similarly, response rates are reasonably consistent over time.
Our findings are consistent with the previous evidence of increasing rates of mental health diagnoses among CYP in recent decades across many high-income countries. Collishaw (Reference Collishaw2015) identified several possible factors that may have contributed to higher rates of mental health diagnoses, including increased help-seeking by parents and young people, improved screening and clinical recognition in schools and primary care, medicalisation of feelings and behaviours previously considered as normal, as well as a possible genuine increase in pathology (Collishaw, Reference Collishaw2015). Green et al. (Reference Green, Mcginnity, Meltzer, Fort and Goodman2005) reported a discrepancy between rates of diagnosis based on a clinical interview (10%) and self-report of mental health diagnosis (1–3%) (Green et al., Reference Green, Mcginnity, Meltzer, Fort and Goodman2005). It is possible, therefore, that much of the reported increase in mental health conditions may simply reflect narrowing of the gap between problems that exist and problems that are reported – for example, due to increased awareness of mental health problems, and/or reduced stigma in acknowledging and seeking help for problems. Although this study could not investigate the impact of specific programmes, it is possible that initiatives such as Targeted Mental Health in Schools (TAMHS) (National_Child_and-Maternal_Health_Intelligence_Network) and Improving Access to Psychological Therapies for Children and Young People (CYP IAPT) (NHS_England) in England may have contributed to greater awareness of mental health issues among professionals in schools and primary care, as well as among parents and CYP themselves.
Our findings differ from previous studies that reported an increase in emotional distress, and decrease in emotional well-being in adolescents, alongside a widening gender gap between girls and boys. For example, Fink et al. (Reference Fink, Patalay, Sharpe, Holley, Deighton and Wolpert2015) reported an increase in emotional distress in 11–13 years old girls in England between 2009 and 2014, and the Health Related Behaviour in School-Age Children (HBSC) study reported a trend to decreased well-being of 15-year-old girls in England, 2002–2014 (Brooks et al., Reference Brooks, Magnusson, Klemera, Chester, Spencer and Smeeton2015; Fink et al., Reference Fink, Patalay, Sharpe, Holley, Deighton and Wolpert2015) Similarly, analyses of data from the Longitudinal Study of Young People in England (LSYPE) showed that mean GHQ scores were slightly worse in 2014 than in 2005 and that the gap between girls and boys had widened slightly over this period (Lessof et al., Reference Lessof, Ross, Brind, Bell and Newton2016). In contrast, we did not find any increase in mental health problems among early adolescent girls in England or Scotland, and SDQE scores decreased significantly among 13–15 years old girls in England. With the exception of 4–12 years old in Scotland (where girls had lower SDQT than boys and showed a greater decrease over time), we found no significant difference in trends between males and females for any country or age group. However, we note that our analyses are over a longer time period than many comparable studies, especially in England, so their findings are not directly comparable. As noted above, sensitivity analyses of the most recent four surveys (2011–2014) show that trends during this period are broadly consistent with longer term trends, but there was some evidence of worsening trends in the health of young adults.
Clinical, policy and research implications
Although the year-on-year changes are relatively small in many cases, the sustained trends over many years have led to significant changes in population-level prevalence of long-standing mental health conditions among CYP in the UK (as highlighted in Fig. 1), with significant implications for health services. Parental or CYP perceptions of a long-standing mental health condition may have an important impact on clinical consultations and the success of treatment for both mental and physical health problems. Most UK clinicians have responsibility for some patients aged 0–24 years and should be aware of the increasing need to consider mental health diagnoses in this age group. For mental health professionals, the differing trends between reported long-standing mental health conditions and questionnaire scores suggest that the use and interpretation of such scores in assessing patients should continue to evolve. Further investigation is needed, but it is possible that an increasing range of mental health issues is not adequately captured by existing questionnaires.
Although our data do not allow us to attribute causality, or to separate the effect of multiple interacting influences on mental health, our findings are nevertheless relevant to several current policy debates. The growing burden of mental health problems faced by CYP, both in absolute terms, and as a proportion of all long-standing health conditions (mental and physical) reinforces the growing demand for CAMHS services, which is already posing an important challenge for UK health services and policymakers. Even positive initiatives such as CYP IAPT and increased funding for CAMHS are unlikely to address the scale of unmet need for CAMHS services that has been widely reported elsewhere and is reinforced in our data. However, as many of the determinants and potential solutions to mental health problems in CYP lie beyond healthcare (Ford et al., Reference Ford, Hamilton, Meltzer and Goodman2007; Newlove-Delgado et al., Reference Newlove-Delgado, Moore, Ukoumunne, Stein and Ford2015), multi-sectoral initiatives will also be needed to address wider determinants of mental health problems, ranging from poverty and impact of cuts to benefits and youth services, to modern societal pressures of cyberbullying and early sexualisation.
Our findings also highlight some interesting research gaps. First, better data are clearly needed to inform and evaluate the national CAMHS strategy, and so improve short- and long-term outcomes of mental health problems in CYP. Second, the apparent paradox of increasing rates of long-standing mental health conditions but no consistent increase in psychological distress deserves further investigation. One possibility is that there has been a change in the distribution of common symptoms such as sadness and anxiety within society. For example, Lessof et al. reported a trend towards higher mean GHQ scores, despite no change in the proportion of people reporting above-threshold scores (Lessof et al., Reference Lessof, Ross, Brind, Bell and Newton2016). Our data replicate this finding for young women in Scotland and young men in England, with a significant increase in mean GHQ score over time, but no increase in the proportion with above-threshold scores. However, it is not clear whether this reflects a genuine change in the distribution of mental health symptoms, or just that the GHQ total score is a more sensitive measure of change. Interestingly, the reverse pattern is seen in English 13–15 years old for all SDQT scores and female SDQE score (i.e. a significant decrease in mean overall score, but no decrease in the proportion with above-threshold score). It is also possible that the threshold for self-/parent report of a mental health condition has diverged over time from clinical thresholds, which may explain some of the discrepancy we found between trends for self-/parent reports of a long-standing mental health condition and above-threshold questionnaire scores. The detailed national study of mental health problems in CYP that is currently underway may allow more detailed investigation of this issue.
Lastly, trends in socio-economic inequalities were beyond the scope of this study, but deserve more detailed investigation in the future. LSYPE data showed that, while trends towards increased GHQ scores were particularly marked in CYP from single-parent and reconstituted families, other measures of psychological distress now appeared to be more prevalent among CYP living in more affluent households (Lessof et al., Reference Lessof, Ross, Brind, Bell and Newton2016).
Conclusions
There has been a striking increase in the reported prevalence of long-standing mental health conditions among CYP in England, Scotland and Wales in recent years, over a period of progressive improvement in many physical and general health measures. We report an apparent discrepancy between increases in reported prevalence of long-standing mental health disorders and relatively little change in scores on questionnaires relating to psychological distress and emotional well-being. This discrepancy deserves further investigation.
Our findings reinforce the need to consider what constitutes a mental health problem for young people and to continue to prioritise resources to help young people and their families overcome difficulties they are experiencing. While policy initiatives to promote access to CAMHS services and parity of esteem for mental and physical health are clearly needed, they may be ineffective unless they are adequately funded and accompanied by parallel measures to promote mental health and well-being in schools and wider society.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291718001757.
Acknowledgements
We acknowledge the staff and participants of all the national health surveys that are analysed in this study.
Author contributors
JP, DSH and RMV conceived the study. JP and KF performed all analyses, with support from DSH. All authors contributed to drafting and revising the manuscript, and approved the final version. JP and DSH are the guarantors. All authors had full access to all of the data in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Financial support
No specific funding was received for this research. DSH is supported by an Improvement Science Fellowship from The Health Foundation. The Health Foundation had no role in the study design, analysis and interpretation of data, writing the manuscript or the decision to submit for publication.
Conflicts of interest
None.







