Introduction
Pharmacological maintenance treatment is the cornerstone in bipolar disorder management. Unfortunately, relapse rates remain high despite mood stabilizing treatment (Pallaskorpi et al., Reference Pallaskorpi, Suominen, Ketokivi, Mantere, Arvilommi, Valtonen, Leppamaki and Isometsa2015). Psychoeducation programs are adjunctive interventions that complement pharmacological treatment with the aim to further reduce illness burden and recurrence. Programs are believed to achieve this not only by increasing patients' knowledge of their disorder, but also by changing key attitudes and behaviors toward improved medication adherence and a healthier lifestyle. Programs include education about the risk of recurrence having a chronic condition, treatment options, the risks of drugs and alcohol, as well as the importance of sleep, routines, and healthy habits. Programs also include training to identify personal early warning signs of an imminent episode, and training to manage symptoms. There are several psychoeducational programs for bipolar disorder but only a few have been evaluated in randomized controlled trials. Even though the length of psychoeducational programs vary – some programs are completed within 6 weeks (Parikh et al., Reference Parikh, Zaretsky, Beaulieu, Yatham, Young, Patelis-Siotis, Macqueen, Levitt, Arenovich, Cervantes, Velyvis, Kennedy and Streiner2012) other last up to 6 months (Colom et al., Reference Colom, Vieta, Martinez-Aran, Reinares, Goikolea, Benabarre, Torrent, Comes, Corbella, Parramon and Corominas2003a) – they include similar key ingredients.
Psychoeducation has been shown to reduce relapse rate (Bond and Anderson, Reference Bond and Anderson2015), increase adherence to medication (Colom et al., Reference Colom, Vieta, Sánchez-Moreno, Martínez-Arán, Reinares, Goikolea and Scott2005; Eker and Harkin, Reference Eker and Harkin2012), and improve social functioning (Perry et al., Reference Perry, Tarrier, Morriss, McCarthy and Limb1999). Even though psychoeducation is now recommended in several bipolar management guidelines (Yatham et al., Reference Yatham, Kennedy, Schaffer, Parikh, Beaulieu, O'Donovan, MacQueen, McIntyre, Sharma, Ravindran, Young, Young, Alda, Milev, Vieta, Calabrese, Berk, Ha and Kapczinski2009; Goodwin et al., Reference Goodwin, Haddad, Ferrier, Aronson, Barnes, Cipriani, Coghill, Fazel, Geddes, Grunze, Holmes, Howes, Hudson, Hunt, Jones, Macmillan, McAllister-Williams, Miklowitz, Morriss, Munafo, Paton, Saharkian, Saunders, Sinclair, Taylor, Vieta and Young2016), concern has been raised that the purported effect of psychoeducation on relapse prevention (Bond and Anderson, Reference Bond and Anderson2015) is being too reliant on two pivotal studies (Colom et al., Reference Colom, Vieta, Martinez-Aran, Reinares, Goikolea, Benabarre, Torrent, Comes, Corbella, Parramon and Corominas2003a, Reference Colom, Vieta, Reinares, Martinez-Aran, Torrent, Goikolea and Gastob). In fact, a recent study failed to demonstrate an effect on relapse except in a sub-group of patients with few previous episodes (Morriss et al., Reference Morriss, Lobban, Riste, Davies, Holland, Long, Lykomitrou, Peters, Roberts, Robinson and Jones2016).
The gold standard to prove efficacy of an intervention is randomized controlled trials (RCTs). But results from RCTs are not readily generalizable to routine clinical practice. This is because RCTs often employ strict inclusion and exclusion criteria generating study populations that may differ from patients seen in routine clinical practice. Psychoeducation trials have enrolled patients from academic centers (Parikh et al., Reference Parikh, Zaretsky, Beaulieu, Yatham, Young, Patelis-Siotis, Macqueen, Levitt, Arenovich, Cervantes, Velyvis, Kennedy and Streiner2012) and excluded people with comorbidities (Colom et al., Reference Colom, Vieta, Martinez-Aran, Reinares, Goikolea, Benabarre, Torrent, Comes, Corbella, Parramon and Corominas2003a; de Barros Pellegrinelli et al., Reference de Barros Pellegrinelli, de, Silval, Dias, Roso, Bandeira, Colom and Moreno2013). It is therefore important to complement RCTs with observational studies to evaluate the effectiveness of interventions in routine clinical practice. Although some observational and non-randomized studies corroborate the positive results of psychoeducation (Michalak et al., Reference Michalak, Yatham, Wan and Lam2005; Tidemalm et al., Reference Tidemalm, Johnson, Hulterstrom, Omerov and Wistedt2007; Candini et al., Reference Candini, Buizza, Ferrari, Caldera, Ermentini, Ghilardi, Nobili, Pioli, Sabaudo and Sacchetti2013), observational studies are hampered by confounding-by-indication. This is because the indication for the intervention might be correlated with the outcome. For example, attending a psychoeducational program has been shown to be associated with better adherence prior to the intervention (Cakir et al., Reference Cakir, Bensusan, Akca and Yazici2009), which might bias the results in favor of psychoeducation.
The aim of this study was to estimate the effectiveness of psychoeducation for bipolar disorder in a routine clinical setting. To partly circumvent the problem of confounding by indication we used a within-individual design that controls for confounding caused by differences in time-stationary covariates.
Method
Sample
Data were obtained from the Swedish quality assurance register for bipolar disorder (BipoläR) (Karanti et al., Reference Karanti, Bobeck, Osterman, Kardell, Tidemalm, Runeson, Lichtenstein and Landén2015; Karanti et al., Reference Karanti, Kardell, Lundberg and Landén2016). BipoläR was established in Sweden in 2004 with the aim to improve the quality of the care of bipolar patients in Sweden. The register contains individualized data on patients’ bipolar disorder type (I, II, NOS, cyclothymia, or schizoaffective disorder bipolar type), demographics, interventions, and outcomes. Data are collected by staff at the psychiatric clinics (e.g. psychiatrists, psychiatric nurses, or psychologists) and entered into a web-based application. Registering units include both private and public psychiatric outpatient health care units, and BipoläR covers most health care regions in Sweden. The study was approved by the Regional Ethics Committee in Gothenburg.
Patients can be included in the register at any time, at which a baseline registration is completed. Patients are then expected to be followed-up annually. By the time of data extraction for this study in late 2013, the database included baseline data on 12 850 individuals with 31 470 unique visits (baseline registrations + annual follow-ups). The number of individual visits (baseline registration + annual follow-ups) varied between 1 and 10.
Registrations at baseline and annual follow-ups include data on, for example, the number of affective episodes (depressive, manic, hypomanic, or mixed episodes), psychiatric hospital admissions, suicide attempts or self-harm, medication, and a split global assessment of functioning (GAF) scale using a 100 point scale to assess the patients function and symptom burden, where we used the symptom dimension for this study (Pedersen et al., Reference Pedersen, Hagtvet and Karterud2007). The BipoläR register included approximately 20% of the total number of bipolar disorder patients in Sweden (data from the National Patient register) during the study period. The sex distribution in BipoläR is on par with the whole bipolar disorder population. Patients who receive inpatient care but fail to establish follow-up contact with outpatient clinics will, however, not be captured in BipoläR.
Measurements
At baseline (the first time a patient is entered in the register), the question regarding psychoeducation read: Has the patient obtained psychoeducation? At the annual follow-up registrations, the question read: Has the patient received psychoeducation during the last 12 months? As treatment periods, we used all periods after the registration at which it was first documented that the patient had received psychoeducation. A formal definition of psychoeducation was not introduced in BipoläR until 2013: ‘Psychoeducation should be a pre-defined program that comprise education about the disorder, include strategies to cope with the disorder, and give the possibility for exchange of experiences.’ Even though no formal definition was available prior to 2013, a survey of psychoeducation programs reported to BipoläR concluded that Swedish psychoeducation programs on average comprised of six 2-h sessions, and that group setting was most common (Askland and Ahmad Sadik, Reference Askland and Ahmad Sadik2016).
Outcome variables were admissions to psychiatric in-patient care, involuntary sectioning, suicide attempts or self-harm, depressive episodes, and (hypo-) manic or mixed episodes. Data on mood episodes and other outcomes during the 12 months preceding the annual follow-up interviews were obtained retrospectively by treating clinicians with access to medical charts.
Statistical analysis
To eliminate unmeasured time-stationary confounding, we analyzed data using a within-individual method in which the individual serves as his/her own control. This is important because patients are not randomly assigned to receive psychoeducation in clinical routine. For example, patients with more severe bipolar disorder could be more likely to receive psychoeducation, or vice versa. Either way, such bias would introduce confounding by indication, i.e. confounding caused by the fact that patients have been selected for a specific treatment based on a higher or lower propensity for a certain outcome. The within-individual design used in this study was recently employed to evaluate the effectiveness of mood-stabilizing drugs in a naturalistic setting (Joas et al., Reference Joas, Karanti, Song, Goodwin, Lichtenstein and Landén2017), and the risk of treatment-emergent switch to mania following antidepressant or central stimulant treatments (Viktorin et al., Reference Viktorin, Lichtenstein, Thase, Larsson, Lundholm, Magnusson and Landén2014; Viktorin et al., Reference Viktorin, Rydén, Thase, Chang, Lundholm, D'Onofrio, Almqvist, Magnusson, Lichtenstein and Larsson2017).
We divided the data into time periods, each with a baseline measurement indicating whether the person had or had not received psychoeducation, followed by the subsequent measurement indicating the outcome (for instance if the person had suffered from depressive periods during the last 12 months). The sample was selected as follows: first, we excluded follow-ups that occurred earlier than 0.75 years or later than 2.0 years after the preceding registration in order to limit variability in time between visits. Second, we excluded those who had received psychoeducation at baseline, i.e. prior to the first assessment. This means that patients were treatment-naïve with respect to psychoeducation when entering the study. Third, the first three measurements for each person had to include information on psychoeducation. This is because we needed three visits to construct at least two time intervals. The final sample consisted of 2819 individuals. Within this group, 402 persons had psychoeducation at any follow-up and could contribute with information on the effectiveness of psychoeducation. Figure 1 displays a schematic view of the sample selection. Figure 2 shows a schematic view of the analysis plan. Data were analyzed using conditional logistic regression (Allison, Reference Allison2006), stratified on individuals. Although only individuals with a changing status of psychoeducation (N = 402) could provide information directly on the effect of psychoeducation, other individuals (N = 2417) provide information on the effects of confounding variables such as age and GAF. Furthermore, the within-individual models only make use of individual variation, meaning that only individuals that change status on outcome variables provide information. These numbers are given for each outcome in tables throughout.
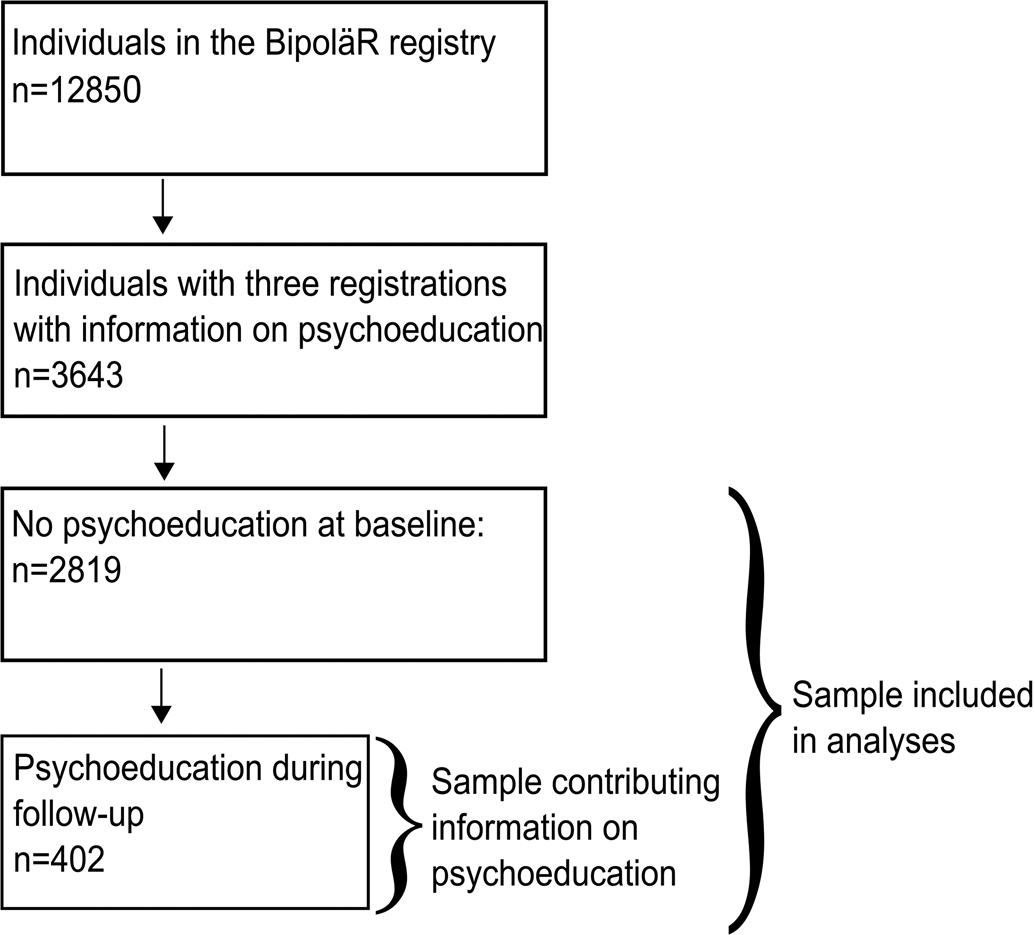
Fig. 1. Sample selection.
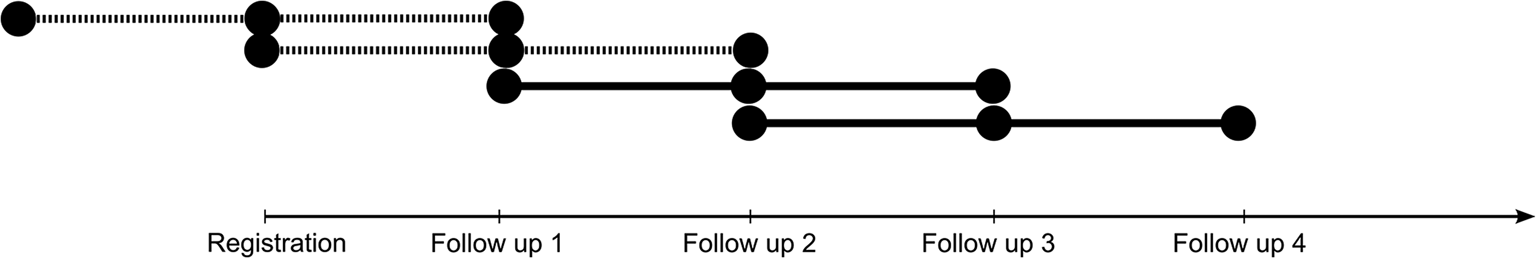
Fig. 2. Schematic view of the study design visualized using one individual's participation. Each line represents a time interval. Note that the number of follow-ups may vary among individuals but includes a minimum of two. The dotted lines indicate non-treatment intervals. Full lines indicate a treatment period, i.e. when the individual had received patient education. The registration or follow-up occurs at the mid-section of each line. Data on completed psychoeducation is collected for the 12 month period preceding the follow-up, whereas the outcome measures are measured at the following visit regarding outcomes 12 months before that visit. Notice the timing of outcome information from one segment might overlap with information on psychoeducation for the following segment. This has been addressed in a sensitivity analysis (Figure S1 in the online data supplement).
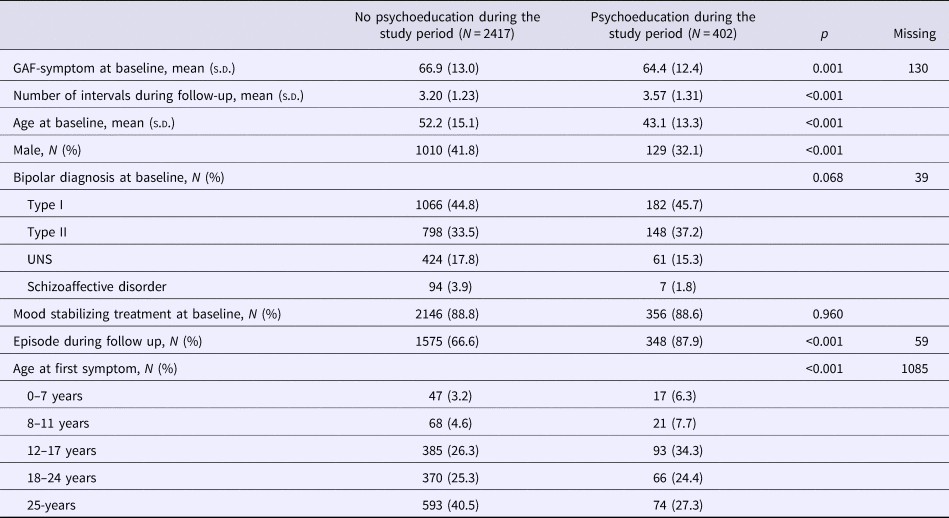
The following outcome variables were analyzed in relation to psychoeducation: any mood episode, (hypo-) manic or mixed episode, depressive episode, inpatient care, involuntary sectioning, and self-harm or suicide attempts. We analyzed the effect of psychoeducation in unadjusted models and models adjusted for the symptom dimension of the Global Assessment of Functioning (GAF) scale, age, and treatment with mood stabilizers (lithium or anticonvulsants). Listwise deletion was employed for intervals with missing values. The results are presented as odds ratios (ORs) with 95% CI, and we used p < 0.05 as the threshold for statistical significance. Pearson's χ2 and t tests were used to test differences in Table 1.
Table 1. Characteristics of the study sample
Although our main mode of analysis was to explore within-individual difference, we also present between-individual models to show differences between the group that received psychoeducation and those that did not. As there were several time intervals per person, we used a logistic GEE model (Halekoh et al., Reference Halekoh, Højsgaard and Yan2006) with an exchangeable correlation structure to account for the correlation between observations on the same individual. These models were adjusted for mood stabilizing medication, GAF-symptom, age, and sex.
Sensitivity- and sub-analyses
Four sensitivity analyses and sub-analyses were conducted to test the robustness of our results. First, it could be possible that the effect of psychoeducation attenuates over time. We therefore conducted a sensitivity analysis by using only the first interval with psychoeducation while excluding subsequent periods. Second, patients' status in the interval just before psychoeducation might be associated with why the person received psychoeducation. We thus conducted a sensitivity analysis where we excluded the segment immediately before psychoeducation. As information on completed psychoeducation was obtained from the same registration as outcomes during the previous segment, there is a possible overlap in the last segment considered to be without psychoeducation. We therefore removed the segment before psychoeducation in a sensitivity analysis to eliminate this possibly ambiguous time interval. Third, the psychoeducation might have occurred early in a time period and influence outcomes at the same registration where psychoeducation was first registered. We therefore computed time intervals where we used measures of psychoeducation and outcomes from the same visits. However, this means that the outcome could have occurred before the event. Therefore, we also included a fourth sensitivity analysis where we excluded such ambiguous observations. Sensitivity analyses #3 and #4 were only computed with the outcome variable ‘relapse in any mood episode’ as the question regarding relapses during the last 12 months at the baseline registration encompassed all relapses. For a schematic view of the sensitivity- and sub-analyses, see Figure S1 in the online Supplementary material.
Results
The characteristics of the study sample are presented in Table 1. Only diagnostic subgroup and mood stabilizing medication at baseline were significantly different between the two groups. For descriptive purposes, we calculated the percentage of individuals with any mood episode during the study periods for the two groups, adjusted for GAF-symptom, mood stabilizing treatment, sex, and age at baseline. Any mood episode occurred in 86.5% of the psychoeducation group and 69.4% in the no psychoeducation group. Notably, these numbers include relapses during the whole study period, including periods before as well as after psychoeducation.
Table 2 shows the results from the main conditional logistic regression analyses. It should be noted that the fully adjusted models have fewer observations than the unadjusted models due to missing data on covariates.
Table 2. Effect of psychoeducation on different outcomes using conditional logistic regression with separate strata for each individual (total number of individuals = 2819; individuals receiving psychoeducation (PE) during follow-up = 402; time intervals = 9161)
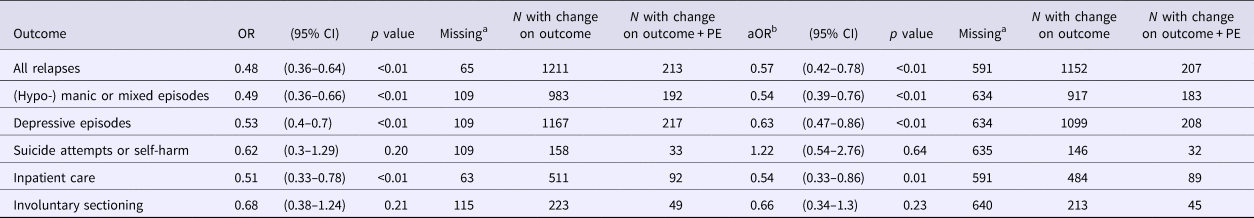
a The number of time intervals with missing data.
b Adjusted for age, mood stabilizing treatment, and GAF-symptom.
Psychoeducation was significantly associated with a decreased rate of any mood episode, (hypo-) manic episodes, mixed episodes, depressive episodes, and inpatient care in the unadjusted as well as in the adjusted analyses. Importantly, only individuals with a changing status on psychoeducation (N = 402) contributed information directly on the effect of psychoeducation, other individuals (N = 2417) provide information on the effects of confounders such as age and GAF.
The first sensitivity analysis (Table S1 in online data supplement), which only used the first time segment after receiving psychoeducation, showed similar results. The results were also similar in the unadjusted second sensitivity analysis (online Supplementary Table S2), which applied a washout period prior to the first instance of psychoeducation, although the estimates were attenuated in the adjusted analysis and not statistically significant except for inpatient care. Sensitivity analyses #3 and #4 (online Supplementary Table S3) showed similar results as the main analysis for all relapses.
For descriptive purposes, we also calculated between-group differences (online Supplemental Table S4) using a GEE model (Halekoh et al., Reference Halekoh, Højsgaard and Yan2006). In these between-group estimates, neither relapse rate nor inpatient care differ between the psychoeducation and no-psychoeducation groups.
Discussion
We used a within-individual design to study the effectiveness of psychoeducation in bipolar disorders in routine clinical practice. Our sample consisted of 2819 subjects of whom 402 individuals received psychoeducation during the follow-up. The results suggest that psychoeducation reduces the risk of mood episodes and hospital admission in routine clinical practice, but we found no evidence for reduced rates of involuntary sectioning, or suicide attempts and self-harm. The sensitivity analyses were chiefly consistent with the main analyses. This observational study is an important complement to previous RCTs suggesting that psychoeducation is effective also when implemented on a large scale in routine clinical practice.
Our findings are in line with a recent meta-analysis on RCTs of psychoeducation that showed a protective effect on any relapse as well as on manic relapse (Bond and Anderson, Reference Bond and Anderson2015). The effect on depressive relapse was only evident when considering programs that delivered the treatment in a group setting. By contrast, however, the latest large scale RCT of psychoeducation did not show an effect of psychoeducation except for those with a low number of previous episodes (Morriss et al., Reference Morriss, Lobban, Riste, Davies, Holland, Long, Lykomitrou, Peters, Roberts, Robinson and Jones2016). Notably, this randomized effectiveness study used an active control, which for obvious reason cannot be used outside a trial setting. Hence, our study gives no information on the active components of psychoeducation.
In most prior RCT studies of psychoeducation, individuals with bipolar II disorder were underrepresented, which means that results apply principally to bipolar I disorder. The current study includes almost equal numbers of subjects with bipolar disorder type I and II (45.6% v. 37.3%), and thus adds to the literature on the effect of psychoeducation in bipolar II disorder. Our results suggest that psychoeducation is effective in both bipolar type I and II disorder, which is in line with Colom et al.'s post-hoc analysis in a subgroup of patients with bipolar type II (Colom et al., Reference Colom, Vieta, Sanchez-Moreno, Goikolea, Popova, Bonnin and Scott2009).
Previous RCTs had well-defined programs of psychoeducation. By contrast, the quality register BipoläR did not provide a definition of psychoeducation during the study period, which means that this study does not include information on the length or setting of the definition of the psychoeducational program. However, a recent survey of psychoeducational programs for bipolar disorder in Sweden found that psychoeducational programs on average consisted of six 2-h sessions, and that group setting was most common (Askland and Ahmad Sadik, Reference Askland and Ahmad Sadik2016). Even though this is briefer than for example the Barcelona program (Colom et al., Reference Colom, Vieta, Martinez-Aran, Reinares, Goikolea, Benabarre, Torrent, Comes, Corbella, Parramon and Corominas2003a), a study found that a short program showed comparable effectiveness to 20 sessions of CBT (Parikh et al., Reference Parikh, Zaretsky, Beaulieu, Yatham, Young, Patelis-Siotis, Macqueen, Levitt, Arenovich, Cervantes, Velyvis, Kennedy and Streiner2012). Another study demonstrated improved adherence in a 6-week psychoeducation program (Eker and Harkin, Reference Eker and Harkin2012). Taken together, these results suggest that briefer psychoeducation curriculums are also effective and might provide an even more cost-effective alternative to more comprehensive programs, which have previously been shown to be cost-effective (Scott et al., Reference Scott, Colom, Popova, Benabarre, Cruz, Valenti, Goikolea, Sanchez-Moreno, Asenjo and Vieta2009). This is important because more extensive programs, e.g. the Barcelona model, not only requires staff training but are also time consuming, which raises barriers to psychoeducation access. Further, smaller general psychiatric outpatient units might not have a sufficient patient base to make the effort worthwhile. Developing a web-based education is one option that would remove some barriers to access.
In previous clinical trials, psychoeducation has been delivered by educators with varying clinical experience and professional backgrounds: experienced psychologist (Colom et al., Reference Colom, Vieta, Martinez-Aran, Reinares, Goikolea, Benabarre, Torrent, Comes, Corbella, Parramon and Corominas2003a), psychologist with little clinical experience (Perry et al., Reference Perry, Tarrier, Morriss, McCarthy and Limb1999), or experienced psychiatric staff including both psychologists, nurses, and psychiatrist (Parikh et al., Reference Parikh, Zaretsky, Beaulieu, Yatham, Young, Patelis-Siotis, Macqueen, Levitt, Arenovich, Cervantes, Velyvis, Kennedy and Streiner2012). In our study, psychoeducation was probably most commonly delivered by nurses, followed by psychiatrists and psychologists (Askland and Ahmad Sadik, Reference Askland and Ahmad Sadik2016).
We did not find an effect of psychoeducation on involuntary sectioning and suicide and self-harm. This could be due to the low number of events and limited power, but it could also be that these severe outcomes are not prevented by psychoeducation. Indeed, although suicidality and self-harm and involuntary treatment are addressed in some longer psychoeducational programs, these topics are not always included in shorter programs given by local clinics in Sweden. We also analyzed our data with between-individual models that did not show any association between psychoeducation and the selected outcomes. However, between-individual models are susceptible to confounding-by-indication, whereas the within-individual model control for time-stationary confounders.
Strengths and limitations
The major strength of this study is the large sample of persons with bipolar disorder treated in a natural setting. The results are therefore generalizable to bipolar disorder patients in routine clinical practice. The study should, however, be interpreted with several limitations in mind. (i) The study is observational and not randomized, which precludes causal conclusions on the effect of psychoeducation. Females and younger patients were overrepresented in psychoeducation programs. The survey of psychoeducational programs in Sweden reported that almost half of responding clinics actively prioritized patients for psychoeducation, the basis of which varied between clinics, but included newly diagnosed patients, young patients, and patients with frequent relapses (Askland and Ahmad Sadik, Reference Askland and Ahmad Sadik2016) reflecting clinical decisions backed by recent evidence (Morriss et al., Reference Morriss, Lobban, Riste, Davies, Holland, Long, Lykomitrou, Peters, Roberts, Robinson and Jones2016). Conversely, clinics reported that they also had criteria for patients less fit for psychoeducation, such as ongoing substance abuse, not being euthymic, lack of insight, personality disorder, numerous previous episodes, and low cognitive ability (Askland and Ahmad Sadik, Reference Askland and Ahmad Sadik2016). To circumvent this potential confounding by indication, we used a within-individual design. This method controls for confounding caused by differences in time-stationary covariates, such as sex, genetic makeup, premorbid history, and lifetime severity of the disorder. We also adjusted for GAF, age, and mood-stabilizing drug use as time-varying confounders. Nevertheless, unmeasured time-varying confounders may still have influenced the outcome. (ii) Given that we rely on annual reports, the timing of intervention and measures of outcomes might in some cases overlap. We therefore conducted a sensitivity analysis where we removed the segment immediately before psychoeducation. In this analysis, decreased risk of inpatient care after psychoeducation was the only significant finding. This analysis comprised fewer observations due to the exclusion of many time-intervals. Hence, lower statistical power probably plays a large part. But the point estimates were also somewhat attenuated when compared to the primary analysis and it cannot be excluded that decreased time-varying confounding might play a role: If severity of illness would be associated with receiving psychoeducation, removing the segment immediately prior to psychoeducation would decrease differences in outcome before and after psychoeducation. There is also the possibility that psychoeducation took place before the outcome due to overlap, but such bias would rather lead to null results in the primary analysis. (iii) Finally, the lack of a formal definition of psychoeducation in the BipoläR questionnaire is a limitation as it reduces the specificity of the exposure variable.
Conclusion
Using a within-individual design that controls for a time-stationary confounding, we show that psychoeducation for bipolar patients in a routine clinical setting decreases the risk of mood new episodes and inpatient care. Although not all sensitivity analyses were entirely concurrent with the main results, the results taken together suggest that findings from previous efficacy clinical trials translate to effectiveness in routine clinical practice.
Author ORCIDs
Erik Joas, 0000-0001-9546-2192
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291719001053
Financial support
This study was supported in part by grants from the Swedish Medical Research Council (K2014-62X-14647-12-51 and K2010-61P-21568-01-4), the Swedish Foundation for Strategic Research (KF10-0039), the Swedish Federal Government under the LUA/ALF agreement (ALFGBG-142041), and the Sigurd and Elsa Golje foundation (LA2015-0173). Erik Joas' is partly funded by the University of Gothenburg (U2014/185). The funding agencies had no role in the design of the research, the data collection and analysis, the interpretation of the data, the writing of the report, or the decision to submit the manuscript.
Conflict of interest
Francesc Colom is the co-author of ‘Psychoeducation Manual for Bipolar Disorder’ (Cambridge University Press, 2006). No other authors report conflicts of interest.






