There is increasing recognition that the impact of military service, separation including deployment and post-traumatic stress disorder (PTSD) extends beyond the individual and can also affect the mental health and well-being of partners and children.Reference Diehle, Brooks and Greenberg1–Reference Beckham, Braxton, Kudler, Feldman, Lytle and Palmer10 However, several mediating factors have been identified, such as family demographics, with parental psychopathology the most consistently identified risk factor.Reference White, de Burgh, Fear and Iversen3, Reference Acion, Ramirez, Jorge and Arndt5, Reference Barker and Berry8 Interest in the possible impact of service personnel's PTSD on their children arose from the post-Vietnam research but most of the empirical studies looked at the impact on adult-aged children, rather than during childhood itself.Reference Jordan, Marmar and Fairbank9, Reference Beckham, Braxton, Kudler, Feldman, Lytle and Palmer10 Little is known about the social and emotional well-being of children whose fathers have PTSD but the impact has been shown to vary by the age and gender of the child. This study examines: (a) the emotional and behavioural well-being of children whose fathers are or were in the UK armed forces during the recent conflicts in Iraq and Afghanistan (between 2003 and 2009), (b) the effect of paternal deployment to Iraq or Afghanistan on children from military families, (c) the effect of paternal PTSD on children from military families, and (d) the specific impact of paternal avoidance and numbing symptoms on childhood emotional and behavioural well-being because these symptoms are particularly pervasive and socially impairing.
Method
Participants
This study recruited participants who were already part of a large (n = 9990) two-phase tri-service cohort (the King's Centre for Military Health Research (KCMHR) cohort study).Reference Hotopf, Hull and Fear11, Reference Fear, Jones and Murphy12 This cohort study initially included a representative random sample of UK service personnel who deployed to the 2003 Iraq conflict, and a non-deployed comparison group; a second phase was conducted that included those who had deployed to Afghanistan, as well as a ‘replenishment’ sample. The replenishment sample, was added to include those who had joined the military since the cohort was first recruited in 2003, and thus would have had the opportunity to deploy to either military operation during the study period. The underlying cohort study comprised regulars (full-time members of the UK armed forces) and reserves (voluntary and part-time members of the UK armed forces who would usually have alternative employment) from all service branches (navy, marines, army and air force).
For the current study, a sample of fathers was drawn from those who completed the second phase of the KCMHR cohort study and gave consent for follow-up. Two groups of fathers were selected. Group 1 consisted of male participants with one or more children aged 3–16 years, who scored ≥40 on the Post Traumatic Disorder Checklist (PCL),Reference Blanchard, Jones-Alexander, Buckley and Forneris13 or who qualified as a ‘case’ on at least two domains of the PCL. Group 2 comprised male participants with one or more children aged 3–16 years who scored <40 on the PCL.
Overall, 1030 military fathers from phase 2 of the KCMHR cohort study, who met the eligibility criteria of the current study were invited to participate. These 1030 fathers were representative of all services, engagement types and included service personnel who had subsequently left the military. If the fathers gave consent, we contacted the mother(s) of their children and invited them to participate in an online survey. The study did not differentiate between biological, looked after and step-children. The study received ethical approval from the UK Ministry of Defence Research Ethics Committee (MODREC), the King's College Hospital local research ethics committee and the US Human Protection Research Office.
Study protocol and procedures
Data collection began in July 2010 and ended in October 2012. Invitation packs consisted of an invite letter informing the father about the study, an information sheet, consent form and response sheet. Data were collected from fathers using standardised self-report online questionnaires and clinical telephone interviews. Instructions given prior to the online questionnaire stipulated that participation in the study was voluntary, participants were free to withdraw at any time and the study was funded by the US Department of Defense.
The online questionnaire was divided into seven sections: (a) consent; (b) service information (including information on most recent deployment, engagement type, and reasons for leaving the armed forces (if they have left)); (c) current employment; (d) mental health; (e) relationship adjustment; (f) details on each of their children (such as name, age, name of mother); (g) questions on the health and well-being of each of their children.
Once fathers had completed the online survey, they were contacted by the research team and booked in for a telephone interview (conducted by trained research assistants). CAPSReference Blake, Weathers and Nagy14 and SAD-QReference Stockwell, Hodgson, Edwards, Taylor and Rankin15 were used, but SAD-Q data are not presented here.
If fathers gave consent, mothers(s) of their children were invited to take part in the study. They were sent an invitation pack containing a letter informing them about the study, an information sheet, a consent form and a response sheet. Mothers were requested to fill in an online questionnaire, which was divided into four sections: (a) consent; (b) current employment; (c) mental health; (d) the health and well-being of each of their children. All participants were sent a cheque for £30 as a thank you for their time and a signposting sheet with a list of agencies that offer services and support for military personnel and their families.
PTSD symptoms were assessed using the 17-item PCL-C;Reference Blanchard, Jones-Alexander, Buckley and Forneris13 a cut-off score of ≥50 was used to determine individuals with probable PTSD, a cut-off of ≥40 was used for subthreshold PTSD.Reference Blanchard, Jones-Alexander, Buckley and Forneris13, Reference Mylle and Maes16 During the interview, all fathers (whether part of the PTSD group or not) were administered the Clinician-Administered PTSD Scale (CAPS-IV).Reference Blake, Weathers and Nagy14, 17 Each symptom is rated on intensity and frequency using a five-point scale ranging from 0 to 4 (never to daily or almost every day). Standard diagnostic scoring uses a F1/I2 rule whereby a symptom is counted as ‘present’ if the frequency scores 1 or higher (i.e. it is present at least once in the past month), and the intensity scores 2 or higher (i.e. experiencing moderate distress or impairment). The frequency and intensity scores can be added to calculate a continuous score of PTSD severity ranging from 0 to 136. To meet diagnosis for PTSD on the CAPS, participants had to have at least one B (re-experiencing) symptom, three C (avoidance and numbing) symptoms and two D (hyperarousal) symptoms. Subthreshold PTSD was established using the definition employed by Cukor et al Reference Cukor, Wyka, Jayasinghe and Difede18 that requires that cluster B and either cluster C or cluster D criteria are met for at least 1 month and functional impairment is reported. Fulfilling the CAPS criteria (full or subthreshold) was the definition used in the subsequent analysis.
Primary outcome measure
Screening for emotional and behavioural difficulties in children was assessed using the 25-item Strengths and Difficulties Questionnaire (SDQ).Reference Goodman19 Total scores were calculated for five subscales: emotional symptoms (i.e. worries a lot, often unhappy), conduct problems (i.e. temper tantrums, fights with other children), hyperactivity (i.e. restless, easily distracted), peer problems (i.e. solitary, picked on/bullied) and prosocial difficulties (i.e. inconsiderate, unkind to others). ‘Caseness’ for ‘total difficulties’ is determined by combining four of the five individual SDQ subscales (excluding prosocial difficulties). Caseness for total difficulties and for each subscale, is categorised as normal, borderline or abnormal using defined and validated cut-offs.Reference Goodman19 Mothers’ and fathers’ scores have been previously shown to be similarReference Davé, Nazareth, Senior and Sherr20 and this was reflected in the SDQ data collected here. Although fathers and mothers did not show perfect concordance when assessing their children, interrater comparisons using Cohen's kappa showed that there were no statistically significant differences on any SDQ question (data available on request from the authors). Consequently, this study used mothers’ SDQ scores where available, substituting the father's score where the mother's was not provided.
Responders
Of the 1030 fathers invited to participate, 86 could not be followed up because of death (n = 3) or insufficient contact details (n = 83). A further 13 individuals were ineligible because their children were outside the 3–16 years age range. The final sample size was 931 eligible fathers. We obtained a response from 688 fathers (73.9%), with 621 (66.7%) fathers completing all aspects of the study (Fig. 1). Of the 621 fathers who responded in full, 511 gave us details to contact the mother(s) of their child or children. Of the 522 mothers contacted as a result, seven were ineligible as their child was outside the 3–16 years age range by the time they were invited to participate, or because the father withdrew his participation from the study. The final sample size of mothers was 515; a response was obtained from 397 (77.1%) of mothers (Fig. 2).
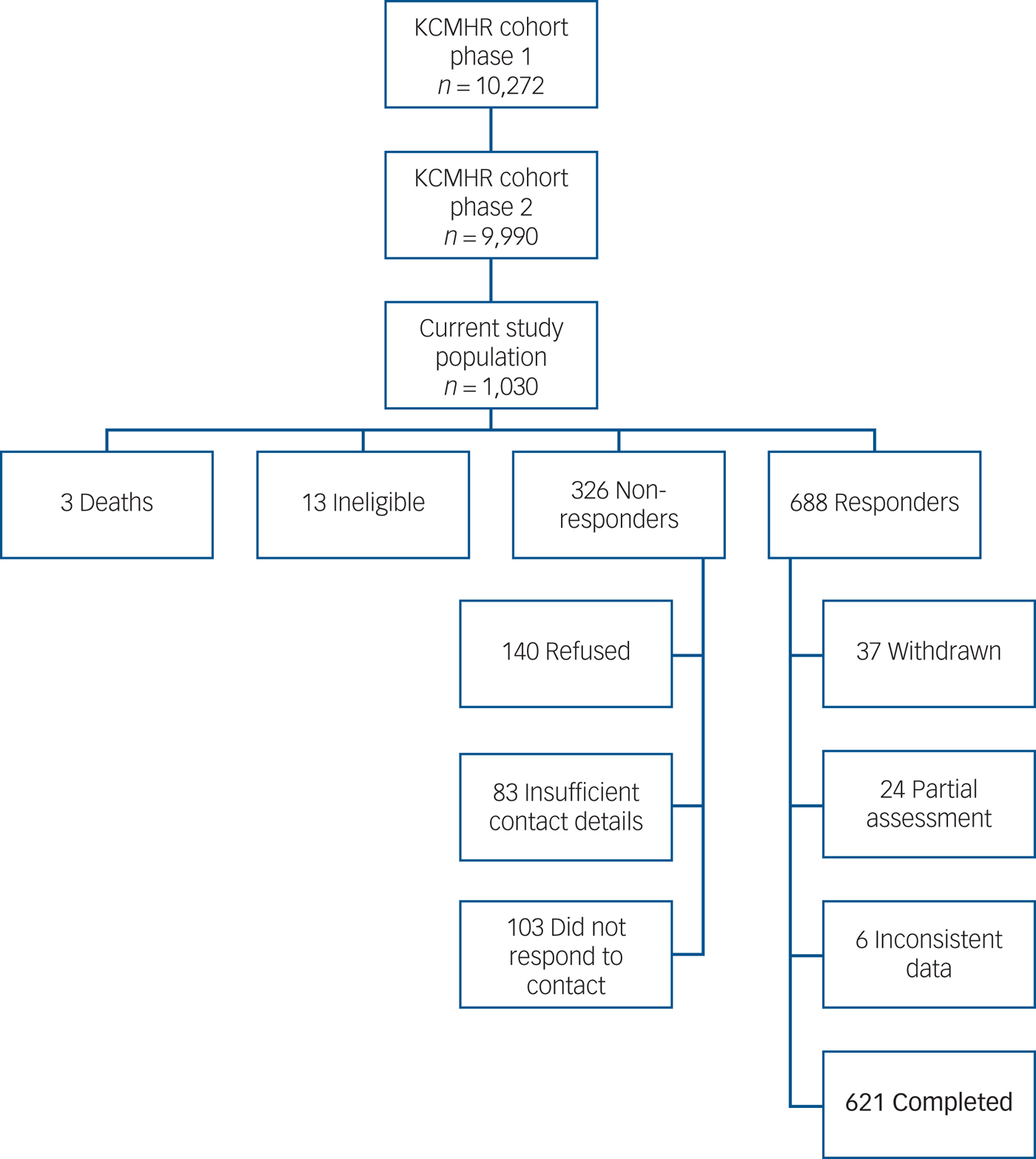
Fig. 1 Summary of sampling and response for fathers.
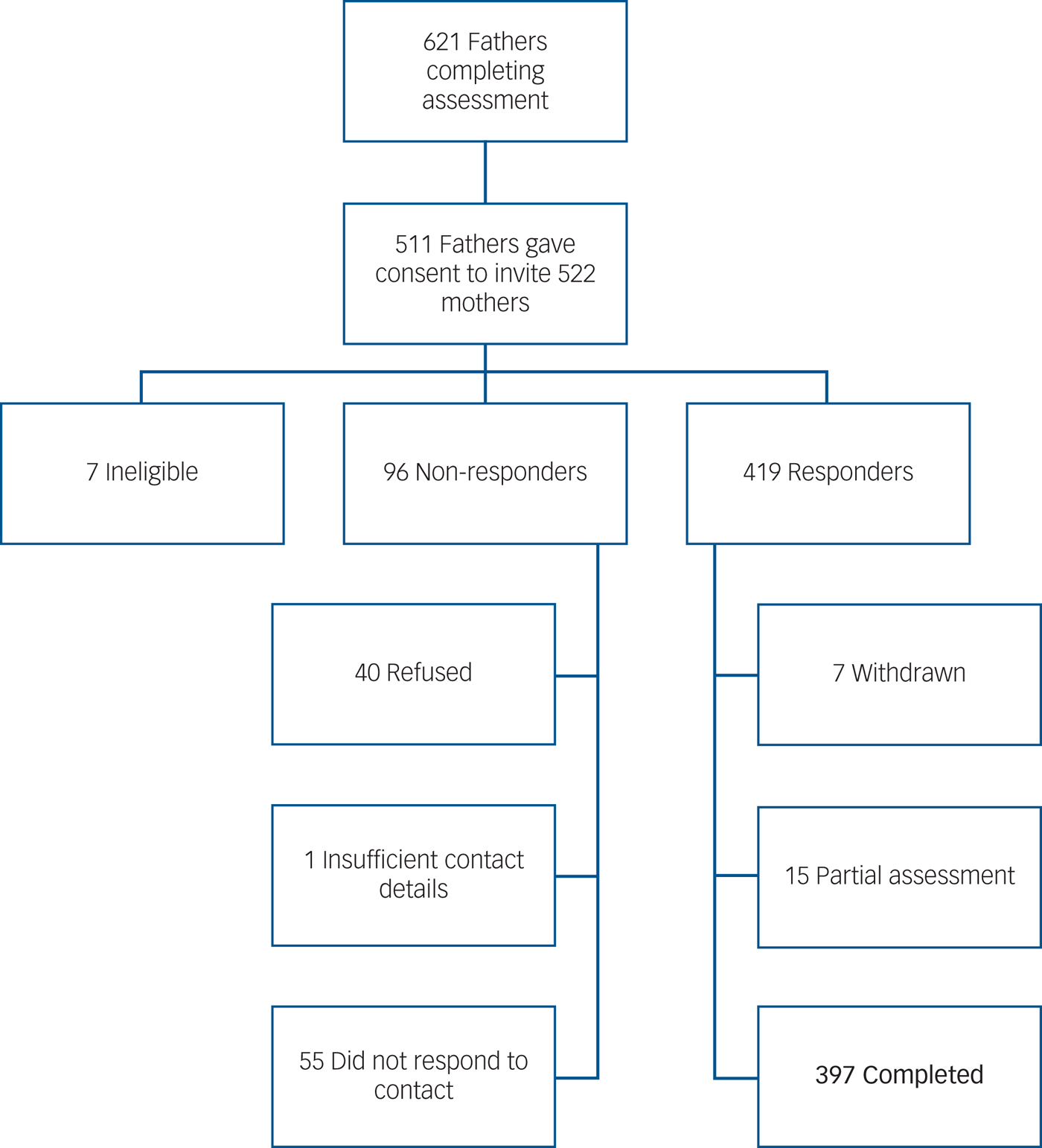
Fig. 2 Summary of sampling and response for mothers.
Responding was associated with age (responders being older), being a reserve, being in the follow-up sample v. operation HERRICK or the replenishment sample (i.e. those with a longer-term commitment to the KCMHR cohort study were more likely to respond), have a PCL score of <50 or a score of <16 on the Alcohol Use Disorders Identification TestReference Babor, Higgins-Biddle, Saunders and Monteiro21 at the time of sampling and being an officer or non-commissioned officer (v. holding a lower rank). Response weights were defined as the inverse probability of responding once sampled and driven by factors shown empirically to predict response (rank, age, sample, engagement type, PCL status and alcohol misuse). Response weights were taken into account in all analyses to adjust for non-response. The weighted analyses provide valid results under the assumption that the data are missing at random and that the observed variables modelled to drive non-response were correctly identified.
Statistical analyses
All analyses were undertaken using the statistical software package Stata (version 11.0), and statistical significance was defined as a P < 0.05. All analyses take account of the response weights by using the survey commands and the clustering by father by using the clustering commands. Weighted percentages and multinomial odds ratios are presented, together with unweighted cell counts. We describe the sociodemographic and military experiences of our sample, before presenting multinomial odds ratios, 95% confidence intervals and P-values, which were calculated to estimate associations between paternal deployment status, paternal PTSD status (as measured by CAPS), paternal reporting of symptoms of avoidance and numbing (as these symptoms are considered to be particularly socially impairing and to interfere with parenting) and childhood SDQ outcomes. SDQ scores used in these analyses were those given by the mother where available, and from the father where a maternal score was not available. Subanalyses were also performed involving stratification by age of the child (<11 years and ≥11 years) and by gender of the child. Univariable and multivariable multinomial and binary logistic regression analyses were undertaken, sociodemographic (child age, paternal age, paternal relationship status, gender of child) and military (rank, service, engagement type (regular or reservist status), deployment status (not deployed to Iraq or Afghanistan or deployed to Iraq or Afghanistan, for the paternal PTSD analyses) factors were included in the multivariable analyses. Our sample size was devised to allow us at least an 85% power to detect a difference in the prevalence of SDQ caseness from 10 to 20% between the paternal PTSD case group and the paternal non-PTSD case group.
Results
Most study participants served in the army (68.3%) and were non-commissioned officers (67.2%) (supplementary Table 1, available at http://dx.doi.org/10.1192/bjp.2017.16). Although all were serving at the time of initial sampling in the underlying cohort study, over a third (36.7%) had left by the time they participated in this study. These 621 fathers have 1044 children, 87.9% have one or two children with 2.5% reporting four or more.
Table 1 describes the emotional and behavioural difficulties (as measured by SDQ) of the 1044 children included in this study. Of the 1044 children, 13.3% were classified as cases for ‘total difficulties’ and a further 9.2% were borderline. The prevalence of difficulties ranged from 6.7% (for prosocial difficulties) to 16.6% for hyperactivity. The distribution by age and gender showed that there were approximately equal numbers of girls and boys (520 v. 524 respectively) but more aged <11 years than those aged ≥11 years (607 v. 437 respectively). Approximately a fifth of boys and those aged <11 years reported hyperactivity, with emotional problems the most prevalent difficulties among girls and those ≥11 years (16.2 and 19.5%, respectively).
Table 1 Characteristics of children of fathers who are or have been in the UK armed forces in the study (n = 1044)a

SDQ, Strengths and Difficulties Questionnaire.
a. Unweighted numbers and weighted percentages are reported.
Impact of paternal deployment to the conflicts in Iraq and Afghanistan
Paternal deployment to the conflicts in Iraq and Afghanistan was not associated with emotional and behavioural difficulties for children of military fathers (as measured by SDQ) (Table 2). Analyses by child age and gender did not reveal any notable associations (data available from the authors on request).
Table 2 Associations between paternal deployment status and childhood social and emotional problems (as measured by the Strengths and Difficulties Questionnaire (SDQ)) for children whose fathers who are or have been in the UK Armed Forcesa

Unweighted numbers and weighted percentages are reported.
a. multinomial odds ratios and 95% confidence interval are reported.
Effect of paternal PTSD
Table 3 reports the association between paternal PTSD status (having subthreshold or full PTSD based on the CAPS) and the SDQ domains. Unadjusted analyses show that paternal PTSD is associated with childhood hyperactivity (odds ratio (OR) 2.01, 95% CI 1.20–3.36), prosocial difficulties (OR = 2.24, 95% CI 1.04–4.81) and total difficulties (OR = 1.93, 95% CI 1.06–3.51). Following adjustment for child and father demographics and father's military factors, only the association with childhood hyperactivity remained statistically significant (OR = 1.86, 95% CI 1.06–3.28).
Table 3 Associations between paternal PTSD and childhood social and emotional problems (as measured by the Strengths and Difficulties Questionnaire (SDQ)) for children whose fathers who are or have been in the UK Armed Forcesa

PTSD, post-traumatic stress disorder.
a. Unweighted numbers, weighted percentages, multinomial odds ratios, adjusted odds ratios and 95% confidence intervals are reported. Adjusted multinomial odds ratios adjusted for child's age, gender, father's age, relationship status, deployment status, engagement type, rank and service.
Supplementary Tables 2 and 3 show the results by age of the child, adjusted for sociodemographic and father's military factors. Among children <11 years of age, father's PTSD was associated with hyperactivity, prosocial difficulties and total difficulties. The association with hyperactivity remained following adjustment. For children aged ≥11 years, paternal PTSD was not associated with any SDQ domain.
The analysis was repeated separately for boys and girls (supplementary Tables 4 and 5). For boys, unadjusted analyses revealed associations between paternal PTSD and childhood hyperactivity, conduct problems, prosocial difficulties and total difficulties. There is also a borderline association between paternal PTSD and childhood peer problems. Following adjustment, associations remained statistically significant for childhood hyperactivity. Unlike boys, there were no associations between paternal PTSD and any emotional and behavioural difficulties for girls.
Effect of paternal avoidance/numbing symptoms
Statistically significant associations were found between paternal symptoms of avoidance and numbing and childhood prosocial difficulties, this was removed following adjustment (Table 4). Additional associations were seen with peer problems for those <11 years of age and boys and conduct problems among boys (data available from the authors on request).
Table 4 Associations between paternal symptoms of numbing and avoidance and childhood social and emotional problems (as measured by the Strengths and Difficulties Questionnaire (SDQ)) for children whose fathers who are or have been in the UK Armed Forcesa

a. Unweighted numbers, weighted percentages, multinomial odds ratios, adjusted multinomial odds ratios and 95% confidence interval are reported. Adjusted multinomial odds ratios adjusted for child's age, gender, father's age, father's relationship status, deployment status, engagement type, rank and service.
Discussion
Main findings
The aim of the study was to examine the emotional and behavioural well-being of children whose fathers were in the UK armed forces during the recent conflicts in Iraq and Afghanistan, particularly the effects of deployment to these conflicts and paternal PTSD. This large representative study of the children of military fathers, using validated measures has shown that the majority of children with fathers in the UK armed forces do not report adverse emotional or behavioural difficulties. Approximately a fifth had an emotional or social difficulty as reported on the SDQ, with the most common difficulty being hyperactivity. None of the childhood outcomes examined were associated with paternal deployment to the conflicts in Iraq or Afghanistan. On the other hand, childhood hyperactivity was associated with paternal PTSD, and this association was most notable among boys and those children under 11 years of age. No associations were observed between childhood difficulties and paternal PTSD among girls or those children aged 11 or older. Analyses were repeated focusing on paternal symptoms of avoidance and numbing, these paternal symptoms were associated with childhood prosocial difficulties.
Comparisons with the literature – paternal deployment to the conflicts in Iraq and Afghanistan
Prior to this study, there had been indications from US studies that paternal deployment had a negative impact on children. US studies have reported children of a deployed parent showing more emotional difficulties (as measured by the SDQ) compared with national (USA) samples and longer deployment was associated with higher levels of emotional difficulties. Parental deployment predicted school-, family- and peer-related difficulties in girls (who had particular problems during post-operation reintegration) and older youths.Reference Chandra, Lara-Cinisomo and Jaycox22 Among children of US returnees from deployment to Afghanistan or Iraq, parental distress and cumulative duration of deployment predicted depression and externalising symptoms.Reference White, de Burgh, Fear and Iversen3, Reference Lester, Peterson and Reeves6
Comparisons between the children aged 5–12 years of recently deployed US military personnel and population norms from other studies did not show significant differences in internalising or externalising symptoms or attentional difficulties, despite finding higher overall psychosocial morbidity in the deployed sample.Reference Flake, Davis, Johnson and Middleton23 This study focused on younger children compared with our broader spread of ages, was a much smaller sample at a quarter the size of our study, and included military mothers as well as fathers. There was also no direct comparison cohort of military children whose parents had not been deployed, and the parents were all recently returned from deployment. Another US study concluded that parental deployment rarely had an impact on otherwise healthy children, but did identify elevated depressive symptoms but not anxiety or behavioural difficulties in children; the authors identified boys and younger children as being more sensitive to adverse consequences of deployment.Reference Jensen, Martin and Watanabe24
In contrast to the US findings, this study in a UK military population did not find any associations between childhood emotional and behavioural symptoms and parental deployment to Iraq or Afghanistan. However, the US studies were often based on small non-representative samples. Small samples can be subject to selection and response bias resulting in greater variability around any point estimates. Our study overcomes these concerns given the large and representative sample compared with many of the previous studies. Furthermore, there are differences in deployment practice between the US and UK context, including the length of deployment being typically 6 months in the UK, and some differences in the degree of exposure to combat-related traumatic events.Reference Sundin, Herrell and Hoge25 Thus, longer and more frequent deployments experienced by US service personnel may account for the differences observed between the two nations. It should also be noted that in our study responses were collected after fathers had returned from deployment; collecting data from parents during the deployment cycle may give rise to different findings.
Our analyses (and many of those previously conducted) have focused on separation because of deployment. We are aware that families will experience other forms of separation, for example, as a result of training exercises. Deployment to a conflict zone is potentially a stressful time for families and why it has been the focus of this, and other, work.
Comparisons with the literature – paternal PTSD
Previous studies that have investigated the role of paternal PTSD on childhood well-being have yielded inconclusive and mixed results,Reference Fisher26 with common methodological issues being non-triangulated data or data being obtained from adult offspring. The few studies that have been conducted in the military context have shown paternal PTSD being associated with childhood low self-esteem, poorer family functioning and cohesion, poorer attitudes towards school, negative attitudes towards the father and increased emotional, behavioural and psychiatric disturbances.Reference Parsons, Kehle and Owen27
There is understandable concern about the combined stressors of military life and parental mental ill health upon families and child development; in a previous study 75% of veterans referred for mental health treatment reported family readjustment difficulties, 58% reported intimate partner conflicts including ‘shouting, pushing or shoving’ and 28% acknowledged that their partner was afraid of them.Reference Sayers, Farrow, Ross and Oslin28
In this current study, paternal PTSD was associated with childhood hyperactivity, and this association was more apparent in boys and younger children, whereas parental symptoms of avoidance and numbing were associated with childhood prosocial difficulties. There is already some evidence from the literature that the numbing and avoidance symptoms of PTSD are the primary reason that PTSD leads to family dysfunction, possibly as the emotional inaccessibility that this creates acts as a barrier to communication within the family.Reference Harkness, Wilson and Raphael29, Reference Davidson and Mellor30 Numbing also diminishes a fathers ability to seek out, engage in and enjoy interactions with his children, leading to a poorer father–child relationship.Reference Ruscio, Weathers, King and King31 These factors may explain the association found in this study between paternal avoidance/numbing symptoms and child prosocial difficulties.
The social domain of the SDQ refers to the ability of the child to be sensitive, reciprocal and friendly during their interactions with peers and family. Children with fathers who have PTSD are likely to miss out on positive role modelling and at the same time are exposed to negative role modelling. With a father who may be experiencing numbing and withdrawal, it is likely that children may miss out on crucial opportunities to model appropriate social behaviourReference Ramchandani, Domoney, Sethna, Psychogiou, Vlachos and Murray32, Reference Sethna, Murray, Netsi, Psychogiou and Ramchandani33 – and this is especially important for male children who may seek to emulate the behaviour of their fathers.
The influence of children's gender and age
We report an association of paternal PTSD with emotional and behavioural problems in boys alone. There may be several explanations for this. It may be that boys are more susceptible to the influence of paternal psychopathology than girls, fathers may engage differentially with boysReference Lewis and Lamb34 and boys may be more susceptible overall to a lack of engagement from fathers.Reference Sarkadi, Kristiansson, Oberklaid and Bremberg35 Literature on paternal depression suggests an association with behavioural problems in boys, but not girls in the younger age group.Reference Ramchandani and Psychogiou36, Reference Ramchandani, Stein, Evans and O'Connor37
Comparisons with the general population
Children of military fathers were more likely to demonstrate a higher frequency of emotional and behavioural problems than children in the general UK population.38 These differences were statistically significant for emotional problems (15.2 v. 11.4%), conduct problems (14.9 v. 12.7%), peer problems (14.5 v. 11.7%), prosocial difficulties (6.7 v. 2.3%) and total difficulties (13.3 v. 9.8%). Although statistically significant, the differences observed are relatively small with the exception of the least frequent outcome, prosocial difficulties. It should be noted that, being part of a military family, is likely to have a number of positive impactsReference Jain, Stevelink and Fear39 (at least one parent in stable employment) and certain facets of military family life may act as protective factors for children.
Strengths and limitations
The cohort from which this study sample is drawn is representative of the deployable UK military population and we intentionally sampled servicemen with PTSD symptoms as UK rates of PTSD among service personnel are relatively low at around 4%.Reference Hotopf, Hull and Fear11, Reference Fear, Jones and Murphy12 The sample of those who did not score highly for PTSD was representative of the total cohort.Reference Fear, Jones and Murphy12 Based on data from the UK Ministry of Defence, approximately a third of male regular service personnel have children, with those with children similarly distributed by service as studied here.40
Previous work has identified some differences in soldier-perceived and spouse-perceived ratings of children's behaviour and well-being.Reference Herzog, Everson and Whitworth41 The strengths of this study involved the use of a validated and internationally used measure of child well-being and the ability to triangulate the ratings of children's well-being by use of both maternal and paternal reports; some studies have focused on single parental reports regarding their children's behavioural and relational difficulties. Triangulation is recognised as important in differentiating between objectively recognised difficulties, and behaviours perceived as concerning or challenging by a parent with their own psychological difficulties.Reference Herzog, Everson and Whitworth41–Reference Dansby and Marinelli43 Although we primarily used maternal reports of the child's emotional and behavioural well-being, our data showed similar reporting patterns among mothers and fathers. Use of maternal reports in this way also enabled us to minimise single-reporter bias, which is a problem in much of the literature on effects of parental mental health problems on children.
The SDQ was chosen to explore childhood difficulties as it has been widely used in both national and international studies, clinically and in population studies. Parental completed questionnaires tend to underestimate emotional problems. However, the questionnaire measures used are well-validated and used widely in clinical practice and research. The use of structured clinical assessments would be advantageous in future studies; however, it was not logistically possible to clinically assess 1044 children.
The primary aim of this study was to examine the impact of paternal PTSD on child well-being within military families, something that has not been previously examined in a UK context. Although we did collect data on maternal mental health from a subset of our families, we were dependent on the father providing us with the contact details of the mother (or mothers) of their children. Permission to contact the mothers was not always provided by the fathers, and analyses determined that paternal mental health status influenced the provision of these details (data available from the authors on request). Hence, it would be inappropriate to adjust for maternal mental health on this subset of children. Further, there is a known interplay between maternal and paternal mental health, meaning that when looking at paternal mental health on child well-being, maternal health is not a true confounder.
The mental health of military mothers and interplay with their children's psychological well-being is an important topic not explored in this study, owing to the small number of military mothers in the cohort. In the UK context, women are rarely deployed in front-line roles. There is little published evidence on the impact of having a mother in the military on the well-being of children. Now that women are starting to be deployed on the front line, quantitative research on the impact upon children will be both feasible and important.
Future directions
Evidence supports the role for preventive intervention in reducing the incidence of psychological disorder in the children of parents with mental health difficulties in the general population.Reference Saxena, Jane-Llopis and Hosman44 Further, there is encouraging emergent work on interventions to improve parenting in military families where there is PTSD, for example, the Families OverComing Under Stress (FOCUS) programmeReference Lester, Saltzman and Woodward45, Reference Lester, Stein and Saltzman46 and the use of acceptance and commitment therapy combined with parenting psychoeducation, which has shown benefit on positive parenting behaviour, parenting satisfaction and psychological flexibility.Reference Casselman and Pemberton47
In conclusion, this large representative study showed that, in general, paternal deployment to the conflicts in Iraq and Afghanistan was not associated with any adverse childhood outcomes. However, this study did find that paternal PTSD was associated with hyperactivity among children overall and specifically among younger children and boys. These results highlight the importance of ensuring appropriate evidence-based interventions for military families.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1192/bjp.2017.16.
Funding
The US Department of Defense funded this work. The US Department of Defense had no influence over the work plan, data analysis or data interpretation.









eLetters
No eLetters have been published for this article.